Published online Nov 14, 2007. doi: 10.3748/wjg.v13.i42.5662
Revised: September 6, 2007
Accepted: October 19, 2007
Published online: November 14, 2007
Black esophagus is a very rare disease and its pathogenesis has been unclear. Black esophagus developed concomitantly with candidiasis after diabetic ketoacidosis has not been reported yet. We report a case who developed esophageal stricture after the treatment of black esophagus and thus balloon dilatation was performed several times but failed, hence, surgical treatment was performed.
- Citation: Kim YH, Choi SY. Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroenterol 2007; 13(42): 5662-5663
- URL: https://www.wjgnet.com/1007-9327/full/v13/i42/5662.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i42.5662
Black esophagus was reported in 1990 by Goldenberg et al[1]. Black esophagus is a rare disease and defined as a dark, pigmented esophagus at endoscopy together with histologic mucosal necrosis. The etiology remains unknown, but is most likely multifactorial, even though most reports have suggested an ischemic pathogenesis[2-5]. It caused by diabetic ketoacidosis or candidiasis, but it is very rare etiology. Here, we present a case of a patient with black esophagus developed concomitantly with candidiasis after diabetic ketoacidosis.
A 34 year old male patient with the past history of type II diabetes transferred to the emergency room with drowsy mentality. His general condition was poor. He presented with arterial hypotension (60/30 mmHg), hyperglycemia (819 mg/dL), electrolyte imbalance (sodium 118 mEq/L and potassium 6.5 mEq/L), impaired renal function (BUN 194 mg/dL and creatinine 2.90 mg/dL), and an acid-base disorder known as metabolic acidosis (pH = 7.241 with low bicarbonate levels). Urine ketones were elevated (+++). The clinical picture suggested that patient had diabetic ketoacidosis.
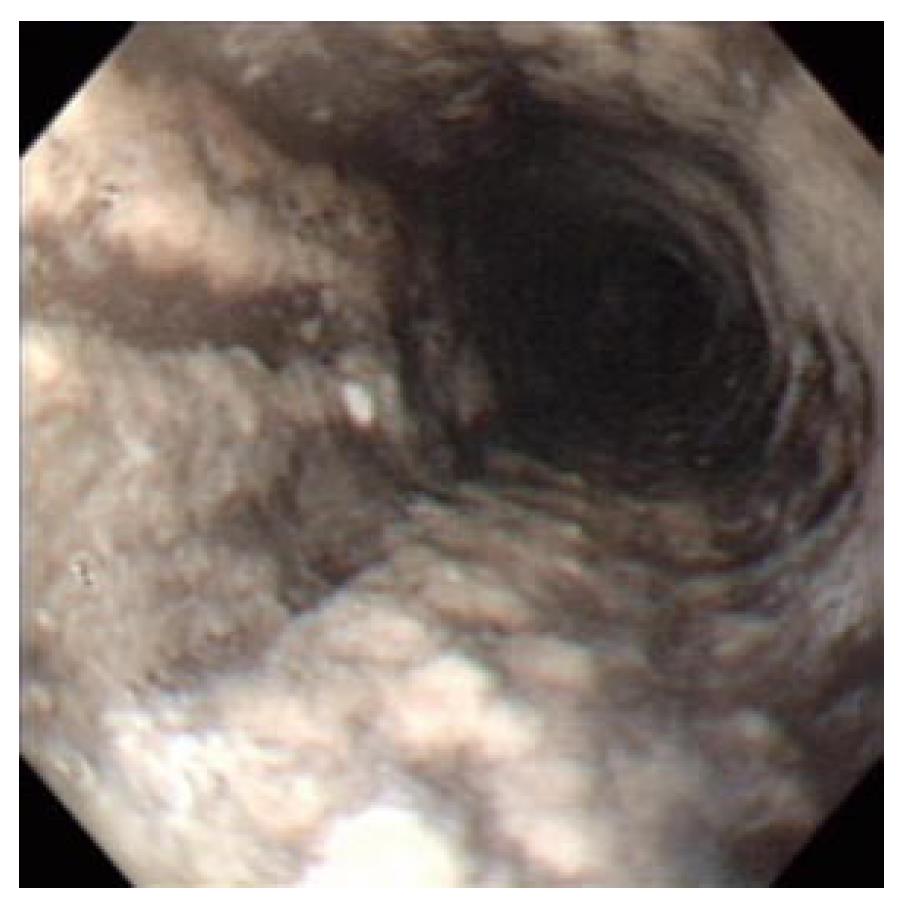
Two days after admission, hematemesis was detected, Esophago-gastro-duodenoscopy (EGD) showed black and friable mucosa from 3 to 4 cm below the cricopharyngeus to the cardia (Figure 1). Biopsies of the esophagus were not obtained at this time due to concern about possible perforation.
