Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1451
Revised: December 26, 2006
Accepted: January 25, 2007
Published online: March 7, 2007
Abnormalities of gastric mucosa in patients with portal hypertension are well documented. Manifestations of portal hypertension in small bowel and colon are less common. Colonic polypoid lesions microscopically consisting of a normal mucosa, with dilatation of submucosal vessels, have been described. We here report the first case of portal hypertensive duodenal polyp, responsible for gastro-intestinal bleeding. Endoscopic treatment turned out to be successful.
- Citation: Zeitoun JD, Chryssostalis A, Terris B, Prat F, Gaudric M, Chaussade S. Portal hypertensive duodenal polyp: A case report. World J Gastroenterol 2007; 13(9): 1451-1452
- URL: https://www.wjgnet.com/1007-9327/full/v13/i9/1451.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i9.1451
Esophagogastric varices are common manifestations of portal hypertension, but other lesions such as gastric mucosal changes, called portal hypertensive gastropathy[1], or colonic mucosal abnormalities[2,3] may occur. Duodenopathy has also been reported, with various forms[4-6] but never under the appearance of a polyp. We describe a patient who was found to have a portal hypertensive duodenal polyp, responsible for gastro-intestinal bleeding. Endoscopic treatment was performed with success.
A 70-year old man, with alcoholic cirrhosis, was hospitalized for a melena. Physical examination found superficial venous engorgement of the abdominal wall, with ascitis. Laboratory data revealed anemia and liver dysfunction. International normalized ratio (INR) value was 1.33.
An upper endoscopy showed large esophageal varices without red spots, and portal hypertensive gastropathy. In the descending portion of the duodenum, a 3-cm long, ulcerated and haemorrhagic polypoid lesion was seen (Figure 1).
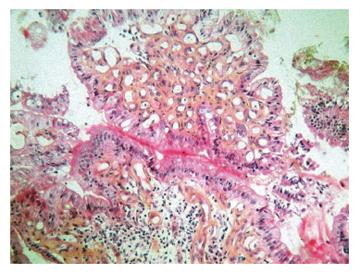
We performed polypectomy using hemostatic clips on the pedicle, then a polypectomy snare. Anatomopathologic examination of the specimen showed a fibrous and inflammatory polyp, with numerous thick-walled capillaries in its subepithelial portion, and a few vascular ectasias were associated (Figure 2). This histological appearance was considered as portal hypertensive duodenopathy. There was no epithelial proliferation in favor of an inverted polyp or hamartomatous lesion.
No complication occurred, and control endoscopy was performed three days later. The duodenal mucosa appeared normal. Colonoscopy revealed an 8-mm polyp located in the left portion of the colon, which was removed with a polypectomy snare. Anemia resolved and the patient was still free of haemorrhagic recurrence six months later.
McCormack et al[1] first described portal hypertensive gastropathy, its appearance consists of mosaic pattern, cherry red spots and scarlatina rash. Other entities have then been documented, such as portal hypertensive enteropathy[4-10] and colonopathy[2,3].
Duodenum can thus be involved and with the exception of varices, lesions reported are erythema, scattered petechiae, friable mucosa, erosion, ulcer and edema.
In our patient, portal hypertensive duodenopathy took the unusual presentation of a polyp. Misra et al[11] and Ryushi Shudo et al[4] reported that the predominant pathological features of portal hypertension duodenopathy (PHD) are subepithelial edema, and increase of diameter and wall thickness of the capillaries. Now, numerous capillaries with a thickening wall were found in our specimen, suggesting that the polyp is due to portal hypertension duodenopathy. On the other hand, colonic polypoid lesions due to portal hypertensive colonopathy have already been described[12].
Moreover, many authors insist on the uncertain clinical significance of portal hypertensive enteropathy[13], in particular whether it can be responsible for gastro-intestinal bleeding.
In the reported case, the only haemorrhagic lesion was the duodenal polyp. Additionally, anemia resolved after polypectomy. This illustrates that portal hypertension duodenopathy is a potential aetiology of gastro-intestinal bleeding.
We removed the polyp using hemostatic clips before applying polypectomy snare, to avoid the potential risk of post polypectomy hemorrhage. Polypectomy appeared to be a safe procedure and allowed histological diagnosis.
In conclusion, we report the case of a cirrhotic patient who had upper gastro-intestinal haemorrhage due to a portal hypertensive duodenal polyp. To our knowledge, this is the first case of this form of portal hypertensive duodenopathy. Endoscopic treatment was performed successfully. Although the new data suggest that portal hypertensive enteropathy may present as a source of bleeding, its exact clinical significance has to be defined subsequently.
S- Editor Liu Y L- Editor Wang XL E- Editor Zhou T
| 1. | McCormack TT, Sims J, Eyre-Brook I, Kennedy H, Goepel J, Johnson AG, Triger DR. Gastric lesions in portal hypertension: inflammatory gastritis or congestive gastropathy? Gut. 1985;26:1226-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 380] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 2. | Kozarek RA, Botoman VA, Bredfeldt JE, Roach JM, Patterson DJ, Ball TJ. Portal colopathy: prospective study of colonoscopy in patients with portal hypertension. Gastroenterology. 1991;101:1192-1197. [PubMed] |
| 3. | Bini EJ, Lascarides CE, Micale PL, Weinshel EH. Mucosal abnormalities of the colon in patients with portal hypertension: an endoscopic study. Gastrointest Endosc. 2000;52:511-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Gupta R, Saraswat VA, Kumar M, Naik SR, Pandey R. Frequency and factors influencing portal hypertensive gastropathy and duodenopathy in cirrhotic portal hypertension. J Gastroenterol Hepatol. 1996;11:728-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Vigneri S, Termini R, Piraino A, Scialabba A, Bovero E, Pisciotta G, Fontana N. The duodenum in liver cirrhosis: endoscopic, morphological and clinical findings. Endoscopy. 1991;23:210-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Shudo R, Yazaki Y, Sakurai S, Uenishi H, Yamada H, Sugawara K. Duodenal erosions, a common and distinctive feature of portal hypertensive duodenopathy. Am J Gastroenterol. 2002;97:867-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Nagral AS, Joshi AS, Bhatia SJ, Abraham P, Mistry FP, Vora IM. Congestive jejunopathy in portal hypertension. Gut. 1993;34:694-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Viggiano TR, Gostout CJ. Portal hypertensive intestinal vasculopathy: a review of the clinical, endoscopic, and histopathologic features. Am J Gastroenterol. 1992;87:944-954. [PubMed] |
| 9. | De Palma GD, Rega M, Masone S, Persico F, Siciliano S, Patrone F, Matantuono L, Persico G. Mucosal abnormalities of the small bowel in patients with cirrhosis and portal hypertension: a capsule endoscopy study. Gastrointest Endosc. 2005;62:529-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 133] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Misra SP, Dwivedi M, Misra V, Gupta M. Ileal varices and portal hypertensive ileopathy in patients with cirrhosis and portal hypertension. Gastrointest Endosc. 2004;60:778-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Misra V, Misra SP, Dwivedi M, Gupta SC. Histomorphometric study of portal hypertensive enteropathy. Am J Clin Pathol. 1997;108:652-657. [PubMed] |
| 12. | Huang WH, Hsu CT, Chao YC. Colonic polypoid lesions: an unusual endoscopic presentation of portal hypertensive colonopathy. Gastrointest Endosc. 1999;50:283-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Cheung RC, Cooper S, Keeffe EB. Endoscopic gastrointestinal manifestations of liver disease. Gastrointest Endosc Clin N Am. 2001;11:15-44. [PubMed] |