Published online Feb 7, 2007. doi: 10.3748/wjg.v13.i5.801
Revised: December 1, 2006
Accepted: December 21, 2006
Published online: February 7, 2007
Fistula between digestive tract and airway is one of the complications after esophagectomy with lymph node dissection. A case of esophagotracheal fistula secondary to esophagitis 9 years after esophagectomy and gastric pull-up for treatment of esophageal carcinoma is described. It was successfully treated with transposition of a pedicled pectoralis major muscle flap.
- Citation: Maruyama K, Motoyama S, Okuyama M, Sato Y, Hayashi K, Minamiya Y, Ogawa JI. Esophagotracheal fistula caused by gastroesophageal reflux 9 years after esophagectomy. World J Gastroenterol 2007; 13(5): 801-803
- URL: https://www.wjgnet.com/1007-9327/full/v13/i5/801.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i5.801
The denervated stomach as an esophageal substitute recovers intraluminal acidity with time. Increased risk for acid reflux after incurs prolonged esophageal exposure to gastric acid which may lead to esophageal mucosal injury. A patient with esophagotracheal fistula caused by reflux esophagitis 9 years after esophagectomy with postoperative radiation therapy was treated with transposition of a pedicled pectoralis major muscle flap. This complication caused by esophagitis has been described.
A 59-year old man presented with a sudden onset of dyspnea and increasing cough productive of gastric contents and saliva. Significant past medical history included an esophagectomy with a reconstruction of gastric tube pulled up through the posterior mediastinum 9 years earlier for esophageal squamous cell carcinoma (pT1, pN0, pM0, pStage I), followed by irradiation (58 Gy) due to positive for malignancy of proximal surgical margin of the esophagus with histological examination. After the operation he had relapses of gastric ulcer and reflux esophagitis. There was no evidence of cancer recurrence over the follow-up period.
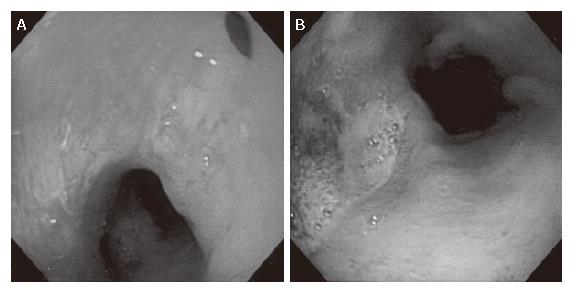
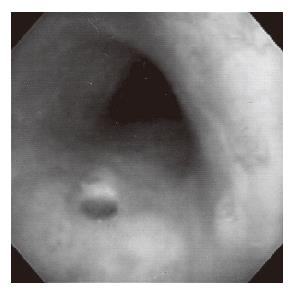
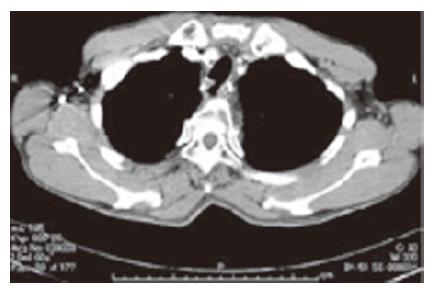
He was symptom-free except for cough after swallowing and regurgitation. None of abnormal shadows was detected in chest radiographs. Upper gastrointestinal endoscopy showed a fistula with a diameter of 5 mm on the anterior wall of the esophagus, 20 mm proximal to the esophagogastric anastomosis (Figure 1A), and a gastric ulcer just below the anastomosis (Figure 1B). No malignant feature was detected around the fistula and pathological examination of biopsy specimens from the gastric ulcer showed chronic inflammation. Bronchoscopic examination demonstrated the fistula in the membranous portion of the trachea, 90 mm distal to the vocal cord and 50 mm proximal to the bifurcation (Figure 2). Computed tomography confirmed the fistula located on a level with the upper wedge of sternum and no image of cancer recurrence (Figure 3). Twenty-four pH monitoring in the cervical esophagus was failed because of his rejection.
The patient received proton pomp inhibitors before operation with a slight improvement in his clinical symptoms, but no apparent improvement in the bronchoscopic examination. Surgery was performed 20 d after administration. A cuff of spiral endotracheal tube (8 mm in diameter) was situated below the fistula in the trachea. With the patient in the supine position, a U-shaped skin incision in the anterior cervix and median sternotomy to the 3rd rib were made. Previous radiation therapy made the procedure difficult. After lysis of adhesions, cervical esophagus and the upper portion of gastric tube were freed. Then, the common wall between esophagus and trachea was carefully dissected free in a cranial to caudal direction until the fistula was identified. No malignant changes were found macroscopically. The wall of the fistula was cut sharply, taking care to avoid tearing of the membranous portion of trachea widely. The fistula orifice in the esophageal wall was closed primarily in layers and the orifice in the trachea was also sutured primarily. The medial wedge of the left clavicle, 1st and 2nd ribs, and the left half of the sternum to the 2nd rib were excised. The left pectoralis major muscle flap was inserted and fixed between the trachea and the gastric tube. His endotracheal tube was extubated immediately after the operation. The patient’s postoperative course was uneventful. On the 16th postoperative day, feeding was started when no leak was found after a gastrograffin swallow revealed no leak. The patient was discharged on the 28th postoperative day. He had no evidence of esophagitis, gastric ulcer and fistula 9 mo after the operation.