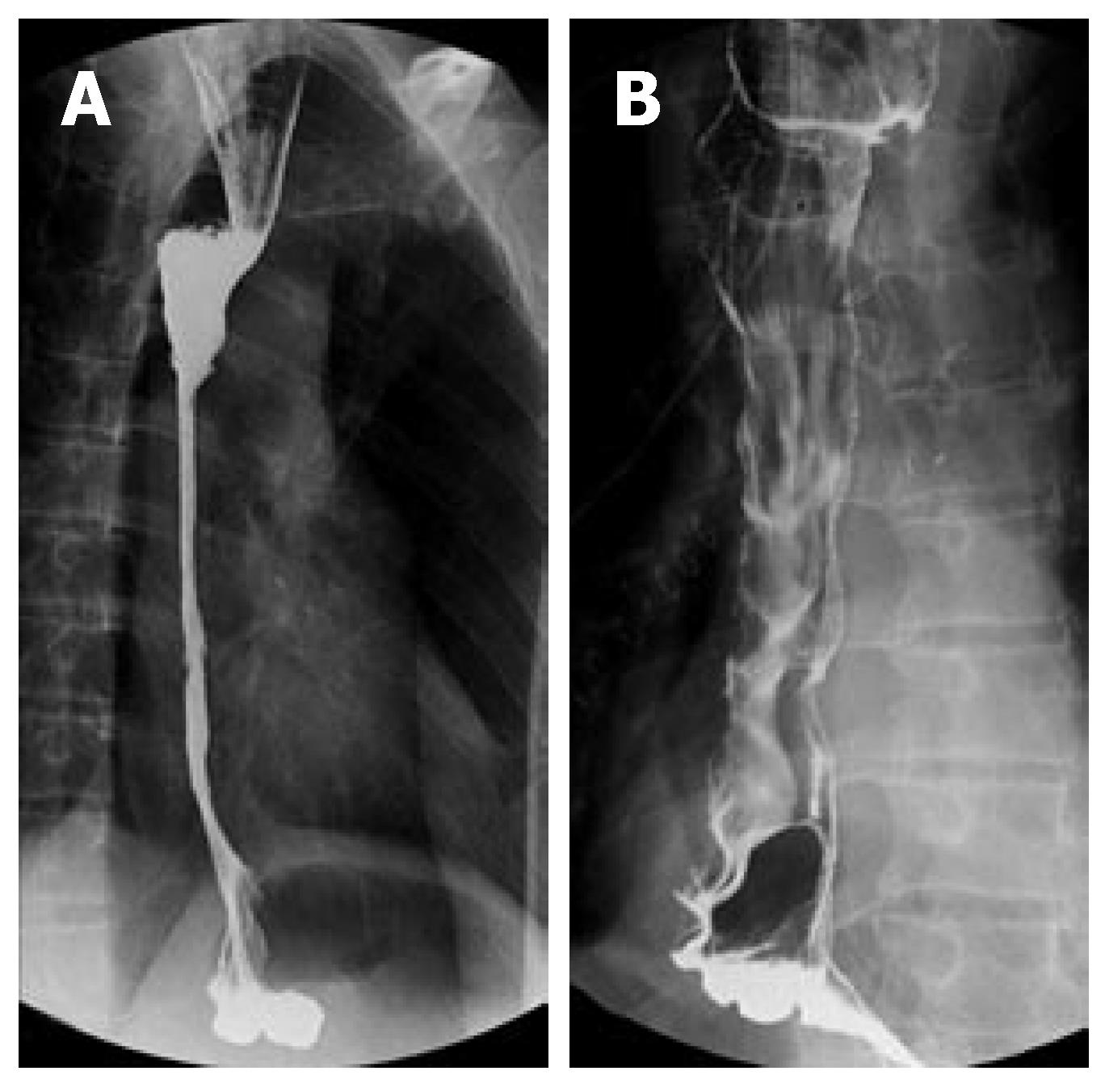
The patient gradually recovered after the conservative treatments such as intravenous proton pump inhibitor, total parenteral nutrition, oral intake restriction and antibiotics. Six days after admission, biopsies of the esophagus were obtained with EGD and revealed submucosal necrosis and candidiasis. After conservative treatments including antifungal agents (fluconazol 200 mg for seven days), the patient was discharged on the thirtieth day of admission. Subsequently, after 2 months, esophagus stricture was developed. Balloon dilation was performed 3 times during 6 months, but it was not improved (Figure 2A), and thus subtotal esophagectomy and esophagogastrostomy were performed (Figure 2B), and on the eighteenth day of surgery, he was discharged without complication.
Black esophagus was reported in 1990 by Goldenberg et al[1]. Black esophagus is a rare disease, and the incidence detected by EGD has been reported to be 0.01%-0.2%[2-5]. It is developed preferentially in the male (81%), and it has been reported to occur predominantly in the elderly[4].
The pathogenesis of black esophagus remains undefined and is probably a combination of an low systemic perfusion, gastric outlet obstruction, and malnutrition[2-5].
Several etiologies have been suggested including ischemia, lye ingestion, microbial infection related to a nasogastric tube, anticardiolipin antibody syndrome, herpes simplex esophagitis, diabetic ketoacidosis, severe vomiting, acute gastric outlet obstruction with massive gastroesophageal reflux, Lactobacillus acidophilus infection, acute caustic injury from detergent in the endoscope, antibiotics, Stevens-Johnson syndrome, and hypothermia[2,3,5]. Among 88 cases of black esophagus reported until now, cases whose etiology was diabetic ketoacidosis were 3 cases[4], cases whose etiology was fungal infection were 2 cases[5,6]; however, reports showing diabetic ketoacidosis and candidiasis concomitantly have not been reported.
Most patients are symptomatic, and the most common symptoms are upper gastrointestinal bleeding such as hematemesis, coffee-ground vomiting and melena[2-4].
The diagnosis is based on typical endoscopic appearance and on histopathological findings after the exclusion of true necrosis and ulceration. It shows the finding of the diffusely black esophageal mucosa, and in most cases it disappears suddenly in the Z-line. Histological findings of esophagus biopsy show necrotic debris, and it may show the finding of the necrotic mucosa without the viable epithelium, and occasionally, the submucosa and up to the muscularis propria, although rare, may be involved[2,4]. This case showed that submucosal involvement.
The prognosis of black esophagus is very poor, and its mortality reaches up to 31.8%-50%, although most of the deaths were caused by underlying illnesses[2-4]. Death secondary to esophageal necrosis occurs in less than 6% of cases[4]. Therapeutic modalities are not standardized, but most authors support a conservative approach by correcting the underlying disease, intravenous proton pump inhibitor, total parenteral nutrition, and oral intake restriction[2-5].
The major complications of black esophagus are esophageal stenosis and stricture formation, and they occur in 10.2%-15% of patients. Repeated dilation is required in most patients[2,4,5]. In our case, repeated dilation was not effective, and thus surgical treatment was performed. Other complications are esophageal perforation, mediastinitis and abscess formation, which occurs in approximately 6% patients[4].
Surgical treatments for black esophagus have been reported in 5 cases[4], nevertheless, all 5 cases were performed surgery for early complications such as esophageal perforation and our case is the first case of black esophagus performed surgical treatment for the late complication esophageal stricture.
S- Editor Liu Y L- Editor Rippe RA E- Editor Liu Y
| 1. | Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology. 1990;98:493-496. [PubMed] |
| 2. | Carneiro M, Lescano M, Romanello L, Módena J, Carneiro F, Ramalho L, Martinelli A, França A. Acute esophageal necrosis. Digestive Endoscopy. 2005;17:89–92. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963-2003. Dis Esophagus. 2006;19:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007;42:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 162] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 5. | Ben Soussan E, Savoye G, Hochain P, Hervé S, Antonietti M, Lemoine F, Ducrotté P. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc. 2002;56:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 93] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Hoffman M, Bash E, Berger SA, Burke M, Yust I. Fatal necrotizing esophagitis due to Penicillium chrysogenum in a patient with acquired immunodeficiency syndrome. Eur J Clin Microbiol Infect Dis. 1992;11:1158-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 1.3] [Reference Citation Analysis (0)] |