Published online Sep 21, 2007. doi: 10.3748/wjg.v13.i35.4716
Revised: April 23, 2007
Accepted: April 29, 2007
Published online: September 21, 2007
Iron is an essential trace metal in the human diet due to its obligate role in a number of metabolic processes. In the diet, iron is present in a number of different forms, generally described as haem (from haemoglobin and myoglobin in animal tissue) and non-haem iron (including ferric oxides and salts, ferritin and lactoferrin). This review describes the molecular mechanisms that co-ordinate the absorption of iron from the diet and its release into the circulation. While many components of the iron transport pathway have been elucidated, a number of key issues still remain to be resolved. Future work in this area will provide a clearer picture regarding the transcellular flux of iron and its regulation by dietary and humoral factors.
- Citation: Sharp P, Srai SK. Molecular mechanisms involved in intestinal iron absorption. World J Gastroenterol 2007; 13(35): 4716-4724
- URL: https://www.wjgnet.com/1007-9327/full/v13/i35/4716.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i35.4716
Iron is an essential trace metal for all organisms. In humans it plays numerous biochemical roles, including oxygen binding in haemoglobin and as an important catalytic centre in many enzymes, for example the cytochromes. In normal healthy adults, some 0.5-2 mg of iron is lost each day due to blood loss and the constant exfoliation of iron-containing epithelial cells that line the gastrointestinal and urinary tracts, skin and hair. Therefore, the same amount of iron from dietary sources is required each day to replace the lost iron and maintain body iron homeostasis. Even though iron is an essential metal in human metabolism, it is highly toxic to cells and tissues if present in elevated levels. Perversely, humans do not possess the necessary machinery to rid the body of excess iron and, therefore, the absorptive process must be tightly regulated within defined physiological limits to avoid pathologies associated with both iron deficiency and overload.
Dietary iron is found in two basic forms, either as haem-found in meat and meat products-or non-haem iron-present in cereals, vegetables, pulses, beans, fruits etc in a number of forms ranging from simple iron oxides and salts to more complex organic chelates. Non-haem iron predominates in all diets comprising some 90%-95% of total daily iron intake. The absorption of both haem and non-haem iron takes place almost exclusively in the duodenum and the bioavailability of iron from these sources is influenced by a number of variables, e.g. the iron content of foods, the type of iron present, i.e. haem or non-haem, and other dietary constituents. Importantly, absorption is also regulated in line with metabolic demands that reflect the amount of iron stored in the body, and the requirements for red blood cell production. These humoral mechanisms are further reviewed in this volume[1].
Despite accounting for only 5%-10% of dietary iron in western countries, haem is the most bioavailable source of iron amounting to is some 20%-30%[2]. In contrast, the bioavailability of non-haem iron is low-only 1%-10% of the dietary load is absorbed-and is profoundly influenced by other dietary components that can enhance or inhibit non-haem iron bioavailability. The most potent enhancer is ascorbic acid (vitamin C), which acts by reducing ferric iron to the more soluble and absorbable ferrous form. Phytates found in cereal products and polyphenolic compounds found in all plant products are the most potent dietary inhibitors of non-haem iron absorption. However, it is important to note that on an equimolar basis the pro-absorptive action of dietary ascorbic acid can counteract the inhibitory effect of phytates and polyphenols[3].
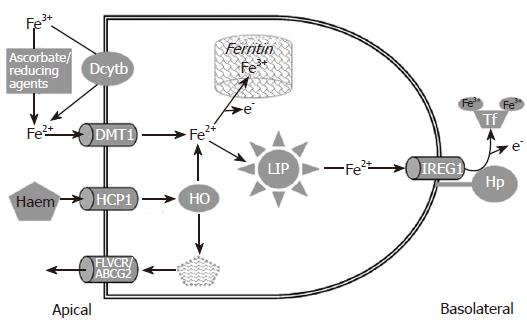
In recent years our understanding of the mechanisms involved in dietary iron absorption by duodenal enterocytes has increased dramatically. Both haem and non-haem iron are taken up in this proximal region of the small intestine, though their transport across the apical membrane of the enterocytes occurs through totally independent pathways (Figure 1).
The majority of dietary non-haem iron enters the gastrointestinal tract in the ferric form. However, Fe3+ is thought to be essentially non-bioavailable (see below) and, therefore, it must first be converted to ferrous iron prior to absorption. There are numerous dietary components capable of reducing Fe3+ to Fe2+, including ascorbic acid[4], and amino acids such as cysteine[5] and histidine[6]. It is believed that the action of these dietary reducing agents takes place in the acidic environment of the gastric lumen. Indeed the essential requirement for an acid environment in iron absorption is exemplified by the fact that achlorhydria is commonly associated with iron deficiency anaemia[7,8]. However, ferric iron reaching the duodenal enterocytes may still be reduced by the cells endogenous reducing activity. A number of studies have demonstrated that the brush-border surface of duodenal enterocytes and cultured intestinal cells possess ferric reductase enzymic activity[9-11]. Using a subtractive cloning strategy designed to identify intestinal genes involved in iron absorption, Dcytb (for duodenal cytochrome b), a homologue of cytochrome b561, was identified as the enzyme responsible for this process[12]. Like cytochrome b561, Dcytb is a haem-containing protein with putative binding sites for ascorbate and semi-dehydroascorbate. The protein is expressed on the brush border membrane of duodenal enterocytes, the major site for the absorption of dietary iron. Moreover, antibodies raised against Dcytb block the endogenous ferric reductase activity of the duodenal brush border membrane, providing further evidence for a functional role in dietary iron processing[12].
Intriguingly, a recent study has reported that the targeted disruption of the Cybrd1 gene in mice (which encodes Dcytb) does not lead to an iron deficient phenotype[13], implying that Dcytb is not necessary for intestinal iron absorption in mice. However, an important caveat to this study is the fact that mice are able to synthesize significant quantities of ascorbic acid-unlike humans who are reliant on dietary vitamin C to satisfy their requirements-and may, therefore, have less need for a duodenal surface ferric reductase.
Following reduction either by Dcytb or dietary reducing agents, the resulting Fe2+ becomes a substrate for the divalent metal transporter, DMT1-also known as the divalent cation transporter, DCT1[14], and natural resistance associated macrophage protein, Nramp2[15]. The relatively low pH of the proximal duodenum together with the acid microclimate present at the brush border membrane[16,17] stabilises iron in the ferrous form and provides a rich source of protons that are essential for driving iron uptake across the apical membrane of the intestinal epithelium[14,18].