Fistulae between digestive tract and airway are recognized as complications after esophagectomy. The digestive tracts include residual esophagus, esophagogastric anastomosis and gastric tube. Leakage from esophagogastric anastomosis can lead to localized mediastinitis and represents a possible cause of tracheoesophagogastric fistula. Gastric tube-to-airway fistula develops due to peptic ulcer, ischemia of gastric tube or airway, radiation or abscess in the mediastinum. Fistula between cervical esophagus and trachea is the rarest case in these three types of fistulae. This fistula caused by gastroesophageal reflux after esophagectomy has not been reported previously.
Peptic ulcers of pulled-up gastric tubes often cause hemorrhage, perforation and penetration[1]. Gutschow et al[2] reported that the denervated stomach as an esophageal substitute recovers a normal intraluminal acidity with time, so that more than 3 years after surgery the 24-hour pH profile in the gastric cavity of almost all patients is similar to that in healthy subjects. Shibuya[3] showed that sever esophagitis is found in 75.6% of remnant esophagus after esophagectomy for esophageal cancer. Gutschow et al[2] showed that 38.5% of patients have reflux esophagitis in the remnant esophagus for 3 years or more after esophagectomy. In our patient, endoscopic examination more than 4 years after esophagectomy revealed often severe esophagitis and gastric ulcer. Although he was treated with a proton pomp inhibitor every time, he discontinued himself taking drugs because of symptom-free. Therefore, it is strongly suggested that repetition of severe esophagitis and postoperative radiation therapy influenced formation of his fistula. In this patient, H pylori-IgG was positive. Although evaluation of his gastric emptying was not made, he often had reflux- symptom after esophagectomy.
Myocutaneous or muscle flap, because of their rich blood supply, can be used to fill the dead space after fistulectomy and add vital tissue to prevent recurrent fistulization[1,4-6]. In the part of cervical area, sternocleidomastoid muscle and pectoralis major have been used. If the esophagus and/or gastric tube cannot be preserved, continuity of the gastrointestinal tract may be reconstructed with, for example, colonic or small bowel interposition[7].
No significant relationship has been found between reflux symptoms, such as heart burn and regurgitation, and endoscopic findings after esophagectomy in the previous reports[3,8]. Patients with denervated stomach may be free from symptoms of gastric ulcer. Therefore, endoscopic examination is necessary at least once a year for early detection of ulceration and esophagitis. Fistulae between digestive tract and airway are grave complications of esophagectomy because they frequently result in respiratory failure and life-threatening conditions. If gastric ulcer or esophagitis is detected in endoscopic examination after esophagectomy, this therapy should be started immediately regardless of the interval between the examination and esophagectomy.
S- Editor Liu Y L- Editor Wang XL E- Editor Lu W
| 1. | Hayashi K, Ando N, Ozawa S, Tsujizuka K, Kitajima M, Kaneko T. Gastric tube-to-tracheal fistula closed with a latissimus dorsi myocutaneous flap. Ann Thorac Surg. 1999;68:561-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Gutschow C, Collard JM, Romagnoli R, Salizzoni M, Hölscher A. Denervated stomach as an esophageal substitute recovers intraluminal acidity with time. Ann Surg. 2001;233:509-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 79] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Shibuya S, Fukudo S, Shineha R, Miyazaki S, Miyata G, Sugawara K, Mori T, Tanabe S, Tonotsuka N, Satomi S. High incidence of reflux esophagitis observed by routine endoscopic examination after gastric pull-up esophagectomy. World J Surg. 2003;27:580-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Marty-Ané CH, Prudhome M, Fabre JM, Domergue J, Balmes M, Mary H. Tracheoesophagogastric anastomosis fistula: a rare complication of esophagectomy. Ann Thorac Surg. 1995;60:690-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Stal JM, Hanly PJ, Darling GE. Gastrobronchial fistula: an unusual complication of esophagectomy. Ann Thorac Surg. 1994;58:886-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Sakamoto K, Ogawa M, Yamamoto S, Mugita N, Saishoji T, Azuma KS, Hayashida K. Closure of a gastric tube-tracheal fistula by transposition of a pedicled sternocleidomastoid muscle flap. Surg Today. 1997;27:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Buskens CJ, Hulscher JB, Fockens P, Obertop H, van Lanschot JJ. Benign tracheo-neo-esophageal fistulas after subtotal esophagectomy. Ann Thorac Surg. 2001;72:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Yuasa N, Sasaki E, Ikeyama T, Miyake H, Nimura Y. Acid and duodenogastroesophageal reflux after esophagectomy with gastric tube reconstruction. Am J Gastroenterol. 2005;100:1021-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |