Published online Nov 7, 2007. doi: 10.3748/wjg.v13.i41.5506
Revised: August 17, 2007
Accepted: August 30, 2007
Published online: November 7, 2007
AIM: To investigate the influence of high dose of dexamethasone on inflammatory mediators and apoptosis of rats with severe acute pancreatitis (SAP).
METHODS: SAP rats were randomly assigned to the model group and treatment group while the normal rats were assigned to the sham operation group. The mortality, ascite volumes, ascites/body weight ratio and pancreas pathological changes of all rats were observed at 3, 6 and 12 h after operation. Their contents of amylase and endotoxin in plasma and contents of tumor necrosis factor (TNF-α), phospholipase A2 (PLA2) and IL-6 in serum were also determined. The microarray sections of their pancreatic tissues were prepared, terminal transferase dUTP nick end labeling (TUNEL) staining was performed and apoptotic indexes were calculated.
RESULTS: There was no marked difference between treatment group and model group in survival. The contents of amylase and endotoxin in plasma and contents of TNF-α, PLA2 and IL-6 in serum, ascite volumes, ascites/body weight ratio and pancreas pathological scores were all lower in treatment group than in model group to different extents at different time points [P < 0.05, 58.3 (26.4) ng/L vs 77.535 (42.157) ng/L in TNF-α content, 8.00 (2.00) points vs 9.00 (2.00) points in pathological score of pancreas respectively; P < 0.01, 0.042 (0.018) EU/mL vs 0.056 (0.0195) EU/mL in endotoxin content, 7791 (1863) U/L vs 9195 (1298) U/L in plasma amylase content, 1.53 (0.79) vs 2.38 (1.10) in ascites/body weight ratio, 8.00 (1.00) points vs 11.00 (1.50) points in pathological score of pancreas; P < 0.001, 3.36 (1.56) ng/L vs 5.65 (1.08) ng/L in IL-6 content, 4.50 (2.00) vs 7.20 (2.00), 4.20 (1.60) vs 6.40 (2.30), 3.40 (2.70) vs 7.90 (1.70) in ascite volumes, respectively]. The apoptotic indexes of pancreas head and pancreas tail were all higher in treatment group than in model group at 6 h [P < 0.01, 0.00 (2.00)% vs 0.00 (0.00)%, 0.20 (1.80) vs 0.00 (0.00) in apoptosis indexes, respectively].
CONCLUSION: The mechanism of dexamethasone treatment in acute pancreatitis is related to its inhibition of inflammatory mediator generation and induction of pancreatic acinar cell apoptosis.
- Citation: Zhang XP, Chen L, Hu QF, Tian H, Xu RJ, Wang ZW, Wang KY, Cheng QH, Yan W, Li Y, Li QY, He Q, Wang F. Effects of large dose of dexamethasone on inflammatory mediators and pancreatic cell apoptosis of rats with severe acute pancreatitis. World J Gastroenterol 2007; 13(41): 5506-5511
- URL: https://www.wjgnet.com/1007-9327/full/v13/i41/5506.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i41.5506
The pathogenesis of severe acute pancreatitis (SAP) is closely related to the factors such as activation of pancreatin, release of inflammatory mediators, microcirculation disturbance and apoptosis. The sound therapeutic effects of large dose of dexamethasone on SAP have been demonstrated. In this experiment, the mechanism of large dose of dexamethasone in SAP was discussed and the changes of inflammatory mediator content and pancreatic acinar cell apoptosis after dexamethasone treatment for SAP rats were observed. The tissue microarray has also been applied to the pathohistological examination of pancreatitis to improve the study efficiency.
Clean grade healthy male Sprague-Dawley (SD) rats with body weight of 250-300 g were purchased from the Experimental Animal Center of Medical School, Zhejiang University. Sodium taurocholate and pentobarbital were purchased from USA Sigma Company, and dexamethasone injection from Zhejiang Xinchang Pharmaceutical Company, China. The full automatic biochemical analyzer was used to determine the plasma amylase level (U/L). Plasma endotoxin tachypleus amebocyte lysate kit was purchased from Shanghai Yihua Medical Science and Technology Corporation (Institute of Medical Analysis, Shanghai, China), the calculation unit is EU/mL. The TNF-α ELISA kit was purchased from Jingmei Bioengineering Corporation, the calculation unit is pg/mL (ng/L). The serum secretory phospholipase A2 enzyme assay ELA kit (PLA2) was purchased from R&D System Institute and the calculation unit is U/mL. The above determinations were all operated according to the instructions of the kits.