The role of this transporter in intestinal iron homeostasis has been highlighted by a number of studies. Our work[18] and that of others[19] have shown that antibodies to DMT1 can significantly inhibit iron absorption. Furthermore, targeted disruption of DMT1 in mice has revealed the essential role of this transporter in both intestinal iron absorption and in erythroid precursor development[20]. In addition to these biochemical and molecular manipulations, two rodent models, the mk/mk mouse[15] and the Belgrade (b) rat[21], which posses a spontaneous mutation (G185R) in the DMT1 gene, exhibit defective intestinal iron uptake and microcytic anaemia. More recently a number of mutations in human DMT1 have also been identified[22-25] which in turn lead to the development of microcytic anaemia.
The molecular identity of the functional DMT1 isoform in intestinal epithelial cells has been the subject of recent debate. At least four isoforms exist through alternate splicing in exon 16[26] and the presence of two transcription start sites-named exon 1A and 1B[27]. Exon 16 splicing gives rise to two variants which differ in their terminal 19-25 amino acids and their 3′ untranslated sequence (UTR). Interestingly one of these variants contains an iron responsive element in its 3′ UTR[26]. The significance of this is discussed later in this review. All four isoforms can be detected at varying levels in intestinal epithelial cells[27], but the exon 1A/IRE-containing variant has been suggested to be the major functional isoform in absorptive enterocytes.
We stated earlier that Fe3+ is thought to be non-bioavailable. However, some workers have proposed that Fe3+ might be absorbed by intestinal enterocytes via a mechanism that is distinct from DMT1 (reviewed in[28]). In this model, ferric iron, which is insoluble at physiological pH, is released from the food matrix in the acidic environment of the stomach, and is chelated by mucins on the duodenal brush border surface, which maintain the iron in the ferric state. Fe3+ enters the enterocyte across the apical membrane via interaction with β3-integrin and mobilferrin (a calreticulin homologue). In the cytosol, this complex combines with flavin monooxygenase and β2-microglobulin to form a larger conglomerate (approximately 520 kDa) known as paraferritin, which has ferric reductase activity resulting in the conversion of the absorbed Fe3+ to Fe2+. Recent evidence suggests that the paraferritin complex may also contain DMT1[29], which may permit the delivery of ferrous iron to intracellular organelles.
In animal and plant tissues, the major iron storage protein is ferritin. Most nutrition texts focus only on haem and non-haem iron, and generally ignore the possibility that ferritin may be an important nutritional source of iron. While the issue of ferritin bioavailability is still controversial, a number of studies have shown that both plant and animal ferritin sources are absorbed in humans[30-32] with a bioavailability equivalent to that of ferrous sulphate. The ferritin iron uptake mechanism is yet to be determined. One possibility is that ferritin is broken down by protease activity in the upper gastrointestinal tract and the released iron is absorbed via the Dcytb/DMT1 route. However, studies have shown that ferritin is largely resistant to high temperature, low pH and protein denaturing agents[33,34]. Therefore, it is possible that ferritin may be absorbed intact and broken down intracellularly (in the lysosomes) to liberate its iron load. In support of this latter possibility, one study has reported that iron and ferritin protein are both taken up by the intestinal Caco-2 cell line[35]. Such a mechanism would require the presence of a ferritin receptor on the apical membrane of intestinal enterocytes. While the presence of ferritin receptors has been postulated on liver[36] and placental[37] plasma membranes, none has yet been identified in intestinal tissue. Taken together this evidence suggests that the molecular identity of at least one important intestinal iron transport gene may remain to be discovered.
In breast-fed infants, a major proportion of iron is bound to the human milk protein lactoferrin, an iron-binding protein capable of binding two ferric ions[38]. Specific receptors for lactoferrin have been identified on the brush border surface of foetal enterocytes[39] and subsequent studies have shown that these receptors mediate the uptake of lactoferrin-bound iron in intestinal epithelial cell cultures[40]. Interestingly, a recent study looking at ontogenic changes in the expression of iron transport proteins in mouse small intestine, has suggested that the lactoferrin receptor may be the principal iron transport pathway in early life[41]. Intriguingly, a recent human volunteer study has indicated that the nutritional importance of lactoferrin may not be limited to infants since it is also a bioavailable source of iron (with equivalent bioavailability to ferrous sulphate) in young adult females[42].
Non-vegetarian diets provide an additional and important source of iron in the form of haem (largely from haemoglobin and myoglobin). While haem comprises only approximately 10% of dietary iron intake, because it is more bioavailable than non-haem iron, it may contribute as much as half of the total iron absorbed from western meat-rich diets[43]. Despite the wealth of information available on the uptake of non-haem iron, the mechanisms involved in haem iron absorption are only just beginning to emerge. Early work on intestinal absorption suggested that haem binds to the duodenal brush border membrane and is absorbed as an intact molecule[43,44]. In support of this proposed mechanism, workers have reported the existence of haem binding proteins on pig enterocytes[45,46] and intestinal Caco-2 cells[47]. More recently, a number of candidate haem binding proteins have been identified in the intestinal epithelial cells including the ATP-binding cassette protein, ABCG2[48], the feline leukaemia virus C receptor protein, FLVCR[49] and the haem carrier protein, HCP1[50]. Of these candidate haem transporters, ABCG2 and FLVCR mediate haem efflux and only HCP1 acts as a haem import protein. The high duodenal expression of HCP1 suggests that it may be the protein involved in haem uptake from the diet. However, the precise role of HCP1 in iron metabolism remains to be fully elucidated. This issue has been complicated by recent data indicating that HCP1 may also function as a proton-coupled folate transporter, independent from its haem transporting properties[51].
Following absorption, haem is detectable in membrane-bound vesicles within the cytoplasm[52,53]. Within these vesicles, it is thought that the iron contained with the protoporphyrin ring is excised by the action of haem oxygenase 1[54] yielding ferrous iron which enters a common intracellular pool along with the iron absorbed via the non-haem transport pathways. Digestion appears to be complete within the enterocytes since a number of studies have failed to detect intact haem efflux across the basolateral membrane[44,47]. One intriguing possibility is that the efflux proteins ABCG2 and FLVCR, also expressed in the duodenum, may act to remove bilirubin formed as a by-product of haem degradation from the enterocytes.
At this stage, the absorbed iron has two fates depending on the body’s requirements. If the body stores are replete, and there is no increased erythropoietic drive, a significant amount of newly absorbed iron will be stored in the enterocytes as ferritin. Because duodenal enterocytes turnover very rapidly (their lifespan is approximately 3-4 d) and the majority of enterocytes contributing to absorption lie in the mid/upper villus region, this intracellular ferritin iron is quickly lost into the intestinal lumen as the ageing cells are sloughed off at the villus tip. Interestingly, in human subjects there is a positive correlation between dietary iron bioavailability and faecal ferritin content which supports the above mechanism[55,56]. Indeed it is likely that this is a very important mechanism for controlling the release of iron into the circulation.
The mechanism by which iron is translocated from the apical pole of the enterocytes so that it becomes available for export across the basolateral membrane is poorly understood. A body of evidence has emerged from studies in Caco-2 cells for a vesicular transport pathway that co-ordinates the transcellular movement of iron. Central to this mechanism is apo-transferrin (apo-Tf) which when added at the basolateral surface of the Caco-2 cell monolayer stimulates transepithelial iron flux in a dose-dependent manner[57-59]. Interestingly, in Caco-2 cells apo-Tf and Fe-Tf, once taken up from the basolateral medium, appear to be directed into distinct endosomal vesicular fractions[59,60]. The apo-Tf containing endosomes are routed towards the apical pole of the cell where they co-localise with vesicles containing DMT1[61]. It is proposed that the iron entering the cell along with DMT1 is transferred to apo-Tf within these endocytic vesicles, and is subsequently exocytosed into the basolateral medium as Fe-Tf. Using a combination of biochemical inhibitors to disrupt this vesicular network, it is estimated that this pathway may count for as much as 50% of the transepithelial iron flux in Caco-2 cells[62,63].
While on the face of it, the above studies provide compelling evidence for a co-ordinated mechanism for the transcellular routing of iron, a number of caveats must be taken into consideration. (1) This model requires the expression of both DMT1 on the apical surface and transferrin receptors (TfR) on the basolateral membrane of the same enterocytes. While this requirement holds for Caco-2 cells[64], the evidence from rat and mouse intestine suggests that TfR are predominantly expressed in the proliferating crypt and lower villus enterocytes[65-69] while dietary iron uptake through apical membrane DMT1 occurs in the upper villus enterocytes[70-73]. (2) Recent studies have shown that intestinal-specific inactivation of IREG1 (the basolateral iron transporter) results in anaemia confirming the essential role of this pathway in iron homeostasis[74]. (3) Caco-2 cells, while an excellent model of the intestinal epithelium, exhibit some non-enterocyte properties including the ability to synthesize and secrete transferrin[75-76]. Taken together, all of these studies highlight the need for further investigation into the transcellular iron transport mechanisms and their role in maintaining body iron homeostasis.
Efflux of iron across the basolateral surface of enterocytes is achieved through the co-ordinated action of a transport protein IREG1[77]-also known as ferroportin[78] and MTP1[79]-and a ferrioxidase, hephaestin[80]. Studies in which IREG1 was expressed in Xenopus laevis oocytes indicate that this is a unidirectional efflux transporter of ferrous iron[77,78]. Interestingly, this efflux function is up-regulated in the presence of ceruloplasmin, a copper binding ferrioxidase, plus transferrin to bind the newly liberated iron[77]. This suggests that while ferrous iron is released through IREG1 it must be oxidised to ferric iron to facilitate its loading onto transferrin for onward transport in the circulation. Interestingly studies with the yeast ceruloplasmin homologue, Fet3p, have highlighted the requirement for ferrioxidase activity in iron accumulation by transferrin[81,82].
As stated above, the use of knockout mice has elegantly demonstrated the essential role of IREG1 in basolateral iron efflux[74]. In addition, a second genetic mutant mouse model-the sex-linked anaemia (sla) mouse-has highlighted the critical requirement for oxidation of iron leaving the enterocytes for normal iron homeostasis. The sla mouse develops a moderate to severe microcytic hypochromic anaemia[83]. It has been shown subsequently that these mice exhibit normal uptake of iron into enterocytes[84], but the subsequent release of iron into the circulation is diminished[85]. As a result, iron accumulates in enterocytes, and is lost when these cells are sloughed at the villus tip[86]. While the in vitro studies described earlier[77] used the ferrioxidase activity of ceruloplasmin to drive iron efflux, in the intestine the oxidation of iron is achieved by a ceruloplasmin homologue, hephaestin, which is also a multicopper ferrioxidase[87]. In the sla mouse, the hephaestin gene is defective leading to a truncated form of the protein[80], which is mislocalised within the enterocytes[88] and has reduced ferrioxidase activity[87].
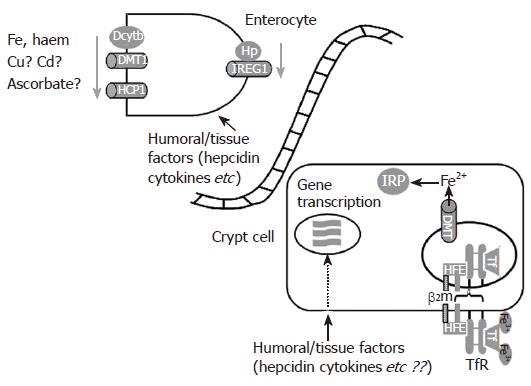
The regulation of intestinal iron absorption is complex and relies on mechanisms which sense dietary iron content as well as iron storage levels in the body and erythropoietic iron requirements (Figure 2). The iron regulatory hormone hepcidin is likely to be an important intermediate in signalling the storage and erythroid requirements and this aspect of iron homeostasis will be dealt with in an accompanying review[1].
In the healthy physiological state intestinal transporter expression will reflect body iron status exemplified by the circulating levels of iron bound to transferrin. Cells in the duodenal crypts of Lieberkühn express both Hfe[89,90], the protein mutated in more than 80% of haemochromatosis patients[91], and TfR on their basolateral surface. It is believed that Hfe binds to TfR regulating the rate at which transferrin-bound iron can enter the cell[92,93]. One suggestion is that the cellular iron concentration established as a result of this interaction ultimately determines the basal level of expression of the proteins involved in iron absorption in the mature absorptive cells in the upper third of the villus. Importantly, in a modification to this hypothesis, we propose that in response to humoral signals, such as hepcidin, iron transport[94] and transporter expression[95] in mature epithelial cells, can be modified rapidly without the need to re-programme the crypt cell sensing mechanism.
Rapid regulation of intestinal transporter expression in response to dietary factors is probably sensed by the villus enterocytes. More than half a century ago the “mucosal block” hypothesis was formulated following studies which demonstrated that a large oral dose of iron could reduce the absorption of a smaller dose administered several hours later[96,97]. It was argued that due to the short time interval between doses, the initial dose must be having a direct effect on the mature enterocytes rather than the crypt cells. Whether such a phenomenon occurs with meaningful dietary iron levels is not clear but this may be a considerable problem with supplemental iron levels[98]. Using the Caco-2 cell model, we have addressed the issue of whether non-haem iron can regulate iron transporter expression within a timescale and at concentrations that are consistent with digestion and absorption of a meal. We found that DMT1 (the IRE-containing isoforms) protein expression on the apical surface of these cells is decreased by iron concentrations as low as 20 μmol/L[64]. The decrease in DMT1 transporter expression was rapid, occurring within 1-4 h following the exposure to iron[99]. Further analysis revealed that DMT1 protein was internalised and targeted towards a late endosomal/lysosomal compartment. Interestingly, these iron-dependent effects were restricted to the apical uptake pathway-IREG1 protein expression was unaltered- and were fully reversible (DMT1 protein levels returned to their original basal levels within 4-8 h) following the removal of iron[99]. Our findings in this pertinent cell culture model are consistent with those observed in rats following oral gavage with an iron bolus[100-102] suggesting that the redistribution of DMT1 between different cellular compartments may be important physiologically for optimising iron absorption from a meal so that it matches better the body’s metabolic requirements.
In addition to trafficking of iron transport proteins, a number of intestinal iron metabolism genes can be regulated post-transcriptionally through interactions between cytosolic iron regulatory proteins (IRP) which bind to iron responsive elements (IRE), stem loop structures in either the 3′ or 5′ untranslated region (UTR) of several mRNA species, under conditions of cellular iron deficiency. TfR mRNA contains five IREs in its 3′UTR, and is stabilised following IRP binding as this blocks a target site for endonuclease activity[103-106]. Interestingly, two isoforms of DMT1 contain a single IRE in the 3′UTR[26]. While the DMT1 IRE can bind IRP in vitro[107,108], its role in regulating DMT1 expression remains to be fully determined.
In contrast to the reported role of the 3′IRE sequences in conferring mRNA stability, the expression of mRNAs possessing 5′IREs, such as ferritin, are poorly translated with cellular iron low. But, expression is increased by high iron levels in duodenal enterocytes[109]. This is because IRP/IRE binding blocks the association of the eukaryotic initiation factor complex to the 43S ribosomal unit[110]. Interestingly, IREG1 mRNA contains a single IRE in the 5′UTR[77,79]. However, the role of IRP/IRE interactions in the regulation of IREG1 transporter expression is even more controversial than its role in regulating DMT1 expression. Evidence suggests that the response to changes in iron status is tissue-specific-IREG1 expression in the liver[79] and lung[111] and in macrophages[112] is up-regulated by high iron whereas in the intestine expression is elevated by iron deficiency[77]. This may indicate that transcriptional, translational and post-translational processing of IREG1 varies between cell types[113]. Clearly, the mechanisms involved in iron-dependent regulation of IREG1 in the intestine require further attention.
While the majority of this review has focussed on the transport pathways in the enterocytes it is important to bear in mind that the intestinal cell population is a highly heterogeneous affair. It is likely, therefore, that cross-talk between the epithelial cells and other cell types, such as macrophages, neutrophils, intraepithelial lymphocytes etc will be important in the overall regulation of intestinal iron transport. One intriguing hypothesis in this regard is the possible physiological role of the pro-inflammatory cytokine TNFα in regulating intestinal iron transport. TNFα is not only synthesized by peripheral blood monocytes and macrophages in response to inflammatory stimuli, but is also released by intraepithelial lymphocytes (IEL) that reside within the intestine in response to high iron intakes[114]. These findings led to the formation of a hypothesis (named the piggyback-sensor model[115]) which suggested that interaction between Hfe in the developing enterocytes with specific epitopes on the IELs was essential for regulating local TNFα production. Once released, TNFα leads to iron deposition within intestinal enterocytes via a TNF receptor 2-dependent mechanism[116]. Further studies by our group[117] and others[118,119] have shown that TNFα has a direct influence on intestinal iron transporter expression and iron transport. These studies have opened the way for further investigations into the role of cell to cell cross-talk and the role of local tissue factors in regulating intestinal iron transport.
Clearly, our understanding of the molecular components of the intestinal iron transport pathway has increased exponentially in the last decade. However, there are still a number of important questions that remain unanswered: (1) How is iron shunted across the enterocytes from the apical pole to the basolateral membrane? There is some evidence for the presence of a tubulovesicular pathway. But, this work has largely been carried out in cell lines, and needs to be explored further in “normal” intestinal tissue. A role for calreticulin, a proposed component of the paraferritin pathway, remains a possibility though is still unproven. (2) What are the relative contributions of ferritin (and possibly lactoferrin) to iron nutrition? Could these iron sources be exploited for new supplemental therapies to treat iron deficiency? (3) Is there a role for cross-talk between enterocytes and other intestinal cell types in the local regulation on intestinal iron transport? If so, what are the cellular mechanisms involved? Are local tissue factors (such as TNFα) relevant physiologically in the control of iron absorption? (4) Hepcidin - how does it regulate intestinal iron transport? Is it an important physiological regulatory or is its main role in iron-related pathologies such as iron deficiency anaemia, haemochromatosis and anaemia of chronic disease?
The authors would like to thank the Biotechnology and Biological Research Council for continued financial support for their work on iron metabolism.
S- Editor Liu Y L- Editor Roberts SE E- Editor Li JL
| 1. | Darshan D, Anderson GJ. Liver-gut axis in the regulation of iron homeostasis. World J Gastroenterol. 2007;13:4737-4745. [PubMed] |
| 2. | Hallberg L, Bjørn-Rasmussen E, Howard L, Rossander L. Dietary heme iron absorption. A discussion of possible mechanisms for the absorption-promoting effect of meat and for the regulation of iron absorption. Scand J Gastroenterol. 1979;14:769-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 85] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Hallberg L, Brune M, Rossander L. Iron absorption in man: ascorbic acid and dose-dependent inhibition by phytate. Am J Clin Nutr. 1989;49:140-144. [PubMed] |
| 4. | Han O, Failla ML, Hill AD, Morris ER, Smith JC. Reduction of Fe(III) is required for uptake of nonheme iron by Caco-2 cells. J Nutr. 1995;125:1291-1299. [PubMed] |
| 5. | Glahn RP, Van Campen DR. Iron uptake is enhanced in Caco-2 cell monolayers by cysteine and reduced cysteinyl glycine. J Nutr. 1997;127:642-647. [PubMed] |
| 6. | Swain JH, Tabatabai LB, Reddy MB. Histidine content of low-molecular-weight beef proteins influences nonheme iron bioavailability in Caco-2 cells. J Nutr. 2002;132:245-251. [PubMed] |
| 7. | Poskitt EM. Early history of iron deficiency. Br J Haematol. 2003;122:554-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Sharma VR, Brannon MA, Carloss EA. Effect of omeprazole on oral iron replacement in patients with iron deficiency anemia. South Med J. 2004;97:887-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Raja KB, Simpson RJ, Peters TJ. Investigation of a role for reduction in ferric iron uptake by mouse duodenum. Biochim Biophys Acta. 1992;1135:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Riedel HD, Remus AJ, Fitscher BA, Stremmel W. Characterization and partial purification of a ferrireductase from human duodenal microvillus membranes. Biochem J. 1995;309:745-748. [PubMed] |
| 11. | Ekmekcioglu C, Feyertag J, Marktl W. A ferric reductase activity is found in brush border membrane vesicles isolated from Caco-2 cells. J Nutr. 1996;126:2209-2217. [PubMed] |
| 12. | McKie AT, Barrow D, Latunde-Dada GO, Rolfs A, Sager G, Mudaly E, Mudaly M, Richardson C, Barlow D, Bomford A. An iron-regulated ferric reductase associated with the absorption of dietary iron. Science. 2001;291:1755-1759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 734] [Cited by in RCA: 726] [Article Influence: 30.3] [Reference Citation Analysis (1)] |
| 13. | Gunshin H, Starr CN, Direnzo C, Fleming MD, Jin J, Greer EL, Sellers VM, Galica SM, Andrews NC. Cybrd1 (duodenal cytochrome b) is not necessary for dietary iron absorption in mice. Blood. 2005;106:2879-2883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 115] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Gunshin H, Mackenzie B, Berger UV, Gunshin Y, Romero MF, Boron WF, Nussberger S, Gollan JL, Hediger MA. Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature. 1997;388:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2383] [Cited by in RCA: 2299] [Article Influence: 82.1] [Reference Citation Analysis (0)] |
| 15. | Fleming MD, Trenor CC, Su MA, Foernzler D, Beier DR, Dietrich WF, Andrews NC. Microcytic anaemia mice have a mutation in Nramp2, a candidate iron transporter gene. Nat Genet. 1997;16:383-386. [PubMed] |
| 16. | Lucas ML, Cooper BT, Lei FH, Johnson IT, Holmes GK, Blair JA, Cooke WT. Acid microclimate in coeliac and Crohn's disease: a model for folate malabsorption. Gut. 1978;19:735-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | McEwan GT, Lucas ML, Denvir M, Raj M, McColl KE, Russell RI, Mathan VI. A combined TDDA-PVC pH and reference electrode for use in the upper small intestine. J Med Eng Technol. 1990;14:16-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Tandy S, Williams M, Leggett A, Lopez-Jimenez M, Dedes M, Ramesh B, Srai SK, Sharp P. Nramp2 expression is associated with pH-dependent iron uptake across the apical membrane of human intestinal Caco-2 cells. J Biol Chem. 2000;275:1023-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 209] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 19. | Griffiths WJ, Sly WS, Cox TM. Intestinal iron uptake determined by divalent metal transporter is enhanced in HFE-deficient mice with hemochromatosis. Gastroenterology. 2001;120:1420-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Gunshin H, Fujiwara Y, Custodio AO, Direnzo C, Robine S, Andrews NC. Slc11a2 is required for intestinal iron absorption and erythropoiesis but dispensable in placenta and liver. J Clin Invest. 2005;115:1258-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 307] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 21. | Fleming MD, Romano MA, Su MA, Garrick LM, Garrick MD, Andrews NC. Nramp2 is mutated in the anemic Belgrade (b) rat: evidence of a role for Nramp2 in endosomal iron transport. Proc Natl Acad Sci USA. 1998;95:1148-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 708] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 22. | Mims MP, Guan Y, Pospisilova D, Priwitzerova M, Indrak K, Ponka P, Divoky V, Prchal JT. Identification of a human mutation of DMT1 in a patient with microcytic anemia and iron overload. Blood. 2005;105:1337-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 150] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 23. | Beaumont C, Delaunay J, Hetet G, Grandchamp B, de Montalembert M, Tchernia G. Two new human DMT1 gene mutations in a patient with microcytic anemia, low ferritinemia, and liver iron overload. Blood. 2006;107:4168-4170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 24. | Iolascon A, d'Apolito M, Servedio V, Cimmino F, Piga A, Camaschella C. Microcytic anemia and hepatic iron overload in a child with compound heterozygous mutations in DMT1 (SCL11A2). Blood. 2006;107:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 25. | Lam-Yuk-Tseung S, Camaschella C, Iolascon A, Gros P. A novel R416C mutation in human DMT1 (SLC11A2) displays pleiotropic effects on function and causes microcytic anemia and hepatic iron overload. Blood Cells Mol Dis. 2006;36:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Lee PL, Gelbart T, West C, Halloran C, Beutler E. The human Nramp2 gene: characterization of the gene structure, alternative splicing, promoter region and polymorphisms. Blood Cells Mol Dis. 1998;24:199-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 238] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | Hubert N, Hentze MW. Previously uncharacterized isoforms of divalent metal transporter (DMT)-1: implications for regulation and cellular function. Proc Natl Acad Sci USA. 2002;99:12345-12350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 321] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 28. | Conrad ME, Umbreit JN. Pathways of iron absorption. Blood Cells Mol Dis. 2002;29:336-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 119] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 29. | Umbreit JN, Conrad ME, Hainsworth LN, Simovich M. The ferrireductase paraferritin contains divalent metal transporter as well as mobilferrin. Am J Physiol Gastrointest Liver Physiol. 2002;282:G534-G539. [PubMed] |
| 30. | Murray-Kolb LE, Welch R, Theil EC, Beard JL. Women with low iron stores absorb iron from soybeans. Am J Clin Nutr. 2003;77:180-184. [PubMed] |
