Published online Oct 7, 2007. doi: 10.3748/wjg.v13.i37.5035
Revised: August 4, 2007
Accepted: August 10, 2007
Published online: October 7, 2007
As among persons with normal anatomy, occasional patients with situs inversus develop malignant tumors. Recently, several laparoscopic operations have been reported in patients with situs inversus. We describe laparoscopic hemicolectomy with radical lymphadenectomy in such a patient. Careful consideration of the mirror-image anatomy permitted safe operation using techniques not otherwise differing from those in ordinary cases. Thus, curative laparoscopic surgery for colon cancer in the presence of situs inversus is feasible and safe.
- Citation: Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, Osugi H. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol 2007; 13(37): 5035-5037
- URL: https://www.wjgnet.com/1007-9327/full/v13/i37/5035.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i37.5035
Situs inversus (SI) is an uncommon anatomic anomaly. Situs inversus totalis denotes complete right-left inversion of thoracic and abdominal viscera[1-7]. Accordingly, surgical procedures are considered more difficult in patients with SI in other patients because of different anatomic positions of organs, especially in laparoscopic surgery. While laparoscopic colorectal surgery recently has become a standard procedure, only two previous reports of laparoscopic surgery for colonic disease in patients with SI are available[3,8]. Here, we display some figures of laparoscopic hemicolectomy with radical lymphadenectomy in a patient with SI, highlighting differences from the ordinary situation.
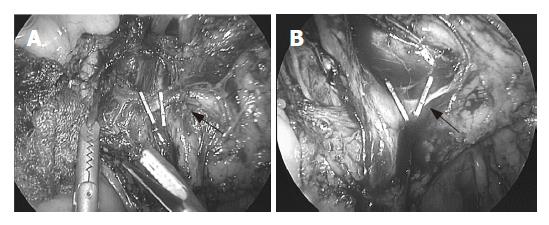
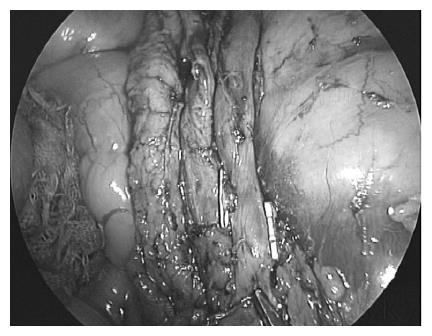
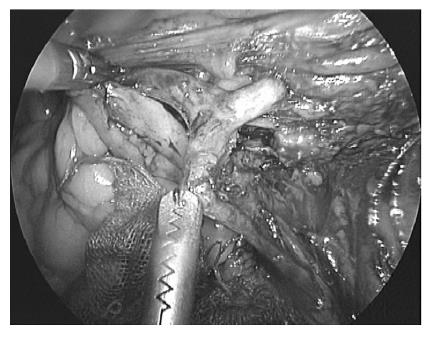
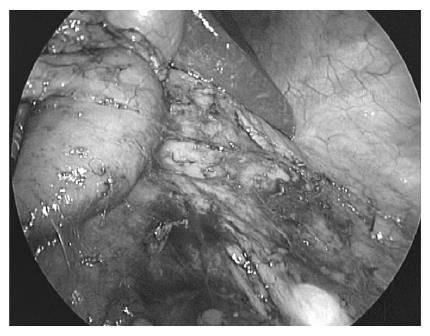
A 53-year-old woman known since early childhood to have situs inversus totalis was referred to her personal physician upon detection of anemia. She underwent ovariectomy for ovarian cancer at the age of 48 years. With a diagnosis of ascending colon cancer according to barium enema radiograph and colonoscopy, the patient was admitted to our hospital for further evaluation and surgical treatment. Laboratory examination confirmed anemia (red blood cell count, 377 × 104/mm3; hemoglobin, 9.3 g/dL; hematocrit, 29.9%). The serum concentration of carcinoembryonic antigen was elevated (89.8 ng/mL; reference range, 0 to 4.9 ng/mL). A chest radiograph showed dextrocardia and a right subphrenic gastric bubble (Figure 1). Abdominal ultrasonography and computed tomography (Figure 2) showed complete transposition of abdominal viscera, confirming situs inversus totalis. Furthermore, the superior mesenteric vein was located to the left of the superior mesenteric artery. Barium enema and colonoscopy showed an ulcerated lesion in the ascending colon. Histologic examination of a specimen from colonscopic biopsy indicated adenocarcinoma. According to the findings above, laparoscopic hemicolectomy with radical lymphadenectomy was performed. With the patient in a lithotomy position, the operator was situated between the legs, the first assistant on the left, and the endoscopist on the right with a reversal of assistants’ location for orthotopic patients. Trocars also were placed in a mirror-image manner, including a 12-mm umbilical trocar for the camera, a 12-mm trocar in the right iliac fossa and a 5-mm trocar in the left iliac fossa as working ports for the operator, and a 5-mm trocar in the left flank and a 12-mm trocar in the epigastrium for traction. The liver was located on the left and the spleen on the right. The mesentery was incised just caudal to the ileocolic vessels, and the fusion fascia was mobilized searching the anterior surface of the transverse portion of the duodenum. The ileocolic vessels were identified and divided after the superior mesenteric vein was exposed (Figure 3). Radical lymphadenectomy was continued up to the root of the middle colic artery (Figure 4), the left branch of the artery was divided (Figure 5). Mobilization of the ascending colon including the tumor (Figure 6) was followed by reconstruction using an end-to-end triangulating stapling method[9] carried out extracorporeally through a 5-cm skin incision continued to the umbilical port. No additional ports were needed. Operation time was 191 min and blood loss was 60 mL, similar to typical findings in orthotopic patients. The procedure was not complicated apart from a need to appreciate mirror-image aspects of anatomy and surgery, including some awkwardness in handling surgical or endoscopic instruments in the presence of right-left inversion. Macroscopically, the tumor was a 45 mm × 25 mm ulcerated lesion in the ascending colon. Histologic examination of the resected specimen disclosed a well-differentiated adenocarcinoma with serosal, lymphatic, and venous invasion, as well as lymph node metastasis.After an uneventful postoperative course, the patient was discharged on the 10th postoperative day.
