Published online Oct 14, 2007. doi: 10.3748/wjg.v13.i38.5154
Revised: June 18, 2007
Accepted: June 26, 2007
Published online: October 14, 2007
We report a cirrhotic patient with duodenal vascular ectasia and spontaneous bleeding. The bleeding was successfully controlled with argon plasma coagulation. Duodenal vascular ectasia may be a cause of upper gastrointestinal bleeding in patients with cirrhosis, and argon plasma coagulation may be effective and safe to achieve hemostasis of this lesion.
- Citation: Lee BJ, Park JJ, Seo YS, Kim JH, Kim A, Yeon JE, Kim JS, Byun KS, Bak YT. Upper gastrointestinal bleeding from duodenal vascular ectasia in a patient with cirrhosis. World J Gastroenterol 2007; 13(38): 5154-5157
- URL: https://www.wjgnet.com/1007-9327/full/v13/i38/5154.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i38.5154
Vascular ectasia of the duodenum is rare[1] and an uncommon source of upper gastroduodenal bleeding. It is associated with chronic illnesses such as aortic valve disease and end-stage renal disease when patients are under long-term hemodialysis[2-4]. Gallagher et al[5] reported a patient with small bowel capillary dilatation and cirrhosis, and suggested that small bowel capillary dilatation appears to be unique in patients with portal hypertension, and may play a role in causing gastrointestinal bleeding. However, to our knowledge, only a few cases of duodenal vascular ectasia have been reported in patients with cirrhosis[5-7]. We report a case of upper gastrointestinal bleeding in a patient with cirrhosis and duodenal vascular ectasia, which was successfully controlled by argon plasma coagulation (APC).
A 62-year-old man was admitted because of melena, dizziness, and anemia with a follow-up history for chronic hepatitis B infection, liver cirrhosis, and hepatocellular carcinoma. About a 2 cm-sized tumor mass was located in subcapsular portion of segment 7. After two sessions of transarterial chemoembolization for the tumor mass, no visible tumor was found. He visited the emergency room two years ago because of hematemesis, and an endoscopic examination revealed esophageal varices with bleeding, which were treated with endoscopic band ligation.
Physical examination revealed blood pressure of 100/80 mmHg, pulse rate of 72 beats per minute, respiratory rate of 14 breaths per minute, and body temperature of 36.8°C. He was alert and oriented to person, place, and time. His sclera was nonicteric and conjunctiva was pale. Chest and heart examinations were normal. Abdominal examination revealed a distended abdomen with prominent shifting dullness. Pitting edema was noted in both lower extremities.
The results of initial laboratory tests were as follows: white blood count (WBC) = 3700/mm3, hemoglobin = 7.3 g/dL, platelets = 34 000/mm3, prothrombin time = 23.8 s, international normalized ratio = 2.05, C-reactive protein = 82.6 mg/dL, total bilirubin= 2.07 mg/dL, direct bilirubin = 0.96 mg/dL, protein = 5.23 g/dL, albumin = 2.83 g/dL, alanine aminotransferase = 67 IU/L, aspartate aminotransferase = 62 IU/L, gamma-glucuronyl transferase = 38 IU/L, alkaline phosphatase = 87 IU/L, glucose = 142 mg/dL, blood urea nitrogen (BUN)/creatine(Cr) = 19.57/0.75 mg/dL, and Na/K/Cl = 120/4.1/87 mEq/mL. Paracentesis revealed clear yellow-colored ascitic fluid, which on analysis showed 0/mm3 WBC, 2000/mm3 red blood cells, 242 mg/dL glucose, and 252 mg/dL protein. The serum α-fetoprotein concentration was 6.2 ng/mL. He was positive for hepatitis B surface antigen and negative for hepatitis B envelope antigen.
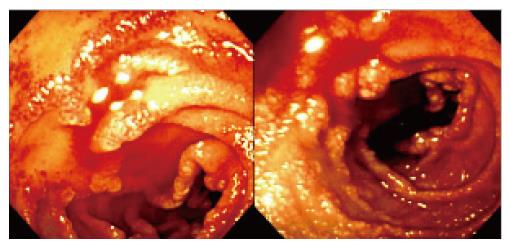
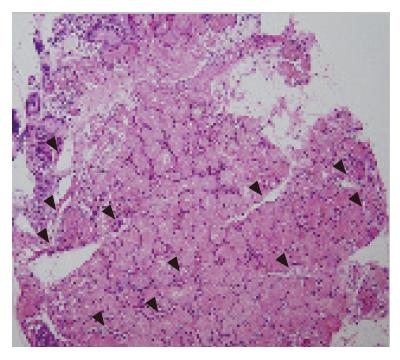
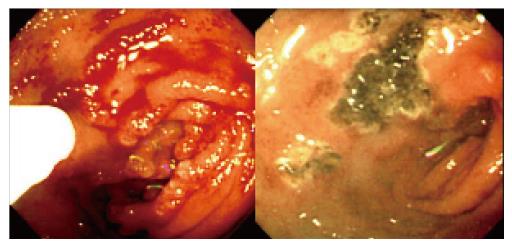
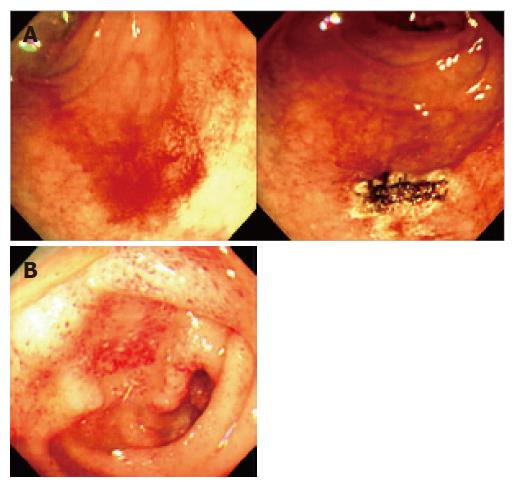
Bleeding from the esophageal varices was suspected and urgent endoscopic examination was performed. However, the urgent endoscopy showed small esophageal varices with no evidence of bleeding, and unexpectedly, vascular ectasia with oozing was found on the duodenal bulb and second portion (Figure 1). Endoscopic biopsy was performed on the vascular ecstatic mucosa and histological examination revealed grossly dilated blood vessels in the Brunner’s glands at the mucosal layer (Figure 2). To achieve hemostasis, APC (Arco-2000, Soring, Germany) was performed (argon gas flow = 1.5 L/min, power = 50 W), which controlled the bleeding without any complications such as bowel perforation (Figure 3). Follow-up endoscopic examination after one week showed minimal blood oozing on the telangiectatic duodenal mucosa, and a second session of APC was performed (Figure 4A). After endoscopic treatment, his hemoglobin concentration did not decrease and his symptoms improved, and the patient was discharged.
Two months after discharge, endoscopic examination revealed a remnant vascular ectatic duodenal mucosa but no spontaneous bleeding (Figure 4B).
Upper gastrointestinal bleeding is one of the most frequent causes of morbidity and mortality during the clinical course of liver cirrhosis[8-11] and has an overall mortality rate of 24% at six weeks and 40% at one year[12]. A recent study showed that gastroesophageal varices (59.1%) comprise the most frequent bleeding lesion in patients with cirrhosis[13]. Others have reported a similar frequency of esophageal varices bleeding, ranging 49%-72%[12,14,15]. Peptic ulcer bleeding is the second most frequent type of bleeding lesion (15.7%)[13].
Upper gastrointestinal vascular ectasia is recognized as an increasingly important source of gastrointestinal bleeding, and can present as that of either overt or of an obscure cause[3,16-19]. Gastric antral vascular ectasia (GAVE) is a distinct vascular abnormality involving mainly the gastric antrum. Endoscopic examination shows linear, friable red streaks radiating from the pylorus. Angiodysplastic lesions are typically discrete, flat, or slightly raised bright-red lesions 2-10 mm in size, often with fern-like margins and a surrounding pale rim[20]. The clinical presentation is either chronic, low-grade bleeding, which often leads to iron-deficiency anemia, or acute bleeding with hematemesis or melena. Patients may have recurrent episodes of bleeding which require multiple transfusions, and become transfusion dependent[20]. A recent study showed that 29% of patients with vascular ectasia also have chronic liver diseases[21].
By definition, GAVE occurs only in the antrum. However, ectopic ectasia has been reported in the cardiac region[22], gastric corpus[23], duodenum[22,24], and possibly in the colon[22]. Astaldi and Strosseli[25] suggested that small bowel biopsies from patients with hepatic cirrhosis might show vascular stasis arising from portal stasis. Bank et al[26] have noted a ‘striking increase in vascularity of the villi’ in a small bowel biopsy of a patient with cirrhosis and esophageal varices. Gallagher et al[5] suggested that capillary dilatation is probably caused by increased pressure in the portal system.
To our knowledge, only a few cases of vascular ectasia of the duodenum have been reported in patients with cirrhosis[5-7]. In one report, histology of the endoscopic duodenal biopsy revealed grossly dilated capillaries in the villi of the duodenum and jejunum, the patient received a portacaval shunt, but died postoperatively[5]. Arendse et al[6] reported a fatal case of vascular ectasia of the duodenum in a patient with cirrhosis, which was revealed by autopsy. Cales et al[7] reported an ectasia in a patient with cirrhosis, which was revealed by autopsy. The patient was treated with endoscopic sclerotherapy and a portosystemic shunt to control the bleeding, although neither was successful. Our study seems to be the first to report successful control of bleeding from vascular ectasia of the duodenum by APC in a patient with cirrhosis.
We attempted to treat bleeding from duodenal vascular ectasia by APC and found a certain improvement on endoscopic examination of the duodenum. However, we did not eradicate the duodenal vascular ectasia. Pavey et al[20] reported that patients with GAVE require more sessions to fully control the bleeding and more transfusion than patients with angiodysplasia. Our patient also seemed to need more sessions of APC to completely eradicate ectasia, although this was not possible because he did not visit our hospital after the last endoscopic examination.
Before the widespread availability of therapeutic endoscopy, vascular ectasia was treated with surgical resection[27,28]. More recently, upper gastrointestinal vascular ectasiae have been treated with various endoscopic techniques including heater probe coagulation[29], bipolar electrocautery[30] and Nd: YAG laser[31-33], and APC[20]. APC is a no-touch electrocoagulation technique in which a high-frequency monopolar alternating current is delivered to the tissue through ionized argon gas[34,35]. The advantages of this method include the technical ease in treating large areas and the ability to achieve superficial coagulation with a controllable depth of injury. The treated areas heal faster and the endpoint of therapy can be reached sooner[34,35]. In our patient, to reduce the risk of bowel perforation, we applied irradiation for 4-6 s with a current of 50 W, and were able to successfully control the bleeding without any serious complications.
In conclusion, duodenal vascular ectasia may be a cause of upper gastrointestinal bleeding in patients with cirrhosis. APC can be used as an effective and safe therapeutic tool to achieve hemostasis of this lesion.
S- Editor Zhu LH L- Editor Wang XL E- Editor Wang HF
| 1. | Tai DI, Chou FF, Lee TY, Lin CC. Vascular ectasia of the duodenum detected by duodenoscopy. Am J Gastroenterol. 1987;82:1071-1073. [PubMed] |
| 2. | Weaver GA, Alpern HD, Davis JS, Ramsey WH, Reichelderfer M. Gastrointestinal angiodysplasia associated with aortic valve disease: part of a spectrum of angiodysplasia of the gut. Gastroenterology. 1979;77:1-11. [PubMed] |
| 3. | Clouse RE, Costigan DJ, Mills BA, Zuckerman GR. Angiodysplasia as a cause of upper gastrointestinal bleeding. Arch Intern Med. 1985;145:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 59] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Cappell MS, Lebwohl O. Cessation of recurrent bleeding from gastrointestinal angiodysplasias after aortic valve replacement. Ann Intern Med. 1986;105:54-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 88] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Gallagher C, Bonar F, Dempsey J, Crowe J. Small bowel capillary dilatation in portal hypertension. Postgrad Med J. 1985;61:541-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Arendse MP, Jaskiewicz K, Funnell I. Massive gastro-intestinal haemorrhage due to vascular ectasia of the duodenum. A case report. S Afr J Surg. 1992;30:111-113. [PubMed] |
| 7. | Calès P, Voigt JJ, Payen JL, Bloom E, Berg P, Vinel JP, Pradère B, Broussy P, Pascal JP. Diffuse vascular ectasia of the antrum, duodenum, and jejunum in a patient with nodular regenerative hyperplasia. Lack of response to portosystemic shunt or gastrectomy. Gut. 1993;34:558-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Franco D, Durandy Y, Deporte A, Bismuth H. Upper gastrointestinal haemorrhage in hepatic cirrhosis: causes and relation to hepatic failure and stress. Lancet. 1977;1:218-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981;80:800-809. [PubMed] |
| 10. | Christensen E, Krintel JJ, Hansen SM, Johansen JK, Juhl E. Prognosis after the first episode of gastrointestinal bleeding or coma in cirrhosis. Survival and prognostic factors. Scand J Gastroenterol. 1989;24:999-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Burroughs AK, Mezzanotte G, Phillips A, McCormick PA, McIntyre N. Cirrhotics with variceal hemorrhage: the importance of the time interval between admission and the start of analysis for survival and rebleeding rates. Hepatology. 1989;9:801-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 107] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | del Olmo JA, Peña A, Serra MA, Wassel AH, Benages A, Rodrigo JM. Predictors of morbidity and mortality after the first episode of upper gastrointestinal bleeding in liver cirrhosis. J Hepatol. 2000;32:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 117] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Lecleire S, Di Fiore F, Merle V, Hervé S, Duhamel C, Rudelli A, Nousbaum JB, Amouretti M, Dupas JL, Gouerou H. Acute upper gastrointestinal bleeding in patients with liver cirrhosis and in noncirrhotic patients: epidemiology and predictive factors of mortality in a prospective multicenter population-based study. J Clin Gastroenterol. 2005;39:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Gatta A, Merkel C, Amodio P, Bellon S, Bellumat A, Bolognesi M, Borsato L, Buttò M, Casson FF, Cavallarin G. Development and validation of a prognostic index predicting death after upper gastrointestinal bleeding in patients with liver cirrhosis: a multicenter study. Am J Gastroenterol. 1994;89:1528-1536. [PubMed] |
| 15. | D'Amico G, De Franchis R. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 592] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 16. | Jensen DM. Current diagnosis and treatment of severe obscure GI hemorrhage. Gastrointest Endosc. 2003;58:256-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Gretz JE, Achem SR. The watermelon stomach: clinical presentation, diagnosis, and treatment. Am J Gastroenterol. 1998;93:890-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Abedi M, Haber GB. Watermelon stomach. Gastroenterologist. 1997;5:179-184. [PubMed] |
| 19. | Jabbari M, Cherry R, Lough JO, Daly DS, Kinnear DG, Goresky CA. Gastric antral vascular ectasia: the watermelon stomach. Gastroenterology. 1984;87:1165-1170. [PubMed] |
| 20. | Pavey DA, Craig PI. Endoscopic therapy for upper-GI vascular ectasias. Gastrointest Endosc. 2004;59:233-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Lonardo A, Greco M, Grisendi A. Bleeding gastrointestinal angiodysplasias: our experience and a review of the literature. Ann Ital Med Int. 2004;19:122-127. [PubMed] |
| 22. | Lux G, Rosch W. Diffuse telangiectasia of the upper GI-tract. Abstract. Endoscopy. 1979;11:281. |
| 23. | Quintero E, Pique JM, Bombi JA, Bordas JM, Sentis J, Elena M, Bosch J, Rodes J. Gastric mucosal vascular ectasias causing bleeding in cirrhosis. A distinct entity associated with hypergastrinemia and low serum levels of pepsinogen I. Gastroenterology. 1987;93:1054-1061. [PubMed] |
| 24. | Wheeler MH, Smith PM, Cotton PB, Evans DM, Lawrie BW. Abnormal blood vessels in the gastric antrum: a cause of upper-gastrointestinal bleeding. Dig Dis Sci. 1979;24:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Astaldi G, Strosselli E. Peroral biopsy of the intestinal mucosa in hepatic cirrhosis. Am J Dig Dis. 1960;5:603-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 65] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Bank S, Marks IN, Moshal MG, TIMME A. Peroral Intestinal Biopsy. Analysis Of Results In 134 Patients. S Afr Med J. 1964;38:451-458. [PubMed] |
| 27. | Moore JD, Thompson NW, Appelman HD, Foley D. Arteriovenous malformations of the gastrointestinal tract. Arch Surg. 1976;111:381-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 187] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 28. | Cavett CM, Selby JH, Hamilton JL, Williamson JW. Arteriovenous malformation in chronic gastrointestinal bleeding. Ann Surg. 1977;185:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 65] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Petrini JL, Johnston JH. Heat probe treatment for antral vascular ectasia. Gastrointest Endosc. 1989;35:324-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Binmoeller KF, Katon RM. Bipolar electrocoagulation for watermelon stomach. Gastrointest Endosc. 1990;36:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Liberski SM, McGarrity TJ, Hartle RJ, Varano V, Reynolds D. The watermelon stomach: long-term outcome in patients treated with Nd: YAG laser therapy. Gastrointest Endosc. 1994;40:584-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Tsai HH, Smith J, Danesh BJ. Successful control of bleeding from gastric antral vascular ectasia (watermelon stomach) by laser photocoagulation. Gut. 1991;32:93-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Gostout CJ, Ahlquist DA, Radford CM, Viggiano TR, Bowyer BA, Balm RK. Endoscopic laser therapy for watermelon stomach. Gastroenterology. 1989;96:1462-1465. [PubMed] |
| 34. | Johanns W, Luis W, Janssen J, Kahl S, Greiner L. Argon plasma coagulation (APC) in gastroenterology: experimental and clinical experiences. Eur J Gastroenterol Hepatol. 1997;9:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Cipolletta L, Bianco MA, Rotondano G, Piscopo R, Prisco A, Garofano ML. Prospective comparison of argon plasma coagulator and heater probe in the endoscopic treatment of major peptic ulcer bleeding. Gastrointest Endosc. 1998;48:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 110] [Article Influence: 4.1] [Reference Citation Analysis (0)] |