| 31. | Davila-Hicks P, Theil EC, Lönnerdal B. Iron in ferritin or in salts (ferrous sulfate) is equally bioavailable in nonanemic women. Am J Clin Nutr. 2004;80:936-940. [PubMed] |
| 32. | Lönnerdal B, Bryant A, Liu X, Theil EC. Iron absorption from soybean ferritin in nonanemic women. Am J Clin Nutr. 2006;83:103-107. [PubMed] |
| 33. | Lonnerdal B, Kelleher SL, Theil EC. Uptake of iron from ferritin by Caco-2 cells. FASEB J. 2004;18:A761 (abstr). |
| 34. | Harrison PM, Arosio P. The ferritins: molecular properties, iron storage function and cellular regulation. Biochim Biophys Acta. 1996;1275:161-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 1849] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 35. | Theil EC. Iron, ferritin, and nutrition. Annu Rev Nutr. 2004;24:327-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 202] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 36. | Moss D, Fargion S, Fracanzani AL, Levi S, Cappellini MD, Arosio P, Powell LW, Halliday JW. Functional roles of the ferritin receptors of human liver, hepatoma, lymphoid and erythroid cells. J Inorg Biochem. 1992;47:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Takami M, Mizumoto K, Kasuya I, Kino K, Sussman HH, Tsunoo H. Human placental ferritin receptor. Biochim Biophys Acta. 1986;884:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Lönnerdal B, Iyer S. Lactoferrin: molecular structure and biological function. Annu Rev Nutr. 1995;15:93-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 490] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 39. | Kawakami H, Lönnerdal B. Isolation and function of a receptor for human lactoferrin in human fetal intestinal brush-border membranes. Am J Physiol. 1991;261:G841-G846. [PubMed] |
| 40. | Suzuki YA, Shin K, Lönnerdal B. Molecular cloning and functional expression of a human intestinal lactoferrin receptor. Biochemistry. 2001;40:15771-15779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 242] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 41. | Lopez V, Suzuki YA, Lönnerdal B. Ontogenic changes in lactoferrin receptor and DMT1 in mouse small intestine: implications for iron absorption during early life. Biochem Cell Biol. 2006;84:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 42. | Lönnerdal B, Bryant A. Absorption of iron from recombinant human lactoferrin in young US women. Am J Clin Nutr. 2006;83:305-309. [PubMed] |
| 43. | Hallberg L. Bioavailability of dietary iron in man. Annu Rev Nutr. 1981;1:123-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 309] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 44. | Wheby MS, Suttle GE, Ford KT. Intestinal absorption of hemoglobin iron. Gastroenterology. 1970;58:647-654. [PubMed] |
| 45. | Gräsbeck R, Kouvonen I, Lundberg M, Tenhunen R. An intestinal receptor for heme. Scand J Haematol. 1979;23:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Gräsbeck R, Majuri R, Kouvonen I, Tenhunen R. Spectral and other studies on the intestinal haem receptor of the pig. Biochim Biophys Acta. 1982;700:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 56] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 47. | Worthington MT, Cohn SM, Miller SK, Luo RQ, Berg CL. Characterization of a human plasma membrane heme transporter in intestinal and hepatocyte cell lines. Am J Physiol Gastrointest Liver Physiol. 2001;280:G1172-G1177. [PubMed] |
| 48. | Krishnamurthy P, Ross DD, Nakanishi T, Bailey-Dell K, Zhou S, Mercer KE, Sarkadi B, Sorrentino BP, Schuetz JD. The stem cell marker Bcrp/ABCG2 enhances hypoxic cell survival through interactions with heme. J Biol Chem. 2004;279:24218-24225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 487] [Cited by in RCA: 493] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 49. | Quigley JG, Yang Z, Worthington MT, Phillips JD, Sabo KM, Sabath DE, Berg CL, Sassa S, Wood BL, Abkowitz JL. Identification of a human heme exporter that is essential for erythropoiesis. Cell. 2004;118:757-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 317] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 50. | Shayeghi M, Latunde-Dada GO, Oakhill JS, Laftah AH, Takeuchi K, Halliday N, Khan Y, Warley A, McCann FE, Hider RC. Identification of an intestinal heme transporter. Cell. 2005;122:789-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 558] [Cited by in RCA: 488] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 51. | Qiu A, Jansen M, Sakaris A, Min SH, Chattopadhyay S, Tsai E, Sandoval C, Zhao R, Akabas MH, Goldman ID. Identification of an intestinal folate transporter and the molecular basis for hereditary folate malabsorption. Cell. 2006;127:917-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 616] [Cited by in RCA: 604] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 52. | Parmley RT, Barton JC, Conrad ME, Austin RL, Holland RM. Ultrastructural cytochemistry and radioautography of hemoglobin--iron absorption. Exp Mol Pathol. 1981;34:131-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 53. | Wyllie JC, Kaufman N. An electron microscopic study of heme uptake by rat duodenum. Lab Invest. 1982;47:471-476. [PubMed] |
| 54. | Raffin SB, Woo CH, Roost KT, Price DC, Schmid R. Intestinal absorption of hemoglobin iron-heme cleavage by mucosal heme oxygenase. J Clin Invest. 1974;54:1344-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 137] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 55. | Hunt JR, Roughead ZK. Nonheme-iron absorption, fecal ferritin excretion, and blood indexes of iron status in women consuming controlled lactoovovegetarian diets for 8 wk. Am J Clin Nutr. 1999;69:944-952. [PubMed] |
| 56. | Roughead ZK, Hunt JR. Adaptation in iron absorption: iron supplementation reduces nonheme-iron but not heme-iron absorption from food. Am J Clin Nutr. 2000;72:982-989. [PubMed] |
| 57. | Alvarez-Hernandez X, Smith M, Glass J. Regulation of iron uptake and transport by transferrin in Caco-2 cells, an intestinal cell line. Biochim Biophys Acta. 1994;1192:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 58. | Alvarez-Hernandez X, Smith M, Glass J. The effect of apotransferrin on iron release from Caco-2 cells, an intestinal epithelial cell line. Blood. 1998;91:3974-3979. [PubMed] |
| 59. | Nuñez MT, Tapia V. Transferrin stimulates iron absorption, exocytosis, and secretion in cultured intestinal cells. Am J Physiol. 1999;276:C1085-C1090. [PubMed] |
| 60. | Alvarez-Hernandez X, Smith M, Glass J. Apo-transferrin is internalized and routed differently from Fe-transferrin by caco-2 cells: a confocal microscopy study of vesicular transport in intestinal cells. Blood. 2000;95:721-723. [PubMed] |
| 61. | Ma Y, Specian RD, Yeh KY, Yeh M, Rodriguez-Paris J, Glass J. The transcytosis of divalent metal transporter 1 and apo-transferrin during iron uptake in intestinal epithelium. Am J Physiol Gastrointest Liver Physiol. 2002;283:G965-G974. [PubMed] |
| 62. | Moriya M, Linder MC. Vesicular transport and apotransferrin in intestinal iron absorption, as shown in the Caco-2 cell model. Am J Physiol Gastrointest Liver Physiol. 2006;290:G301-G309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Linder MC, Moriya M, Whon A, Kassa A, Gilley C. Vesicular transport of fe and interaction with other metal ions in polarized Caco2 cell monolayers. Biol Res. 2006;39:143-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 64. | Sharp P, Tandy S, Yamaji S, Tennant J, Williams M, Singh Srai SK. Rapid regulation of divalent metal transporter (DMT1) protein but not mRNA expression by non-haem iron in human intestinal Caco-2 cells. FEBS Lett. 2002;510:71-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 65. | Anderson GJ, Powell LW, Halliday JW. Transferrin receptor distribution and regulation in the rat small intestine. Effect of iron stores and erythropoiesis. Gastroenterology. 1990;98:576-585. [PubMed] |
| 66. | Anderson GJ, Walsh MD, Powell LW, Halliday JW. Intestinal transferrin receptors and iron absorption in the neonatal rat. Br J Haematol. 1991;77:229-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 67. | Levine DA, Wood JW. Immunolocalization of transferrin and transferrin receptor in mouse small intestinal absorptive cells. J Histochem Cytochem. 1990;38:851-858 DOI : 10.1177/38.6.2186090. |
| 68. | Jeffrey GP, Basclain KA, Allen TL. Molecular regulation of transferrin receptor and ferritin expression in the rat gastrointestinal tract. Gastroenterology. 1996;110:790-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 69. | Oates PS, Thomas C, Morgan EH. Transferrin receptor activity and localisation in the rat duodenum. Pflugers Arch. 2000;440:116-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 70. | O'Riordan DK, Sharp P, Sykes RM, Srai SK, Epstein O, Debnam ES. Cellular mechanisms underlying the increased duodenal iron absorption in rats in response to phenylhydrazine-induced haemolytic anaemia. Eur J Clin Invest. 1995;25:722-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 71. | O'Riordan DK, Debnam ES, Sharp PA, Simpson RJ, Taylor EM, Srai SK. Mechanisms involved in increased iron uptake across rat duodenal brush-border membrane during hypoxia. J Physiol. 1997;500:379-384. [PubMed] |
| 72. | Canonne-Hergaux F, Gruenheid S, Ponka P, Gros P. Cellular and subcellular localization of the Nramp2 iron transporter in the intestinal brush border and regulation by dietary iron. Blood. 1999;93:4406-4417. [PubMed] |
| 73. | Trinder D, Oates PS, Thomas C, Sadleir J, Morgan EH. Localisation of divalent metal transporter 1 (DMT1) to the microvillus membrane of rat duodenal enterocytes in iron deficiency, but to hepatocytes in iron overload. Gut. 2000;46:270-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 172] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 74. | Donovan A, Lima CA, Pinkus JL, Pinkus GS, Zon LI, Robine S, Andrews NC. The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab. 2005;1:191-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 779] [Cited by in RCA: 911] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 75. | Rindler MJ, Traber MG. A specific sorting signal is not required for the polarized secretion of newly synthesized proteins from cultured intestinal epithelial cells. J Cell Biol. 1988;107:471-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 89] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 76. | Halleux C, Schneider YJ. Iron absorption by CaCo 2 cells cultivated in serum-free medium as in vitro model of the human intestinal epithelial barrier. J Cell Physiol. 1994;158:17-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | McKie AT, Marciani P, Rolfs A, Brennan K, Wehr K, Barrow D, Miret S, Bomford A, Peters TJ, Farzaneh F. A novel duodenal iron-regulated transporter, IREG1, implicated in the basolateral transfer of iron to the circulation. Mol Cell. 2000;5:299-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1054] [Cited by in RCA: 1029] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 78. | Donovan A, Brownlie A, Zhou Y, Shepard J, Pratt SJ, Moynihan J, Paw BH, Drejer A, Barut B, Zapata A. Positional cloning of zebrafish ferroportin1 identifies a conserved vertebrate iron exporter. Nature. 2000;403:776-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1226] [Cited by in RCA: 1211] [Article Influence: 48.4] [Reference Citation Analysis (0)] |
| 79. | Abboud S, Haile DJ. A novel mammalian iron-regulated protein involved in intracellular iron metabolism. J Biol Chem. 2000;275:19906-19912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 943] [Cited by in RCA: 928] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 80. | Vulpe CD, Kuo YM, Murphy TL, Cowley L, Askwith C, Libina N, Gitschier J, Anderson GJ. Hephaestin, a ceruloplasmin homologue implicated in intestinal iron transport, is defective in the sla mouse. Nat Genet. 1999;21:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 775] [Cited by in RCA: 746] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 81. | de Silva D, Davis-Kaplan S, Fergestad J, Kaplan J. Purification and characterization of Fet3 protein, a yeast homologue of ceruloplasmin. J Biol Chem. 1997;272:14208-14213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 88] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 82. | Harris ZL, Davis-Kaplan SR, Gitlin JD, Kaplan J. A fungal multicopper oxidase restores iron homeostasis in aceruloplasminemia. Blood. 2004;103:4672-4673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 83. | Grewal MS. A sex−linked anemia in the mouse. Genet. Res. 1962;3:238-247. [RCA] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 84. | Manis J. Active transport of iron by intestine: selective genetic defect in the mouse. Nature. 1970;227:385-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 86. | Edwards JA, Hoke JE, Mattioli M, Reichlin M. Ferritin distribution and synthesis in sex-linked anemia. J Lab Clin Med. 1977;90:68-76. [PubMed] |
| 87. | Chen H, Attieh ZK, Su T, Syed BA, Gao H, Alaeddine RM, Fox TC, Usta J, Naylor CE, Evans RW. Hephaestin is a ferroxidase that maintains partial activity in sex-linked anemia mice. Blood. 2004;103:3933-3939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 119] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 88. | Kuo YM, Su T, Chen H, Attieh Z, Syed BA, McKie AT, Anderson GJ, Gitschier J, Vulpe CD. Mislocalisation of hephaestin, a multicopper ferroxidase involved in basolateral intestinal iron transport, in the sex linked anaemia mouse. Gut. 2004;53:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 89. | Parkkila S, Waheed A, Britton RS, Feder JN, Tsuchihashi Z, Schatzman RC, Bacon BR, Sly WS. Immunohistochemistry of HLA-H, the protein defective in patients with hereditary hemochromatosis, reveals unique pattern of expression in gastrointestinal tract. Proc Natl Acad Sci USA. 1997;94:2534-2539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 180] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 90. | Waheed A, Parkkila S, Saarnio J, Fleming RE, Zhou XY, Tomatsu S, Britton RS, Bacon BR, Sly WS. Association of HFE protein with transferrin receptor in crypt enterocytes of human duodenum. Proc Natl Acad Sci USA. 1999;96:1579-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 164] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 91. | Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava A, Dormishian F, Domingo R, Ellis MC, Fullan A. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996;13:399-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2676] [Cited by in RCA: 2550] [Article Influence: 87.9] [Reference Citation Analysis (0)] |
| 92. | Parkkila S, Waheed A, Britton RS, Bacon BR, Zhou XY, Tomatsu S, Fleming RE, Sly WS. Association of the transferrin receptor in human placenta with HFE, the protein defective in hereditary hemochromatosis. Proc Natl Acad Sci USA. 1997;94:13198-13202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 239] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 93. | Feder JN, Penny DM, Irrinki A, Lee VK, Lebrón JA, Watson N, Tsuchihashi Z, Sigal E, Bjorkman PJ, Schatzman RC. The hemochromatosis gene product complexes with the transferrin receptor and lowers its affinity for ligand binding. Proc Natl Acad Sci USA. 1998;95:1472-1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 604] [Cited by in RCA: 577] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 94. | Laftah AH, Ramesh B, Simpson RJ, Solanky N, Bahram S, Schümann K, Debnam ES, Srai SK. Effect of hepcidin on intestinal iron absorption in mice. Blood. 2004;103:3940-3944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 156] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 95. | Yamaji S, Sharp P, Ramesh B, Srai SK. Inhibition of iron transport across human intestinal epithelial cells by hepcidin. Blood. 2004;104:2178-2180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 95] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 96. | Hahn PF, Bale WF, Ross JF, Balfour WM, Whipple GH. Radioactive iron absorption by gastro-intestinal tract: influence of anemia, anoxia, and antecedent feeding distribution in growing dogs. J Exp Med. 1943;78:169-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 235] [Cited by in RCA: 196] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 97. | Stewart WB, Yuile CL, Claiborne HA, Snowman RT, Whipple GH. Radioiron absorption in anemic dogs; fluctuations in the mucosal block and evidence for a gradient of absorption in the gastrointestinal tract. J Exp Med. 1950;92:375-382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 98. | Benito P, House W, Miller D. Comparison of oral and intraperitoneal iron supplementation in anaemic rats: a re-evaluation of the mucosal block theory of iron absorption. Br J Nutr. 1998;79:533-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 99. | Johnson DM, Yamaji S, Tennant J, Srai SK, Sharp PA. Regulation of divalent metal transporter expression in human intestinal epithelial cells following exposure to non-haem iron. FEBS Lett. 2005;579:1923-1929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 100. | Oates PS, Trinder D, Morgan EH. Gastrointestinal function, divalent metal transporter-1 expression and intestinal iron absorption. Pflugers Arch. 2000;440:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 101. | Yeh KY, Yeh M, Watkins JA, Rodriguez-Paris J, Glass J. Dietary iron induces rapid changes in rat intestinal divalent metal transporter expression. Am J Physiol Gastrointest Liver Physiol. 2000;279:G1070-G1079. [PubMed] |
| 102. | Frazer DM, Wilkins SJ, Becker EM, Murphy TL, Vulpe CD, McKie AT, Anderson GJ. A rapid decrease in the expression of DMT1 and Dcytb but not Ireg1 or hephaestin explains the mucosal block phenomenon of iron absorption. Gut. 2003;52:340-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 135] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 103. | Casey JL, Hentze MW, Koeller DM, Caughman SW, Rouault TA, Klausner RD, Harford JB. Iron-responsive elements: regulatory RNA sequences that control mRNA levels and translation. Science. 1988;240:924-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 520] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 104. | Müllner EW, Kühn LC. A stem-loop in the 3' untranslated region mediates iron-dependent regulation of transferrin receptor mRNA stability in the cytoplasm. Cell. 1988;53:815-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 415] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 105. | Müllner EW, Neupert B, Kühn LC. A specific mRNA binding factor regulates the iron-dependent stability of cytoplasmic transferrin receptor mRNA. Cell. 1989;58:373-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 396] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 106. | Hentze MW, Kühn LC. Molecular control of vertebrate iron metabolism: mRNA-based regulatory circuits operated by iron, nitric oxide, and oxidative stress. Proc Natl Acad Sci. 1996;93:8175-8182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 993] [Cited by in RCA: 983] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 107. | Wardrop SL, Richardson DR. The effect of intracellular iron concentration and nitrogen monoxide on Nramp2 expression and non-transferrin-bound iron uptake. Eur J Biochem. 1999;263:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 108. | Gunshin H, Allerson CR, Polycarpou-Schwarz M, Rofts A, Rogers JT, Kishi F, Hentze MW, Rouault TA, Andrews NC, Hediger MA. Iron-dependent regulation of the divalent metal ion transporter. FEBS Lett. 2001;509:309-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 227] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 109. | Oates PS, Morgan EH. Ferritin gene expression and transferrin receptor activity in intestine of rats with varying iron stores. Am J Physiol. 1997;273:G636-G646. [PubMed] |
| 110. | Muckenthaler M, Gray NK, Hentze MW. IRP-1 binding to ferritin mRNA prevents the recruitment of the small ribosomal subunit by the cap-binding complex eIF4F. Mol Cell. 1998;2:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 190] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 111. | Yang F, Wang X, Haile DJ, Piantadosi CA, Ghio AJ. Iron increases expression of iron-export protein MTP1 in lung cells. Am J Physiol Lung Cell Mol Physiol. 2002;283:L932-L939. [PubMed] |
| 112. | Delaby C, Pilard N, Gonçalves AS, Beaumont C, Canonne-Hergaux F. Presence of the iron exporter ferroportin at the plasma membrane of macrophages is enhanced by iron loading and down-regulated by hepcidin. Blood. 2005;106:3979-3984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 205] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 113. | Canonne-Hergaux F, Donovan A, Delaby C, Wang HJ, Gros P. Comparative studies of duodenal and macrophage ferroportin proteins. Am J Physiol Gastrointest Liver Physiol. 2006;290:G156-G163. [PubMed] |
| 114. | Ten Elshof AE, Brittenham GM, Chorney KA, Page MJ, Gerhard G, Cable EE, Chorney MJ. Gamma delta intraepithelial lymphocytes drive tumor necrosis factor-alpha responsiveness to intestinal iron challenge: relevance to hemochromatosis. Immunol Rev. 1999;167:223-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 115. | Chorney MJ, Yoshida Y, Meyer PN, Yoshida M, Gerhard GS. The enigmatic role of the hemochromatosis protein (HFE) in iron absorption. Trends Mol Med. 2003;9:118-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 116. | Meyer PN, Gerhard GS, Yoshida Y, Yoshida M, Chorney KA, Beard J, Kauffman EJ, Weiss G, Chorney MJ. Hemochromatosis protein (HFE) and tumor necrosis factor receptor 2 (TNFR2) influence tissue iron levels: elements of a common gut pathway? Blood Cells Mol Dis. 2002;29:274-285. [PubMed] |
| 117. | Johnson D, Bayele H, Johnston K, Tennant J, Srai SK, Sharp P. Tumour necrosis factor alpha regulates iron transport and transporter expression in human intestinal epithelial cells. FEBS Lett. 2004;573:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 118. | Sharma N, Laftah AH, Brookes MJ, Cooper B, Iqbal T, Tselepis C. A role for tumour necrosis factor alpha in human small bowel iron transport. Biochem J. 2005;390:437-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 119. | Laftah AH, Sharma N, Brookes MJ, McKie AT, Simpson RJ, Iqbal TH, Tselepis C. Tumour necrosis factor alpha causes hypoferraemia and reduced intestinal iron absorption in mice. Biochem J. 2006;397:61-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |