INTRODUCTION
Recurrence and metastasis are the major obstacles to further improve the prognosis of hepatocellular carcinoma (HCC). Tumor recurrence is common after hepatic resection of huge HCC greater than 10 cm in diameter. The overall 1- and 3-year survival rates are 66% and 44%, respectively. The overall 5-year survival ranges from 11% to 76%, with a median around 30% after hepatectomy[1]. Extrahepatic recurrence occurs in 30% of the patients. Resection of isolated extrahepatic HCC metastasis has been advocated to obtain a possibility of long-term survival[2,3]. Accurate re-staging plays the most important role in making a decision on extrahepatic metastasis resection. Nowadays, PET/CT is more and more widely available, and its application with 18F-FDG in oncology has become one of the standard imaging modalities in diagnosing, staging and re-staging HCC[4]. We present here a patient with huge HCC resected six years ago and a new omental lymph node metastasis recently identified by 18 F-FDG PET/CT. Long-term survival was achieved in this patient after resection of the omental lymph node metastasis.
CASE REPORT
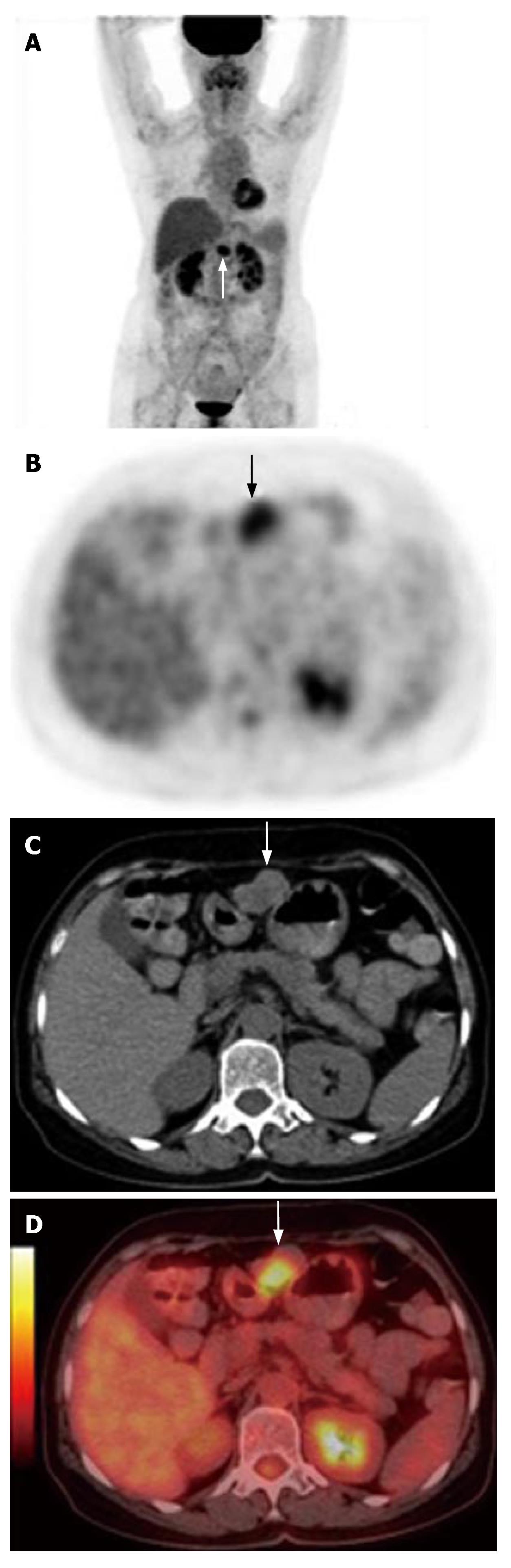
A 60-year old woman with a medical history of HBV infection and no cirrhosis was referred to our hospital for a liver tumor found by coincidence. The AFP level was 13.4 ng/mL. HCC was suspected (Figure 1) and a left hemihepatectomy was performed in December 2000. Histology showed a HCC (Edmondson-Steiner's gradeI) with a diameter of 13.0 cm with central necrosis. No microscopic vascular invasion was found. After partial liver resection, AFP values returned to normal. The patient accepted trancatheter arterial chemo-embolization (TACE) treatment 1 mo after hepatectomy and no special change was found during angiography. After 78 mo of follow-up, her AFP increased to 597.8 ng/mL. Conventional chest and abdominal CT did not find any evidence of intrahepatic recurrence and extrahepatic metastasis. To find out the reason for AFP increasing, the patient was referred to our center for a whole body PET/CT examination. 18F-FDG PET/CT detected a high metabolic lymph node in the omental position (Figure 2). Due to the maximum standard uptake value (SUVmax), lymph node metastasis was considered. The high metabolic lymph node was excised. Histopathological examination of the resected nodule revealed a metastatic hepatocellular carcinoma. After excision of the tumor, her AFP level decreased to normal. Ten months after resection of the extrahepatic metastasis and 88 mo after partial liver resection, the patient was in good condition with no recurrence at the time when we wrote this paper.
Figure 1 Contrast CT demonstrating a huge lesion at the left lobe of liver (black arrows, portal phase).
Figure 2 Whole body PET showing an isolated highly metabolic focus in the upper abdomen (white arrow) (A), non-enhanced CT (C) detecting a median density lesion in the omenta (white arrow), 18F-FDG PET (B) and fused imaging of PET/CT (D) revealing a highly metabolic lesion at the same position.
DISCUSSION
HCC over 10 cm in diameter is found in a number of patients undergoing hepatic resection. A large HCC has its specific clinicopathological features. Multiple tumor nodules, venous invasion and impaired liver function are factors associated with its recurrence[5]. Hepatic resection of HCC with a diameter ≥ 10 cm at stage II or III is safe and effective for selected patients without liver cirrhosis. The overall incidence of postoperative complications is 39%. The 3-, 5- and 9-year overall survival rates after hepatic resection are 32%, 27%, and 17%, respectively[6]. Appropriate selection of candidates for partial hepatectomy based on the above prognostic factors may play an important role in decreasing the high mortality rate and poor long-term survival of such patients[7].
Approximately 50% of patients with resected HCC may have tumor recurrence. The overall 1-, 3- and 5-year disease-free survival rates are reported to be 43%, 26% and 20%, respectively[1]. Thus, it is of importance to predict its relapse and treat it with other modalities[8]. The role of resection in case of intrahepatic recurrences is widely accepted. If the distribution and localization of extrahepatic metastasis are fully confirmed, these lesions may be resected. In our case, conventional CT did not find any intrahepatic and extrahepatic metastasis. However, the whole body PET/CT detected isolated extrahepatic metastasis which we treated with surgery. 18F-FDG PET/CT is not only a useful tool for preoperative staging, but also a follow-up means better than conventional diagnostic modalities, especially for staging and re-staging after hepatectomy.
In case of an AFP producing HCC, unexplained rise of serum AFP after treatment is an early indicator of tumor recurrence or extrahepatic metastasis. However, the sensitivity of conventional imaging techniques is limited in detecting recurrent diseases in such patients[9]. 18F-FDG PET/CT has proved to be an effective whole-body imaging technique that detects metabolic changes preceding structural findings. It was reported that tumor restaging with PET/CT can detect and localize disease recurrence among patients with no or mild symptoms and an elevated tumor marker level[10]. PET/CT also can provide information about whether the detected disease is resectable. 18F-FDG PET/CT provides fused images that demonstrate the complementary role of functional and anatomic assessments in the diagnosis of cancer recurrence through the precise localization of suspected 18F-FDG uptake foci and their characterization as malignant or benign[11].
TACE is a procedure involving injection of chemotherapeutic agents into the hepatic artery supplying the tumor, followed by embolization with lipiodol or gelfoam pieces. It appears that postoperative adjuvant hepatic arterial chemotherapy is more likely beneficial for preventing recurrence than preoperative TACE. To date, convincing evidence supporting the effectiveness of adjuvant therapy in preventing HCC recurrence is lacking. Validated information in the literature is limited in a paucity of randomized studies. It was reported that meaningful meta-analysis is impossible because of different therapeutic regimens used and the lack of stratification of patients according to the risk of recurrence[12]. Better understanding of biological characteristics of HCC can lead to better outcomes of adjuvant surgical treatment[13]. For example, if patients at a high risk of HCC recurrence could be identified before the resection, they would benefit from additional treatment modalities, such as neoadjuvant therapy, adjuvant therapy and biotherapy. It is not necessary for patients at a low risk of tumor recurrence to receive the above therapies[14]. Molecular imaging in oncology is the noninvasive imaging of the key molecules and molecule-based events characterized by the genotype and phenotype of human cancer. Tumors with increased 18F-FDG uptake are more metabolically active and biologically aggressive. PET/CT with 18F-FDG would play a key role in evaluating recurrence risk of HCC before hepatectomy[15]. Further research is warranted because of the limited number of reports and the absence of randomized trials.
Aggressive management with combined resection of isolated extrahepatic recurrence and re-resection or local therapy for intrahepatic recurrence may offer long-term survival in selected HCC patients. Our case demonstrates that 18F-FDG PET/CT provides the most significant additional information related to the accurate detection of extrahepatic spread of tumors and additional important information in patients with presumed resectable extrahepatic metastases. This test should be used for patients at a high risk of extrahepatic disease and should be evaluated prospectively for all patients under consideration for intrahepatic recurrence and extrahepatic metastasis resection.