Ninety clean grade healthy male SD rats were prepared into SAP models by the improved Aho's method and randomly divided into the model group (45 rats) and treatment group (45 rats). Another 45 were assigned into the sham operation group. The above groups were then randomly divided into the 3, 6 and 12 h group with 15 rats in each. The treatment group was injected with dexamethasone via vena caudalis, 0.5 mg/100 g body weight, 15 min after successful preparation of SAP model. In the sham operation group, pancreas and duodenum were turned over before the abdomen was closed. The sham operation group and model group were injected with the saline of the same volume via vena caudalis 15 min after the operation[1]. SAP model was established according to the reference[1].
The rat mortality was determined at 3, 6 and 12 h after operation and the survival rate was calculated at different time points.
After the rats were anesthetized by sodium pentobarbital and killed in batches, the pancreas samples were collected. Fix them according to the related requirements, observe the pathological changes of pancreas after HE staining and compare the pathological scores among groups. The standard of pancreas pathological score was in accordance with reference[2]. The content of amylase, endotoxin in plasma, and TNF-α, IL-6 and PLA2 in serum of all groups were determined at different time points.
The tissue microarray was applied to prepare the tissue microarray sections of pancreas, which were stained by DNA, and terminal transferase dUTP nick end labeling (TUNEL). The observation of pancreatic cells and calcula-tion of apoptotic indexes were carried out respectively.
The statistical analysis was conducted with the SPSS11.5 software. The Kruskal-Wallis test or variance analysis (only applied to PLA2) was performed for the comparison among the three groups. The Bonfferoni test was also applied to the comparison. There are statistical significances when P < 0.05.
The mortality of model group was 0% (0/15), 0% (0/15) and 13.33% (2/15) at 3, 6 and 12 h, respectively. The sham operation group and dexamethasone treated group survived at all time points while there was no marked difference between the model group and dexamethasone treated group (P > 0.05)[1].
The model group and treated group had significantly higher ascite columes than sham operation group (P < 0.001), while the treatment group had significantly lower ascite volume than the model group (P < 0.001) (Table 1).
The model group and treatment group had significantly higher ascites/body weight ratio than sham operation group (P < 0.001), while the treatment group had significantly lower ratio than the model group at 3 h (P < 0.01), and the treatment group had significantly lower ratio than the model group at 6 and 12 h (P < 0.001) (Table 2).
The plasma amylase content in model group and dexamethasone treated group was significantly higher than in the sham operation group at all time points (P < 0.001). There was no marked difference between the dexamethasone treated group and model group at 3 and 6 h (P > 0.05). The plasma amylase content in the dexamethasone treated group was significantly less than in the model group at 12 h (P < 0.01) (Table 3).
| Index | Sham operation group | Model group | Dexamethasone treated group | ||||||
| 3 h | 6 h | 12 h | 3 h | 6 h | 12 h | 3 h | 6 h | 12 h | |
| Amylase | 2038 | 2117 | 1725 | 7423 | 8149 | 9195 | 6739 | 7839 | 7791b |
| (U/L) | (346) | (324) | (434) | (2275) | (1540) | (1298) | (2310) | (2258) | (1863) |
| Endotoxin | 0.015 | 0.015 | 0.016 | 0.035 | 0.055 | 0.056 | 0.03 | 0.040b | 0.042b |
| (EU/mL) | (0.007) | (0.007) | (0.005) | (0.017) | (0.025) | (0.0195) | (0.014) | (0.012) | (0.018) |
| TNF-α | 3.3 | 4.9 | 3.7 | 46.125 | 77.535 | 67.301 | 38.4 | 58.3a | 38.7a |
| (ng/L) | (3.6) | (2.6) | (2.3) | (37.954) | (42.157) | (32.1315) | (26.6) | (26.4) | (28.5) |
| IL-6 | 1.75 | 1.75 | 1.48 | 4.87 | 6.65 | 5.65 | 3.31b | 3.17b | 3.36b |
| (ng/L) | (0.65) | (1.04) | (0.57) | (1.38) | (1.45) | (1.08) | (1.38) | (1.28) | (1.56) |
The plasma endotoxin content in the model group and dexamethasone treated group was significantly higher than in the sham operation group at all time points (P < 0.001). No marked difference was found between the dexamethasone treated group and model group at 3 h (P > 0.05). The content in dexamethasone treated group was significantly less than in the model group at 6 and 12 h (P < 0.01) (Table 3).
The model group and dexamethasone treated group had significantly higher serum TNF-α content than the sham operation group at all time points (P < 0.001). No marked difference was noticed between the dexamethasone treated group and model group at 3 h (P > 0.05). The dexamethasone treated group had significantly less serum TNF-α content than the model group at 6 and 12 h (P < 0.05)[1] (Table 3).
The serum IL-6 contents of model group and treatment group were significantly higher than those of sham operation group (P < 0.001); the content of treatment group was significantly lower than that of model group at 3 h (P < 0.01); and the contents of treatment group were significantly lower than those of model group at 6 and 12 h (P < 0.001) (Table 3).
The model group and dexamethasone treated group significantly higher serum PLA2 content than the sham operation group at all time points (P < 0.001). The content in the dexamethasone treated group was significantly less than in the model group (P < 0.001) (Table 4).
HE staining was performed and the pathohistological score standard was referred to the improved Schmidt score. Two chief pathologists used the blind method for scoring[2].
Gross pathological changes of pancreas. (1) Sham operation group: No apparent abnormality of pancreas and peripancreatic epiploon at all time points. (2) Model group: The gross pathological change of pancreas tail was more apparent than that of pancreas head. The severity of overall pathological change increased with time after modeling. At 3 h, a small amount of hemorrhagic ascites was observed by naked eyes with relatively apparent changes of pancreas hyperemia and edema, hemorrhage and necrosis; at 6 and 12 h, hemorrhagic ascites increased more apparently with edema, hemorrhage and necrosis, and more saponified spots could be seen on peripancreatic epiploon and peritoneum. (3) Treatment group: At 3 h, the degree of pancreas hyperemia and edema, hemorrhage and necrosis was milder than that of model group with decrease of ascitic fluid; at 6 and 12 h, the pancreatic hemorrhage and necrosis area and degree were milder than those of model group with apparent decrease of ascitic fluid.
The pancreas pathological changes under light microscope. (1) Sham operation group: Mild interstitial edema occurred in a few cases, and neutrophil infiltration was occasional. No acinar cell, fat necrosis and hemorrhage were observed. (2) Model group: The pathological change severity increased with time after modeling. At 3 h, pancreas interstitial hyperemia, edema, a small amount of inflammatory cell infiltration, focal necrosis and interstitial hemorrhage occurred, among which some were lamellar hemorrhage and necrosis. At 6 h, interstitial edema, hemorrhage, inflammatory cell infiltration, focal and lamellar hemorrhage and necrosis occurred. At 12 h, large area of hemorrhage and necrosis, lobule outline damage and a large amount of inflammatory cell infiltration were found. (3) Treatment group: The pathological change scope and degree of most cases were milder than those of model group at corresponding time points. Only a few had lamellar hemorrhage and necrosis, but the scope of hemorrhage and necrosis decreased and inflammatory cell infiltration apparently alleviated.
Both model group and dexamethasone group had significantly higher pathological score of pancreas than the sham operation group at different time points (P < 0.01) while that in dexamethasone group was significantly less than in the model group at 3 and 6 h (P < 0.05), and it was also significantly less in the dexamethasone group than in the model group at 12 h (P < 0.01) (Table 5).
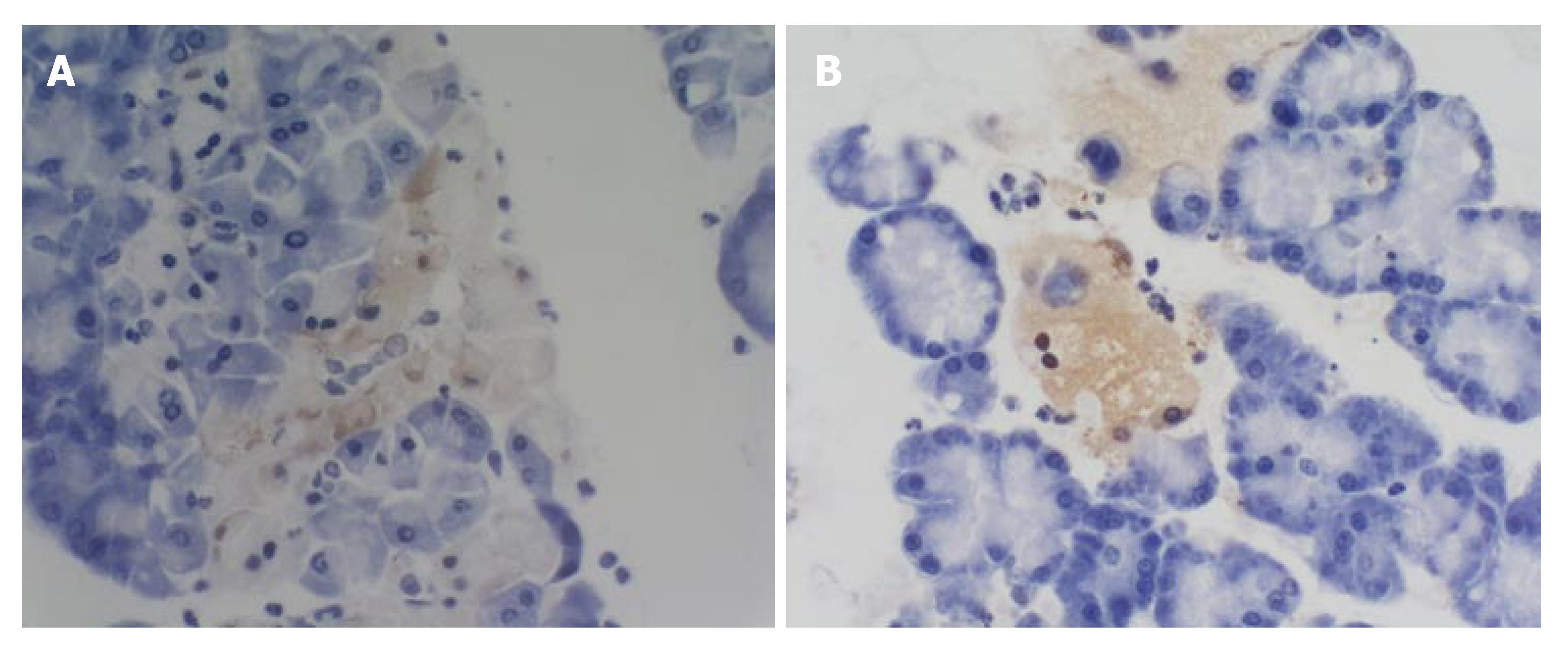
The apoptosis index of pancreas head and tail at 3 and 12 h was not significantly different among all groups (P > 0.05). No marked difference was found between the model group and sham operation group at different time points (P > 0.05). At 6 h, the apoptosis index of pancreas in the treatment group was significantly higher in the model group and sham operation group (P < 0.01) (Table 6, Figure 1A and B).
| Group (t/h) | Pancreas head | Pancreas tail | ||||
| 3 h | 6 h | 12 h | 3 h | 6 h | 12 h | |
| Sham operation group | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Model group | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Dexamethasone treated group | 0.00 (0.00) | 0.00 (2.00)b | 0.00 (0.00) | 0.00 (0.00) | 0.20 (1.80)b | 0.00 (0.00) |
There was a positive correlation between amylase and PLA2 of model group at 3 h (P < 0.05); the TNF-α content of treatment group was positively correlated with PLA2 at 6 h (P < 0.05). There was a positive correlation between pancreas pathological score and TNF-α (P < 0.05).
Under normal circumstances, the inflammatory mediators are at low level of dynamic balance to maintain the stability of the internal environment. Excessive inflammatory reaction plays a vital role in SAP pathogenesis[3-6]. In this experiment, the influence of dexamethasone on inflammatory mediators in treatment of SAP rats was studied and its relationship with the apoptosis of pancreatic acinar cells was discussed.