Predisposition to situs inversus (SI), a rare congenital condition present in 1 of 5000 to 10 000 live births, is inherited in a simple autosomal recessive manner. SI may involve transposition of thoracic or abdominal organs, or both. Situs inversus totalis denotes complete inversion of thoracic and abdominal viscera[1-7]. Apart from genetic predisposition, no etiologies have been established, and SI itself has no pathophysiologic significance[1,5]. However, surgical techniques need to allow for spatial implications of this condition. Cardiac and intestinal malformations as well as other visceral and vascular anomalies that can be associated with SI follow variable patterns[1]. Careful preoperative anatomic assessment is vitally important in the presence of SI[1,5]. Careful preoperative planning of laparoscopic procedures (positions of operator, assistants, and trocar sites as well as instrumentation) is needed, as mentioned in several previous reports of laparoscopic surgery in patients with SI[2-4,6-8]. No specific intraoperative complications have been described in the reports above. Likewise, no unanticipated problems were encountered in our case. Patients with SI who develop malignant tumors in lung, liver, stomach, or colon have been encountered[1,5]. In the present case, the patient was operated on by a surgeon with experience in over 400 laparoscopic colorectal operations. The position of the operator did not differ from that in orthotopic patients, but positions of assistants and trocars were reversed from the usual locations. Endoscopic instruments were used as they were ordinarily used, although mechanical awkwardness was noted in handling surgical or endoscopic instruments in the presence of reversed spatial relationship. Careful recognition of the mirror-image anatomy permitted safe radical lymphadenectomy and mobilization of the colon, while the surgical technique itself did not differ from the usual situation. Operative time and blood loss were comparable to those in orthotopic patients. Laparoscopic surgery for colon cancer in SI thus should be considered a feasible, safe and curative procedure that surgeons should not hesitate to perform.
S- Editor Zhu LH L- Editor Wang XL E- Editor Wang HF
| 1. | Iwamura T, Shibata N, Haraguchi Y, Hisashi Y, Nishikawa T, Yamada H, Hayashi T, Toyoda K. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J Clin Gastroenterol. 2001;33:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Song JY, Rana N, Rotman CA. Laparoscopic appendectomy in a female patient with situs inversus: case report and literature review. JSLS. 2004;8:175-177. [PubMed] |
| 3. | Kobus C, Targarona EM, Bendahan GE, Alonso V, Balagué C, Vela S, Garriga J, Trias M. Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbecks Arch Surg. 2004;389:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Docimo G, Manzi F, Maione L, Canero A, Veneto F, Lo Schiavo F, Sparavigna L, Amoroso V, De Rosa M, Docimo L. Case report: laparoscopic cholecystectomy in situs viscerum inversus. Hepatogastroenterology. 2004;51:958-960. [PubMed] |
| 5. | Goi T, Kawasaki M, Yamazaki T, Koneri K, Katayama K, Hirose K, Yamaguchi A. Ascending colon cancer with hepatic metastasis and cholecystolithiasis in a patient with situs inversus totalis without any expression of UVRAG mRNA: report of a case. Surg Today. 2003;33:702-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Kamitani S, Tsutamoto Y, Hanasawa K, Tani T. Laparoscopic cholecystectomy in situs inversus totalis with "inferior" cystic artery: a case report. World J Gastroenterol. 2005;11:5232-5234. [PubMed] |
| 7. | Oms LM, Badia JM. Laparoscopic cholecystectomy in situs inversus totalis: The importance of being left-handed. Surg Endosc. 2003;17:1859-1861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Davies H, Slater GH, Bailey M. Laparascopic sigmoid colectomy for diverticular disease in a patient with situs inversus. Surg Endosc. 2003;17:160-161. [PubMed] |
| 9. | Fukunaga Y, Higashino M, Tanimura S, Nishiguchi Y, Kishida S, Nishikawa M, Ogata A, Osugi H. A novel laparoscopic technique for stapled colon and rectal anastomosis. Tech Coloproctol. 2003;7:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |