Published online Oct 14, 2007. doi: 10.3748/wjg.v13.i38.5090
Revised: May 12, 2007
Accepted: May 26, 2007
Published online: October 14, 2007
AIM: To establish a scoring system for predicting the incidence of postoperative complications and mortality in general surgery based on the physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM), and to evaluate its efficacy.
METHODS: Eighty-four patients with postoperative complications or death and 172 patients without postoperative complications, who underwent surgery in our department during the previous 2 years, were retrospectively analyzed by logistic regression. Fifteen indexes were investigated including age, cardiovascular function, respiratory function, blood test results, endocrine function, central nervous system function, hepatic function, renal function, nutritional status, extent of operative trauma, and course of anesthesia. Modified POSSUM (M-POSSUM) was developed using significant risk factors with its efficacy evaluated.
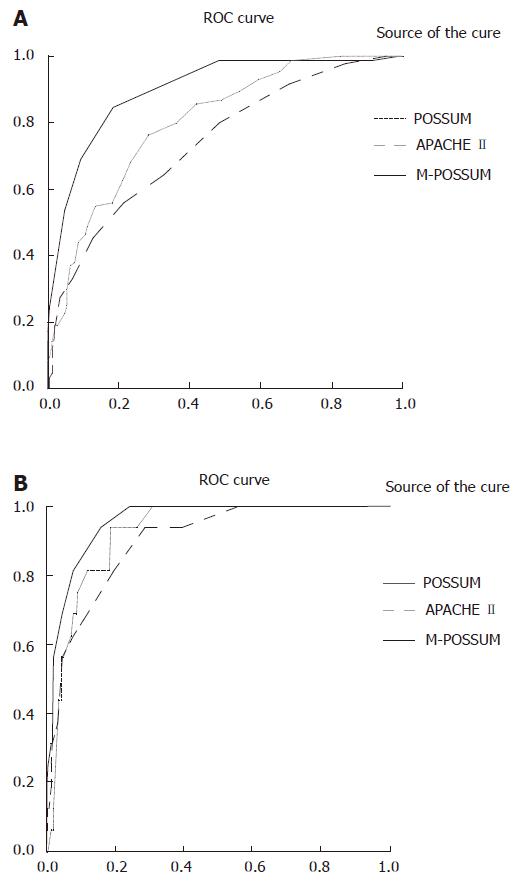
RESULTS: The significant risk factors were found to be age, cardiovascular function, respiratory function, hepatic function, renal function, blood test results, endocrine function, nutritional status, duration of operation, intraoperative blood loss, and course of anesthesia. These factors were all included in the scoring system. There were significant differences in the scores between the patients with and without postoperative complications, between the patients died and survived with complications, and between the patients died and survived without complications. The receiver operating characteristic curves showed that the M-POSSUM could accurately predict postoperative complications and mortality.
CONCLUSION: M-POSSUM correlates well with postoperative complications and mortality, and is more accurate than POSSUM.
- Citation: Ding LA, Sun LQ, Chen SX, Qu LL, Xie DF. Modified physiological and operative score for the enumeration of mortality and morbidity risk assessment model in general surgery. World J Gastroenterol 2007; 13(38): 5090-5095
- URL: https://www.wjgnet.com/1007-9327/full/v13/i38/5090.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i38.5090
With the progress in medical sciences, operative indications for many medical conditions are being expanded, the range of operations is growing, with operative complications increased accordingly. Assessment of the functional condition of organs and systems assists in quantifying the operative risks. Assessment methods allow us to judge the state of an illness and carry out the appropriate preventive treatment immediately, thereby decreasing operative complications and mortality. Numerous scoring systems arecurrently available, including the Glasgow coma scale (GCS), acute physiology, age and cHealth evaluation II (APACHE II)[1], physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM)[2] and others[3-5].
These scoring systems are important tools in deciding the course of treatment. The best known and most widely used scoring systems, APACHE II and POSSUM, have limitations when applied to high-risk general surgical patients. APACHE II is best suited to intensive care patients, but requires 24 h of observation, and weighing tables for individual disease state. POSSUM is limited by its somewhat subjective nature and incomplete evaluation of cardiac signs. We propose the modified POSSUM (M-POSSUM) as a reasonable, practical and objective scoring system that can be used across a broad disease spectrum in general surgery.
The study group included 84 patients with postoperative complications who underwent surgery in our department from May 2002 to May 2004, 16 of them died. The control group included 172 patients without postoperative complications who were randomly selected during the same period of time. General clinical characteristics of the patients including age and gender are illustrated in Table 1. Diagnoses in the malignancy group included colorectal cancer, gastric carcinoma, pancreatic carcinoma, ampullary carcinoma and breast cancer. Diagnoses in the benign group included gastric ulcer, bowel obstruction, cholelithiasis and hyperthyroidism. Concomitant diseases included hypertension, coronary heart disease, pneumopathy, diabetes mellitus, hepatitis and hepatic cirrhosis, cholelithiasis, anemia, cerebrovascular disease and others.
| Clinic data | Postoperativecomplications | Postoperativedeath | Postoperativecomplications |
| No. | 84 | 16 | 172 |
| Age (yr) | 50-79 | 50-79 | 50-79 |
| Average age | 68.67 ± 12.47 | 59.64 ± 13.48 | 69.82 ± 7.98 |
| Gender (Male/Female) | 55/29 | 11/5 | 109/63 |
| Diagnosis, n (%) | |||
| Malignancy | 76 (90.5) | 12 (75.0) | 162 (94.2) |
| Benign | 8 (9.5) | 4 (25.0) | 10 (5.8) |
| Concomitant diseases, n (%) | |||
| Yes | 14 (16.7) | 1 (6.3) | 68 (39.5) |
| No | 70 (83.3) | 15 (93.7) | 104 (60.5) |
The complications and deaths were caused by common illnesses. In this study, we defined complications as outlined in the book “Clinical General Surgery-Diagnostic Analysis and Treatment Gist”. Patients were divided into a group of patients with complications and a group of patients without complications. The group of patients with complications was further divided into a group of patients who survived and a group of patients who died.
We recorded independent variables such as age, sex, function of all organs and systems, results of laboratory tests and special investigations, duration of operation and volume of intraoperative blood loss. The dependent variables were “complications or not” and “death or not” designated as “0” and “1.” We used logistic regression analysis to determine significant risk factors and relative risk (RR).
The indices used were determined by our study results and the prescribed targets and standards of APACHE II and POSSUM. The remaining factors were assigned a point value score (0, 1, 2, 3, or 4). Thus a 15-factor, five-grade scoring system was developed. We compared the difference in M-POSSUM values between various groups, plotted receiver operating characteristic (ROC) curves and calculated the area under the curves to determine the accuracy of M-POSSUM in predicting perioperative and postoperative complication and mortality rates.
All information was stored in a computer database. The general clinical data were analyzed by chi-square test. Risk factors were analyzed by logistic regression analysis. Differences in quantitative data were analyzed by t-test. A ROC curve was used to evaluate the ability of M-POSSUM to predict postoperative complications and mortality. All these analyses were performed using the Statistical Package for Social Sciences (SPSS) version 11.5.
The RR and P were analyzed by logistic regression (Table 2). Eleven significant variables determined were as follows: age, cardiovascular function, respiratory function, blood test results, gastrointestinal function, endocrine function, nutritional status, hepatic function, renal function, type of incision and course of anesthesia.
| Factors | Suffered complications | Died | ||
| RR | P | RR | P | |
| Age (yr) > 60 | 0.681 | 0.356 | 0.211 | 0.008 |
| > 70 | 2.181 | 0.005 | 0.391 | 0.091 |
| > 80 | 1.469 | 0.356 | 0.549 | 0.569 |
| Abnormal circulation system | 2.074 | 0.014 | 1.092 | 0.869 |
| ECG mild change | 0.893 | 0.274 | 0.374 | 0.933 |
| ECG ST-T change | 3.817 | 0.031 | 1.928 | 0.418 |
| Abnormal respiratory system | 3.581 | 0.000 | 1.723 | 0.311 |
| Liver function | 3.438 | 0.000 | 16.007 | 0.000 |
| Blood system | 2.610 | 0.000 | 2.735 | 0.070 |
| Renal function | 4.333 | 0.042 | 15.667 | 0.000 |
| Gastrointestinal diseases | 15.545 | 0.011 | 5.571 | 0.046 |
| Endocrine system | 2.374 | 0.002 | 1.615 | 0.359 |
| Nutrition | 4.938 | 0.000 | 6.000 | 0.003 |
| Central nervous system | 1.492 | 0.506 | 3.286 | 0.148 |
| Operation time > 2 h | 1.097 | 0.096 | 0.028 | 0.112 |
| Operation time > 4 h | 3.541 | 0.013 | 2.549 | 0.093 |
| Operative hemorrhage > 300 mL | 0.783 | 0.306 | 0.481 | 0.216 |
| Operative hemorrhage > 500 mL | 2.347 | 0.007 | 3.392 | 0.027 |
| Palliative excision of malignant tumor | 0.693 | 0.047 | 2.014 | 0.082 |
| Malignant tumor can’t excise | 7.139 | 0.000 | 5.175 | 0.000 |
| BP < 90/60 mmHg during operation | 5.429 | 0.000 | 13.105 | 0.000 |
| Steadyperioperative ECG monitoring | 7.781 | 0.000 | 16.001 | 0.000 |
Using our study results as well as the prescribed targets and standards of APACHE II and POSSUM, we were able to overcome the shortcomings of APACHE II and POSSUM, eliminate some non-significant variables, and determine the indices to be used. The remaining factors were assigned a point value score (0, 1, 2, 3 or 4). Thus, a 15-factor, five-grade scoring system was developed (Table 3).
| Index | 0 | 1 | 2 | 3 | 4 |
| Age (yr) | < 60 | 60-69 | 70-79 | ≥ 80 | |
| Circulatory system | Normal Car Fun, BP, ECG | Car fun grade I, mild HP and abnormal ECG, sinoatrial bradycardia/tachycardia, low valtage of limb lead, BBB | Car fun grade II, Mod. HP, well controlled by med, occasional atrial premature beats | Car fun grade III, myocardial infarct < 3 mon, mod HP by med, ectopic, arythm, ST-T change, artrial fibrillation | Serious car, insuf, AHF, mal HP |
| Respiratory system | Normal | Long history of smoking, CB, asthma, URI, thick pulmonary markings | Mild COPD, mild PF change, mild pneumo | Mod COPD, Mod to serious abnormal PF | Respiratory failure |
| Liver function | Normal | History of hepatitis/cirrhosis of liver, TB < 34.2 μmol/L | TB 34.2-51.3 μmol/L | TB > 51.3 μmol/L | |
| Renal function | Normal | BUN ≤ 10.1 mmol/L, Cr ≤ 170 μmol/L | BUN 10.1-15 mmol/L, Cr 170-300 μmol/L | Renal failure need dialysis | |
| Gastrointestinal tract | Normal | History of chronic gastroenteritis, controlled peptic ulcer | Active gastrointestinal diseases(hemorrhage/ perforation of ulcers, active Crohn’s disease | Percutaneous intestinal fistula | Short bowel syndrome, transplantation of small bowels |
| Blood system | Normal | PLT/WBC decreased mildly, Hb (rectified) > 85 g/L | Hematopathy as stable leukemia, WBC ≥ 14.5 × 109/L | Aplastic anemia, hypersplenism syndrome, leukemia etc. | |
| Endocrine system | Normal | Mild increased BG, UGLu (-), treated hyperthyroidism, hypothyroidism, acromegaly, gout, rheumatoid disease | Mild increased BG, UGLu (+ - + +), and controlled DM, by oral medicine, hormonotherapy, active gout | DM, astable with oral medicine | Diabetic nephropathy |
| Nutritional Status2 | Normal | Slight malnutrition (albumin 30-35 g/L, weight decrease < 2.5 Kg/m) | Moderate malnutrition (albumin < 30 g/L, mass decrease 2.5-5 kg/m); Radiotherapy/chemotherapy | Cachexia | |
| GCS | 15 | 12-14 | 9-11 | ≤ 8 | |
| Operative wound | Mino (OPT < 2 h/ hemorrhage volume < 300 mL) | Mod (OPT 2-4 h/hemorrhage volume 300-500 mL) | Major (OPT > 4 h/hemorrhage volume > 500 mL)/Palliative excision of Mal tumor | M Major++ (excision > 3 organs) /Mal tumor can’t excise | |
| Anesthesia course | Arrhythmia/low BP < 1/2 h | continual low BP/ cardio-pulmonary resuscitation |
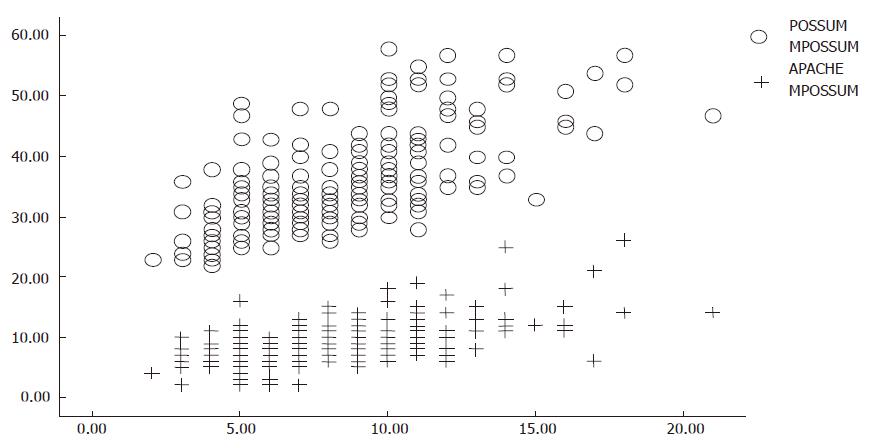
We compared the M-POSSUM scores of the groups (Table 4), which were significantly different in all groups. The frequency distributional graph of M-POSSUM is shown in Figure 1. The ROC curves and areas under them are shown in Figures 2A and 2B, and Table 5. We were able to use them to predict the morbidity and mortality rates in postoperative patients and determine the accuracy of M-POSSUM in predicting morbidity and mortality.
| Group | n | M-POSSUM | t-test | |
| t | P | |||
| No complication | 172 | 6.51 ± 2.22 | -13.723 | 0.000 |
| Complication | 84 | 11.04 ± 2.95 | ||
| Alive | 240 | 7.58 ± 2.83 | -9.096 | 0.000 |
| Dead | 16 | 14.25 ± 3.02 | ||
| Alive with complication | 68 | 10.28 ± 2.38 | -5.693 | 0.000 |
| Variaty | Area | SD | P |
| M-POSSUM (predicting for morbidity) | 0.901 | 0.020 | 0.000 |
| M-POSSUM (predicting for mortality) | 0.955 | 0.016 | 0.000 |
Logistic regression analysis yielded statistically significant equations for both morbidity and mortality. The morbidity equation was lnR/1-R = -7.287 + 0.765M-POSSUM (P = 0.000), and the mortality equation was lnR/1-R = -10.000 + 0.681M-POSSUM (P = 0.000). The predictive accuracy of morbidity equation and mortality equation was 83.6% and 94.1%, respectively.
In general surgery, postoperative morbidity rate ranges 15%-40%. Among patients at the age of 80 years or more undergoing abdominal surgery, the morbidity is higher and the mortality is about 4%[6,7]. While the range and types of operation continue to expand and the treatment guidelines for carcinoma change (progressively emphasizing radical treatment, safety and function), postoperative morbidity and mortality are increasing. Scoring systems are used to objectively assess and quantify the severity of illness, determine prognosis, guide patient monitoring and treatment, and avoid preventable deaths. Ideally, an effective scoring system should also be able to provide useful comparisons between surgeons, surgical units, hospitals and regions.
In general surgery, patients at a higher risk are mostly the elderly, who often suffer from concurrent diseases. Most routine blood biochemistry tests cannot exactly reflect any organ’s physiological status. Tests and special investigations cannot replace detailed case histories and overall somatoscopy. Baseline health status, previous complications and concurrent diseases can all be found in case history. The frequently used scoring systems, APACHE II and POSSUM, have some limitations[8-13]. They lay stress on physiological criteria, but not on hepatic function, blood glucose level and nutritional status, all of which were found to be independent factors affecting morbidity and mortality in our study. The POSSUM has been modified to form P-POSSUM, which is considered more accurate in predicting clinical results[5,14]. However, no other reports support it[15,16].
It has been accepted that age and morbidity is correlated with mortality. Elderly patients with concurrent diseases are more likely to develop perioperative and postoperative complications. In our study, a significant difference was found in the number of concurrent diseases between the groups of patients with and without complications. The concurrent diseases associated with a higher morbidity included high blood pressure, coronary disease, chronic lung disease, diabetes and hepatic cirrhosis. This is identical with the results in previous reports. Baue[17] reported that the main causes of death after major operations are acute respiratory distress syndrome (ARDS), stress ulcer, renal failure, intra-abdominal abscess, multiple organ dysfunction syndrome (MODS) and systemic inflammatory response syndrome (SIRS). In our study, the complications in 16 patients who died were infection, fistula, and hemorrhage, leading to MODS and shock. We found that the factors with the highest correlation with death were blood pressure, electrocardiographic activity during anesthesia, hepatic function, renal function, nutritional status, gastrointestinal function and volume of intraoperative blood loss. Surgeons should therefore improve or correct such abnormalities before operation, to prevent complications, and should promptly identify and manage perioperative and postoperative complications.
A metabolically active organism is in a state of constant dynamic balance, and a static physiological index cannot reflect the dynamic changes. In our study, the significant independent factors were determined by linear multivariate discriminant analysis.
In the present study, the main factors influencing morbidity were gastrointestinal function, course of anesthesia, nutritional status, renal function, respiratory function, hepatic function, cardiovascular function and a non-excisable malignant tumor. The main factors influencing mortality were hepatic function, renal function, nutritional status, digestive tract function and a non-excisable malignant tumor. These results can guide surgeons to maintain stable blood pressure and monitor electrocardiographic activity perioperatively, and to be cautious about operating on late-stage malignant tumors, in order to decrease morbidity and mortality.
In contrast to APACHE II and POSSUM, the present scoring system is based on GCS, APACHE II and POSSUM, supplemented with the following indices: hepatic function (bilirubin), blood glucose level, gastrointestinal function and nutritional status (albumin). However, body temperature, heart rate, sodium and potassium, which are always normal preoperatively in general surgery, are not considered. To avoid repetition, duration of operation, volume of intraoperative blood loss and surgery are considered an operative wound index for a malignant tumor. M-POSSUM also takes blood pressure and electrocardiographic activity into consideration during anesthesia.
The area under the ROC curve reflects the accuracy of prediction. In general, the accuracy is low when the area is in the range of 0.5-0.7, intermediate when the area is between 0.7 and 0.9, and high when the area is greater than 0.9. The ROC curves for morbidity and mortality demonstrate that M-POSSUM is a more accurate predictor than POSSUM. The predictive accuracy for morbidity and mortality is 83.6% and 94.1%, respectively.
Using M-POSSUM, we can obtain a numerical estimate of the health status of an individual patient prior to operation, enabling us to adjust the type and duration of operation and determine reasonably individualized postoperative monitoring and treatment so as to decrease morbidity and mortality in general surgery, especially in aged patients.
In conclusion, M-POSSUM is more accurate than POSSUM and APACHE II in predicting postoperative morbidity and mortality, and therefore seems to be a better model for risk assessment.
The authors thank Professor Zhi-Xu Wang, Medical Nutrition Institute of Qingdao University, for assistance with statistical calculation, and Director Xiu-Lin He, Nutrition Center of the Affiliated Hospital of Medical College, Qingdao University and staff of the Department of General Surgery for their help and assistance.
With the development in surgical techniques, the surgical domain is enlarging and more diseases are managed with surgery. The incidence of post-operation complications and mortality is increasing because of the increasing number of elderly and tumor patients. Surgeons should be able to evaluate patients effectively preoperatively, by quantitating the operative risk, in order to decrease the incidence of postoperative complications and mortality. An attempt was made to achieve this in the present study.
Modern surgeons are faced with many problems, such as an aging population and complicated critical trauma. There is a significant increase in the number of patients suffering from advanced tumors and critical organ disease or dysfunction. Therefore, it is important to increase curative effects and decrease failure rates of therapy. These issues can be solved with the development of scoring systems such as APACHEI, II, III and POSSUM.
Three indices of POSSUM which are poorly correlated with postoperative outcome (body temperature, serum electrolytes and type of surgery) were excluded from M-POSSUM. Six indices which are better correlated with past history, course of anesthesia, hepatic function, gastrointestinal function, endocrine function and nutritional status were included. M-POSSUM correlates well with APACHE II and POSSUM, and is superior to both of them.
M-POSSUM can decrease postoperative complications after targeted preoperative therapeutic measures in intermediate and high risk patients.
Scoring systems such as those defined by APACHE I, II, III and POSSUM, or the American Society of Anesthesiologists (ASA) are used to quantify the severity of an illness before treatment or surgery.
This study is interesting and scientific and readable.
S- Editor Ma N L- Editor Wang XL E- Editor Li JL
| 1. | Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10902] [Cited by in RCA: 11113] [Article Influence: 277.8] [Reference Citation Analysis (0)] |
| 2. | Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1126] [Cited by in RCA: 1134] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 3. | Brooks MJ, Sutton R, Sarin S. Comparison of Surgical Risk Score, POSSUM and p-POSSUM in higher-risk surgical patients. Br J Surg. 2005;92:1288-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 96] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Ramkumar T, Ng V, Fowler L, Farouk R. A comparison of POSSUM, P-POSSUM and colorectal POSSUM for the prediction of postoperative mortality in patients undergoing colorectal resection. Dis Colon Rectum. 2006;49:330-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Slim K, Panis Y, Alves A, Kwiatkowski F, Mathieu P, Mantion G. Predicting postoperative mortality in patients undergoing colorectal surgery. World J Surg. 2006;30:100-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Unalp HR, Kamer E, Kar H, Bal A, Peskersoy M, Ali Onal M. Urgent abdominal re-explorations. World J Emerg Surg. 2006;1:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Martin RC, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 530] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 8. | Nyström PO, Bax R, Dellinger EP, Dominioni L, Knaus WA, Meakins JL, Ohmann C, Solomkin JS, Wacha H, Wittmann DH. Proposed definitions for diagnosis, severity scoring, stratification, and outcome for trials on intraabdominal infection. Joint Working Party of SIS North America and Europe. World J Surg. 1990;14:148-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 73] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Van Le L, Fakhry S, Walton LA, Moore DH, Fowler WC, Rutledge R. Use of the APACHE II scoring system to determine mortality of gynecologic oncology patients in the intensive care unit. Obstet Gynecol. 1995;85:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Daffurn K, Kerridge R, Hillman KM. Active management of the dying patient. Med J Aust. 1992;157:701-704. [PubMed] |
| 11. | Higgins TL, McGee WT, Steingrub JS, Rapoport J, Lemeshow S, Teres D. Early indicators of prolonged intensive care unit stay: impact of illness severity, physician staffing, and pre-intensive care unit length of stay. Crit Care Med. 2003;31:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 147] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Tekkis PP, Bentley AJ, Kocher HM, South LM, Trotter GA. Risk scoring in surgical patients. Br J Surg. 1999;86:1225. [PubMed] |
| 13. | Neary WD, Heather BP, Earnshaw JJ. The Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (POSSUM). Br J Surg. 2003;90:157-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 98] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ. POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg. 1998;85:1217-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 506] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 15. | Organ N, Morgan T, Venkatesh B, Purdie D. Evaluation of the P-POSSUM mortality prediction algorithm in Australian surgical intensive care unit patients. ANZ J Surg. 2002;72:735-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Markus PM, Martell J, Leister I, Horstmann O, Brinker J, Becker H. Predicting postoperative morbidity by clinical assessment. Br J Surg. 2005;92:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Baue AE, Durham R, Faist E. Systemic inflammatory response syndrome (SIRS), multiple organ dysfunction syndrome (MODS), multiple organ failure (MOF): are we winning the battle? Shock. 1998;10:79-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 327] [Article Influence: 12.1] [Reference Citation Analysis (0)] |