TNF-α can increase the local tissue damage and capillary permeability, eventually aggravating pancreatic necrosis, which is important in AP[7,8]. Norman et al[7] found in SAP rats a positive correlation between the TNF-α concentrations in pancreatic tissue and plasma and the level of pancreatic injury and inflammation, which is consistent to the fact that in this experiment, the pancreas pathological score was positively correlated with TNF-α at 12 h in model group (P < 0.05). It was found in this experiment that the serum TNF-α contents were lower in treatment group than in model group at 6 and 12 h (P < 0.05), demonstrating that dexamethasone plays a certain role in inhibiting serum TNF-α content. Since PLA2 plays an important role in SAP onset[8-10], PLA2 antagonist can significantly improve the pathological injury of pancreas of the animal model with pancreatic injury[11,12]. In this study, the serum PLA2 content was lower in treatment group than in model group (P < 0.001), demonstrating a significant inhibiting effect of dexamethasone on PLA2 or its generation. IL-6, mainly generated by monocyte/macrophage, T cell, B cell, etc, participates in many acute body reactions such as burn, sepsis and major operation. The positive correlation between serum IL-6 level and AP severity has been proved by many studies[13]. And the histological score of pancreas can be significantly improved by lowering IL-6. The serum IL-6 contents were all lower in treatment group than in model group to different extents (P < 0.01 or P < 0.001), demonstrating that dexamethasone can inhibit serum IL-6 content.
In recent years, it was found that both inflammatory mediators and pancreatic acinar cell apoptosis are related to AP[14,15]. Apoptosis participates in AP onset[16]. The apoptosis of pancreatic acinar cell might be a reaction beneficial to the body after the occurrence of pancreatitis[17,18]. Both necrosis and apoptosis are death modes of injured cells[19]. However, substantially different from necrosis, apoptosis will not release the harmful substance in lysosome or cause intense inflammatory reaction[20]. Necrosis prevails in SAP. The illness can be alleviated by apoptosis induction and aggravated by apoptosis inhibition[14]. In this experiment, according to the result of TUNEL staining, the apoptotic index was higher in treatment group than in model group (P < 0.01), and the pathological score was lower in treatment group than in model group (P < 0.05) at 6 h, demonstrating that dexamethasone can promote the apoptosis of pancreatic cells and protect pancreatic tissue.
The effect of glucocorticoid (represented by dexamethasone) on AP/SAP has been an issue in dispute. In 1952, Stephensen et al[21] for the first time reported the effect of glucocorticoid in AP treatment. Many empirical studies show glucocorticoid can improve the survival of AP animals[22,23] Its mechanisms mainly are: inhibiting the generation of inflammatory mediators and (or) inhibiting the effects of inflammatory mediators, enhancing body stress, improving microcirculation, alleviating endotoxemia, cleaning free radicals, inhibiting nitric oxide (NO) and expression of NF-κB, etc[22,24,25]. In terms of administration and dose, Dong et al[26,27] found a large dose of dexamethasone was obviously superior to the small dose dexamethasone in therapeutic effect and early use of dexamethasone was superior to dexamethasone of the same dose 5 h later. We used large doses of dexamethasone and achieved relatively sound therapeutic effects, obviously alleviating pathological changes of pancreas.
This empirical study used the improved Aho's method[28] to prepare SAP model, the rat survival of the dexamethasone treated group was significantly higher than that of the model group, but there was no marked difference between the two groups (P > 0.05). However, no matter gross or under light microscope, the treatment group has milder pancreatic tissue cell inflammatory pathological changes, less ascitic fluid and hemorrhage, and lower necrosis scope than the model group at all time points.
The contents of amylase and endotoxin in plasma and TNF-α, PLA2 and IL-6 in serum were all lower in dexamethasone treated group than in model group. The apoptotic index was higher in treatment group than in model group while the inflammation, hemorrhage and necrosis of pancreas were all milder in treatment group than in model group, indicating that dexamethasone can improve the pancreatic injury of SAP rats by directly inducing pancreatic cell apoptosis, or indirectly inducing apoptosis through inhibition of excessive rise of TNF-α, IL-6, PLA2, etc. In this experiment, no relation has been found between inflammatory mediators and pancreas apoptotic index. However, it has been found in many studies that the inflammatory mediators released by injured cells in AP can influence apoptosis. The role of inflammatory mediators that indirectly regulate apoptotic gene is significant and non-neglectable during its participation in apoptosis. It is worth mentioning that there are various but one influential factors act together to result in apoptosis during AP, presenting a network relation structure[29].
We used the tissue microarray section maker (Beecher Instruments, USA) to drill a hole 2.0 mm in diameter on recipient block and combined TUNEL staining method to examine the apoptotic index. The results indicate that the tissue chip 2.0 mm in diameter can achieve reliable experimental result, which is representative, time, energy and reagent saving, and convenient for control.
The severe acute pancreatitis (SAP) is one of the common acute abdomens in clinical practice. The pathogenesis of SAP is closely related to factors such as activation of pancreatin, release of inflammatory mediators, microcirculation disturbance and apoptosis. The recent studies prove the apoptosis could be a beneficial reaction to AP. The apoptosis of acinar cell in pancreas inducing injury can alleviate the inflammatory reaction. In this experiment, the mechanism of dexamethasone treatment in SAP was discussed and the changes of inflammatory mediator content and pancreatic acinar cell apoptosis were observed.
To discuss the influence of dexamethasone on inflammatory mediators and apoptosis of rats with SAP, the authors established the rat SAP models and combined the tissue microarrays to observe the influence of dexamethasone on apoptosis of acinar cell in pancreas, providing a new theoretical basis for dexamethasone treatment of SAP and application of tissue microarrays in pancreatitis pathological examinations.
The tissue microarray has been applied to the pathohistological examination of pancreatitis to improve the study efficiency.
The sound therapeutic effects of a large dose of dexamethasone on SAP have been demonstrated. It is of some value to apply tissue microarrays to pathological examination and analysis of non-tumor diseases like pancreatitis.
The apoptosis is a kind of self-protecting fashion namely the body starts the autogene program under certain pathological and physiological conditions and removes the irreparable cells, which is substantially different from necrosis. Tissue microarray (TMA), or tissue chip, is a method of harvesting small disks (diameter 0.6-2.0 mm) of tissue from a range of standard histologic sections and placing in an array on a recipient paraffin block by which hundreds of cases can be analyzed simultaneously. This technique allows maximization of tissue resources by analysis of small-core biopsies of blocks, rather than complete sections.
Through animal studies, the authors investigated the influence of dexamethasone on inflammatory mediators and apoptosis of rats with severe acute pancreatitis. They concluded that the mechanism of dexamethasone treatment in acute pancreatitis is related to its inhibition of inflammatory mediator generation and induction of pancreatic acinar cell apoptosis.
S- Editor Zhu LH L- Editor Ma JY E- Editor Liu Y
| 1. | Zhang XP, Zhang L, Chen LJ, Cheng QH, Wang JM, Cai W, Shen HP, Cai J. Influence of dexamethasone on inflammatory mediators and NF-kappaB expression in multiple organs of rats with severe acute pancreatitis. World J Gastroenterol. 2007;13:548-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Zhang XP, Zhang L, Yang P, Zhang RP, Cheng QH. Protective effects of baicalin and octreotide on multiple organ injury in severe acute pancreatitis. Dig Dis Sci. 2008;53:581-591. [PubMed] |
| 3. | Wang ZF, Pan CE, Liu SG. The role of inflammatory mediators in acute pancreatitis. Shijie Huaren Xiaohua Zazhi. 1998;6:170-171. |
| 4. | Gu J, Li N. Acute pancreatitis and SIRS. Gandan Waike Zazhi. 2004;12:149-152. |
| 5. | Dugernier TL, Laterre PF, Wittebole X, Roeseler J, Latinne D, Reynaert MS, Pugin J. Compartmentalization of the inflammatory response during acute pancreatitis: correlation with local and systemic complications. Am J Respir Crit Care Med. 2003;168:148-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Bentrem DJ, Joehl RJ. Pancreas: healing response in critical illness. Crit Care Med. 2003;31:S582-S589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Yang J, Murphy C, Denham W, Botchkina G, Tracey KJ, Norman J. Evidence of a central role for p38 map kinase induction of tumor necrosis factor alpha in pancreatitis-associated pulmonary injury. Surgery. 1999;126:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Kerekes L, Antal-Szalmás P, Dezso B, Sipka S, Furka A, Mikó I, Sápy P. In vitro examination of the influence of lipase and amylase on dog's pancreas tissue incubated with endotoxins, phospholipase A2 or cytokines. Magy Seb. 2005;58:120-124. [PubMed] |
| 9. | Norman JG, Fink GW, Franz MG. Acute pancreatitis induces intrapancreatic tumor necrosis factor gene expression. Arch Surg. 1995;130:966-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 149] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Friess H, Shrikhande S, Riesle E, Kashiwagi M, Baczako K, Zimmermann A, Uhl W, Büchler MW. Phospholipase A2 isoforms in acute pancreatitis. Ann Surg. 2001;233:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Caronna R, Diana L, Nofroni I, Sibio S, Catinelli S, Sammartino P, Chirletti P. Effects of gabexate mesilate (FOY) on amylase and phospholipase A2 in human serum and pancreatic juice. Dig Dis Sci. 2005;50:868-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Caronna R, Loretta D, Campedelli P, Catinelli S, Nofroni I, Sibio S, Sinibaldi G, Chirletti P. Gabexate mesilate (FOY) inhibition of amylase and phospholipase A(2) activity in sow pancreatic juice. J Invest Surg. 2003;16:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Bhatia M. Novel therapeutic targets for acute pancreatitis and associated multiple organ dysfunction syndrome. Curr Drug Targets Inflamm Allergy. 2002;1:343-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 89] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Kaiser AM, Saluja AK, Lu L, Yamanaka K, Yamaguchi Y, Steer ML. Effects of cycloheximide on pancreatic endonuclease activity, apoptosis, and severity of acute pancreatitis. Am J Physiol. 1996;271:C982-C993. [PubMed] |
| 15. | Bhatia M. Apoptosis of pancreatic acinar cells in acute pancreatitis: is it good or bad? J Cell Mol Med. 2004;8:402-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Wu ZJ, Zhang YD, Lei ZM, Yu SH. Discuss apoptosis in pathogenesis of rat acute pancreatitis. Zhongguo Xiandai Yixue Zazhi. 2003;13:13-15. |
| 17. | Yasuda T, Takeyama Y, Ueda T, Shinzeki M, Sawa H, Nakajima T, Kuroda Y. Breakdown of intestinal mucosa via accelerated apoptosis increases intestinal permeability in experimental severe acute pancreatitis. J Surg Res. 2006;135:18-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Chen HM, Hsu JT, Chen JC, Ng CJ, Chiu DF, Chen MF. Delayed neutrophil apoptosis attenuated by melatonin in human acute pancreatitis. Pancreas. 2005;31:360-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | McHugh P, Turina M. Apoptosis and necrosis: a review for surgeons. Surg Infect (Larchmt). 2006;7:53-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Samuilov VD, Oleskin AV, Lagunova EM. Programmed cell death. Biochemistry (Mosc). 2000;65:873-887. [PubMed] |
| 21. | Stephenson HE, Pfeffer RB, Saypol GM. Acute hemorrhagic pancreatitis; report of a case with cortisone treatment. AMA Arch Surg. 1952;65:307-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Sugiyama Y, Kato S, Abe M, Mitsufuji S, Takeuchi K. Different effects of dexamethasone and the nitric oxide synthase inhibitor L-NAME on caerulein-induced rat acute pancreatitis, depending on the severity. Inflammopharmacology. 2005;13:291-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Paszt A, Takács T, Rakonczay Z, Kaszaki J, Wolfard A, Tiszlavicz L, Lázár G, Duda E, Szentpáli K, Czakó L. The role of the glucocorticoid-dependent mechanism in the progression of sodium taurocholate-induced acute pancreatitis in the rat. Pancreas. 2004;29:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Wang ZF, Pan CE, Lu Y, Liu SG, Zhang GJ, Zhang XB. The role of inflammatory mediators in severe acute pancreatitis and regulation of glucocorticoids. Hepatobiliary Pancreat Dis Int. 2003;2:458-462. [PubMed] |
| 25. | Liu JS, Wei XG, Fu J, Liu J, Yuan YZ, Wu YL. Stady of the relationship among endothelin,nitric oxide,oxgen free radical and acute pancreatitis. Zhongguo Yishi Zazhi. 2003;5:28-29. |
| 26. | Dong R, Wang ZF, LV Y, Ma QJ. Treatment of severe acute pancreatitis with large dosage of dexamethsone in the earlier time. Gandan Waike Zazhi. 2005;13:58-60. |
| 27. | Dong R, Wang ZF, Lu Y, Pan CE. Empirical study on severe acute pancreatitis treated by large dose of dexamethasone. Zhonghua Putong Waike Zahi. 2001;10:314-317. |
| 28. | Aho HJ. Experimental pancreatitis in the rats: sodium taurocholate-induced acute hemorrhagic pancreatitis. Scand J Gastroenterol. 1980;15:411-416. |
| 29. | Zhang XP, Lin Q. Advancement of study on the relationship between mediators of inflammation and apoptosis in acute pancreatitis. Shijie Huaren Xiaohua Zazhi. 2005;13:2773-2777. |