Published online Aug 14, 2007. doi: 10.3748/wjg.v13.i30.4091
Revised: April 3, 2007
Accepted: April 26, 2007
Published online: August 14, 2007
AIM: To investigate if differences exist for patients’ gastroesophageal reflux as measured by the Bravo ambulatory esophageal pH system between d 1 and d 2.
METHODS: A retrospective study of 27 consecutive adult patients who underwent Bravo esophageal pH monitoring was performed. Patients underwent EGD under IV conscious sedation prior to Bravo placement. Acid reflux variables and symptom scores for d 1 were compared to d 2.
RESULTS: The mean doses of fentanyl and midazolam were 90.4 μg and 7.2 mg, respectively. D 1 results were significantly more elevated than d 2 with respect to total time pH < 4, upright position reflux, and mean number of long refluxes. No statistical difference was noted between the two days for supine position reflux, number of refluxes, duration of longest reflux, episodes of heartburn, and symptom score.
CONCLUSION: Patients undergoing Bravo esophageal pH monitoring in association with EGD and moderate conscious sedation experience significantly more acid reflux on d 1 compared to d 2. The IV sedation may be responsible for the increased reflux on d 1. Performed this way, 48-h Bravo results may not be entirely representative of the patients’ true GE reflux profile.
- Citation: Bechtold ML, Holly JSL, Thaler K, Marshall JB. Bravo (wireless) ambulatory esophageal pH monitoring: How do day 1 and day 2 results compare? World J Gastroenterol 2007; 13(30): 4091-4095
- URL: https://www.wjgnet.com/1007-9327/full/v13/i30/4091.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i30.4091
Ambulatory esophageal pH monitoring has for many years been a widely available method for quantifying esophageal acid exposure in patients with suspected gastroesophageal reflux disease (GERD)[1-3]. Until recently, the only way to perform ambulatory esophageal pH monitoring has been by the transnasal placement of a pH catheter probe, left in place for 24 h. Indications have included evaluation prior to anti-reflux surgery, refractory symptoms despite proton pump inhibitor (PPI) therapy, recurrent GERD symptoms following anti-reflux surgery, and continuation of atypical or extra-esophageal symptoms of GERD despite empirical therapy with a PPI.
At best, ambulatory pH monitoring with a catheter pH probe is moderately uncomfortable to patients, and there are some patients who are unable to tolerate the catheter altogether. Performance in adults has also traditionally required that esophageal manometry first be performed to localize the position of the lower esophageal sphincter relative to the nares. In addition, patients with nasally passed pH catheters often restrict their activities and diet, which has the potential to underestimate the amount of reflux they might have under more normal circumstances[2,4]. These various limitations of catheter-based ambulatory pH monitoring were major factors that led to the development of the Bravo pH monitoring system (Medtronic, Shoreview, MN), a catheter-less system that employs a radiotelemetry pH-sensing capsule clipped to the esophageal wall, which transmits pH data to a recorder worn by the patient. The Bravo delivery system was designed for either oral or nasal passage[5], though the capsule size may make transnasal passage difficult for some patients[6]. Compared to catheter-based pH monitoring, Bravo esophageal pH monitoring is better tolerated by patients and permits increased duration of pH recording[6-9].
Some of the technical details of Bravo pH capsule placement have not been standardized. For instance, the Bravo capsule may be clipped to the esophagus at the time that a patient undergoes diagnostic EGD utilizing conscious sedation. Alternatively, placement may be done on a different day, potentially without sedation, provided that the distance from the incisors (or the nares) to the GE junction is known based on measurements from previous esophageal manometry or endoscopy.
Most studies have examined Bravo esophageal pH results over an entire 48-h period without mentioning or giving specific d 1 and d 2 results. The few studies examining differences in d 1 and d 2 have varied results. Since patients in our practice undergo concomitant EGD under moderate sedation, we wondered if this sedation could potentially affect the d 1 results, possibly increasing gastroesophageal reflux on d 1. Our study compared d 1 with d 2 Bravo esophageal pH results.
We conducted a retrospective study of 27 consecutive patients age 15 years and older at the University of Missouri Hospital and Clinics who underwent 48-h Bravo ambulatory esophageal pH monitoring for suspected GERD off of any anti-reflux medications. The study was approved by the Institutional Review Board of our institution. All patients had stopped any proton pump inhibitors and H2-receptor antagonists seven days before placement of their Bravo pH capsules.
All patients in our study underwent EGD under IV conscious sedation with fentanyl and midazolam on the same day just prior to Bravo pH capsule placement. Four different endoscopists did the EGDs and Bravo placements. The amount of sedation given patients was at the discretion of the endoscopist. The Bravo capsule was placed 6 cm above the gastroesophageal junction in standard fashion[5,10]. We utilized vacuum suction applied at > 510 mmHg for 30 s prior to clipping the Bravo capsule. Immediately after deployment, direct visualization of the attached capsule was performed with the endoscope to confirm proper placement. Patients were instructed to wear the Bravo data recorder around their waist or to be within five feet of it at all times during the 48-h recording period. After recovery from their conscious sedation and discharge from our GI laboratory, patients were encouraged to resume their normal daily activities and usual diets. Patients were instructed to keep a diary to document when they ate, periods of sleep, and the occurrence of symptoms. They were also told to press a button on the data recorder when they perceived GERD-related symptoms.
After 48 h, patients returned to the GI laboratory, where they turned in their receivers and diaries. The data contained in the receiver was then downloaded to a computer, analyzed by Medtronic software, which then generated a summary report, which was reviewed and interpreted by one gastroenterologist (JBM). The computer analysis gave the percent of total time pH < 4, percent of upright time pH < 4, percent of supine time pH < 4, total number of reflux episodes, number of reflux episodes 5 min or longer, and the duration of the longest reflux episode for the entire 48-h recording period for d 1 and d 2 separately. A symptom score was calculated by dividing episodes of heartburn (or other reflux symptoms) which correlated with pH < 4 by the total number of heartburn episodes (or other reflux symptoms), and compared between d 1 and d 2.
Age of patients and doses of sedative medications were reported as mean ± SD. The reflux data collected from d 1 were statistically compared to d 2 to examine for significant differences. Differences were calculated for each variable comparing d 1 minus d 2. By this method, a positive value for the difference indicated that the value for d 1 was higher than the value for d 2. Since some of the measured variables were not normally distributed, the nonparametric Wilcoxon Signed Rank test was used to test the null hypothesis of no difference in the responses for the two days. In view of the large number of tests conducted, results were considered significant only for P values < 0.01. Ninety-five percent confidence interval estimates of the median difference between days were calculated. Analyses were done using the statistical software SAS (SAS Institute Inc., Cary, NC, USA).
Twenty-seven consecutive patients met entry criteria into the study (i.e. Bravo pH study done for suspected GERD with the study done off of anti-reflux medications). One patient was excluded after data analysis showed that their Bravo capsule had dislodged from the esophagus right after it had been placed. That left 26 patients for analysis as part of the study. This included six males (23%) and twenty females (77%), with a mean age of 47.6 ± 12.2 (range 15 to 67) years. Only three of the patients were less than 35 years of age (ages 15, 24 and 29 years). Five of the patients had a prior Nissen fundoplication, and one had a prior gastroplasty. The mean doses of sedative medications used in the patients were 90.4 ± 24.6 μg of fentanyl and 7.2 ± 2.8 mg of midazolam.
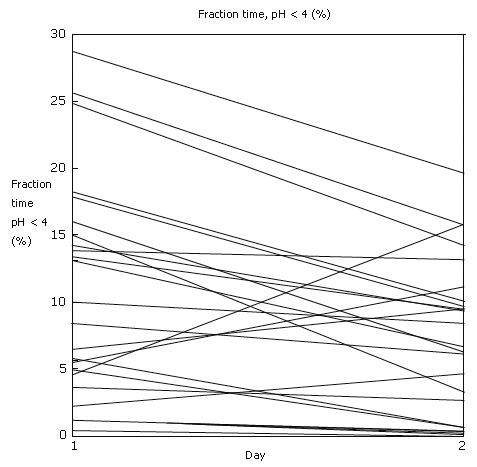
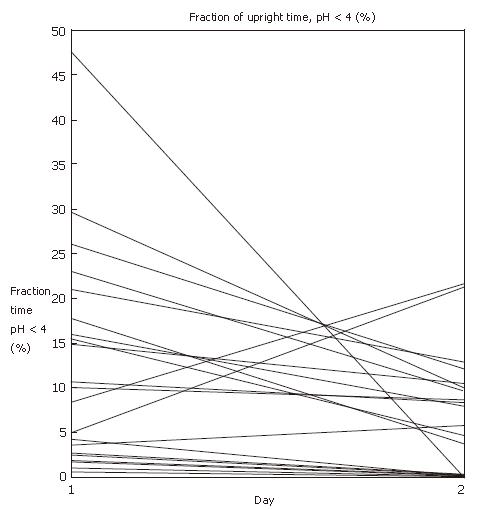
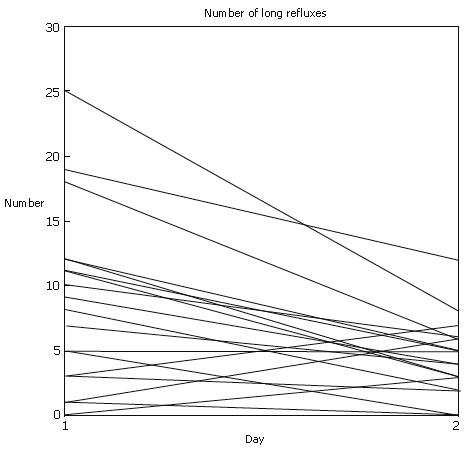
Table 1 shows the d 1 and d 2 results. Of the ten variables examined, significant differences (P < 0.01) were seen in three. More reflux was seen on d 1 as compared to d 2 as regards percent of total time pH <4 (P = 0.0049), percent of upright time pH < 4 (P = 0.0051), and the number of long reflux episodes (P = 0.0077). There were trends to more reflux on d 1 compared to d 2 in terms of the mean number of reflux episodes per day and the mean duration of long reflux episodes, but these differences were not statistically significant. There were no differences between d 1 and d 2 in terms of percent of supine time pH < 4, number of heartburn episodes, and symptom scores. Figure 1, Figure 2, Figure 3 plot the d 1 and d 2 values for the three variables that showed statistical differences.
| Variable | d 1(mean) | d 2(mean) | P-Value | 95% CI |
| Total time pH < 4 (%) | 10.4 | 7.1 | 0.0049 | 0.8-8.0 |
| Total time pH < 4-Upright (%) | 11.7 | 6.3 | 0.0051 | 1.6-7.9 |
| Total time pH < 4-Supine (%) | 9.4 | 10.0 | 0.8596 | |
| Mean number of reflux episodes (n) | 65.3 | 55.6 | 0.0257 | |
| Mean number of long refluxes (n) | 6.8 | 3.8 | 0.0077 | 0.0-6.0 |
| Mean duration of long refluxes (min) | 26.5 | 19.7 | 0.0617 | |
| Total heartburn episodes (n) | 6.2 | 8.0 | 0.2752 | |
| Heartburn episodes with pH < 4 (n) | 2.5 | 2.9 | 0.686 | |
| Symptom score | 0.323 | 0.254 | 0.1353 |
Since its introduction in 1974, ambulatory esophageal pH monitoring has helped to advance our knowledge regarding GERD, and has become an important tool in its diagnosis and management[1,11]. Until recently, the performance of the test has required the transnasal placement of a pH catheter probe, left in place for 24 h. In addition to being an uncomfortable test, patients commonly restrict their activities and diet, which has the potential to underestimate the amount of reflux that might occur under more typical lifestyle circumstances[2,4].
The recently introduced Bravo pH system, which uses a radiotelemetric capsule that is clipped to the esophageal wall, has been shown to be better tolerated by patients and to permit a more normal lifestyle during the study period[6,8,9,11]. Acid reflux monitoring results with Bravo should better reflect the real pattern of reflux in the day-to-day life of patients. The other potential major advantage of Bravo technology is that it permits longer periods of monitoring. While most Bravo studies currently are 48 h in duration, some have reported monitoring periods for as long as four days[12].
One of the most pressing issues relating to Bravo esophageal pH testing is that normal values are much less well established for this new technology as compared to conventional catheter-based pH monitoring[11]. Another relates to the lack of standardization as to whether the tests are performed without sedation on a day separate from endoscopic exams versus placing the pH capsule in association with EGD.
In our own practice, we have placed the Bravo capsule in association with the patient undergoing an EGD under moderate conscious sedation on the same day. Because of concern that d 1 was therefore not typical of our patients’ usual lifestyle, we decided to examine the amount of gastroesophageal reflux that our patients experienced on d 1 versus d 2. We hypothesized that patients might have more reflux on d 1 because of the effects of the endoscopy and sedation. Our findings confirmed this, showing significantly more reflux on d 1 than d 2 in terms of percent of total time pH < 4, percent of upright time pH < 4, and the number of long reflux episodes. There was no statistical difference in the supine time pH < 4, absolute number of reflux episodes per day, mean duration of long reflux episodes, number of heartburn episodes, and symptom scores. While we believe that the moderate intravenous sedation we gave to our patients to be responsible for the greater reflux on d 1, our study was not designed to clarify the specific mechanism. Our patients received a mean dose of 90 μg of fentany l and 7 mg of midazolam. While we did see more upright reflux on d 1 compared to d 2, there was no difference in supine reflux between the two days. A potential explanation for this observation is that the effects of their sedation may just be limited to the first 8 or 12 h after the endoscopy and Bravo capsule placement. Consequently, the medication effects may have worn completely off by the time the patient goes to bed that first night.
While most studies employing Bravo technology have reported overall 48-h pH results, some have compared d 1 with d 2. These latter studies have shown greatly varying findings. Similar to our study, Bhat et al[13] found more reflux on d 1 than d 2. Increased esophageal acid exposure during first six hours after capsule attachment was believed to have accounted for this finding. As in our series, patients in their study underwent EGD under conscious sedation just preceding Bravo placement, though they did not report specific medication dosages.
Most of the studies which have commented on d 1 versus d 2 reflux have reported no consistent differences. For instance, Prakash et al[7] said there were no differences in reflux variables between d 1 and d 2, though they did not report specific values. Patients in their study underwent EGD under conscious sedation, employing a variety of different medications, at the time of Bravo placement, though specific medication doses were not reported. Pandolfino et al[2] found no differences between d 1 and d 2 in their patients who also underwent same-day EGD with 50 to 75 mg of meperidine and 1 to 5 mg of midazolam. Tseng et al[14] found no consistent differences in their patient group who underwent same-day EGD with fentanyl and midazolam, though sedation doses were not given. Ahlawat et al[15] found no consistent differences in their group of patients who underwent same-day EGD under propofol.
Interestingly, one study found more reflux on d 2 than d 1[16]. Patients in this study did not undergo EGD or receive sedation on the day of their Bravo placements. Another study reported more reflux episodes on d 2 than d 1, but no consistent differences in other reflux variables[8]. Patients in this latter study underwent EGD on the day of Bravo placement, but no mention was given as to whether patients received sedation or the dose of sedative medications.
What should we make of the great variability that different studies have found between d 1 reflux versus d 2 reflux? For one thing, it points out that we need more study of the effects of the various protocols used to place Bravo pH capsules, and how they impact the d 1, d 2 and overall reflux results. It is entirely possible that there will be different normal ranges for reflux depending on whether the Bravo capsule is placed at the time of EGD with sedation versus it being placed without same-day endoscopy and sedation. Perhaps more emphasis should be given to placing the Bravo without endoscopy and sedation altogether. Alternatively, if endoscopy and sedation are to be used, we could look into doing longer studies, say 72 or 96-h studies, and then eliminating the d 1 data.
In conclusion, patients undergoing Bravo (wireless) ambulatory esophageal pH monitoring in our study showed increased acid reflux in the distal esophagus on d 1 as compared to d 2. We believe that this was the result of patients having undergone EGD with moderate sedation just prior to Bravo placement. However, given the variability as to what the literature reports in regards to d 1 versus d 2 reflux results, we believe that much more study of this phenomenon is needed as we apply the test clinically. We also believe that better establishment of normal results for Bravo pH monitoring is needed and will need to reflect the placement protocol used.
The authors thank Richard W Madsen, PhD for statistical support.
The recently introduced Bravo ambulatory esophageal pH system offers a catheter-less method of monitoring gastroesophageal (GE) reflux over an extended period and of correlating symptoms with acid reflux episodes. Limited data is available comparing d 1 with d 2 results. However, since patients may be sedated to clip the pH electrode to the esophagus, this sedation may potentially affect the d 1 results, possibly increasing GE reflux on d 1. This study compared d 1 with d 2 results.
The Bravo ambulatory esophageal pH system is a relatively new technology used to analyze GERD. This new system allows for 48 h of monitoring and is more comfortable to patients as compared to the 24 h transnasal pH catheter probe. However, limited data has suggested the results of the Bravo system vary over the two-day span. This study examines if a difference does exist in the patients’ reflux profile from d 1 to d 2 and postulates potential contributing factors.
The Bravo ambulatory esophageal pH system is a catheter-less system which is becoming more popular for the analysis of GERD.
This article demonstrates a significant difference in total time pH < 4, upright position reflux, and mean number of long refluxes between d 1 and d 2. The most likely contributing factor was the use of IV sedation prior to the attachment of the pH probe. Future studies may be performed to compare the Bravo capsule placement with and without prior IV sedation.
This retrospective study explores the effect of conscious sedation, performed before endoscopy and capsule placement, on 48-h Bravo pH findings. The Authors observed higher values of total acid exposure, upright reflux and number of long refluxes on d 1 vs d 2. Based on these retrospective data and on literature data, these differences may result from conscious sedation. Rationale and objectives of this study are very interesting, methods and presentation of data are reliable and allow relevant scientific conclusions.
S- Editor Zhu LH L- Editor Negro F E- Editor Wang HF
| 1. | Kahrilas PJ, Quigley EM. Clinical esophageal pH recording: a technical review for practice guideline development. Gastroenterology. 1996;110:1982-1996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 313] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | Pandolfino JE, Richter JE, Ours T, Guardino JM, Chapman J, Kahrilas PJ. Ambulatory esophageal pH monitoring using a wireless system. Am J Gastroenterol. 2003;98:740-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 344] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 3. | Wong WM, Bautista J, Dekel R, Malagon IB, Tuchinsky I, Green C, Dickman R, Esquivel R, Fass R. Feasibility and tolerability of transnasal/per-oral placement of the wireless pH capsule vs. traditional 24-h oesophageal pH monitoring--a randomized trial. Aliment Pharmacol Ther. 2005;21:155-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Fass R, Hell R, Sampliner RE, Pulliam G, Graver E, Hartz V, Johnson C, Jaffe P. Effect of ambulatory 24-hour esophageal pH monitoring on reflux-provoking activities. Dig Dis Sci. 1999;44:2263-2269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 103] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Chotiprashidi P, Liu J, Carpenter S, Chuttani R, DiSario J, Hussain N, Somogyi L, Petersen BT. ASGE Technology Status Evaluation Report: wireless esophageal pH monitoring system. Gastrointest Endosc. 2005;62:485-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Lutsi B, Hirano I. Ambulatory pH monitoring: new advances and indications. J Gastroenterol Hepatol. 2006;2:835-842. |
| 7. | Prakash C, Clouse RE. Value of extended recording time with wireless pH monitoring in evaluating gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2005;3:329-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Remes-Troche JM, Ibarra-Palomino J, Carmona-Sánchez RI, Valdovinos MA. Performance, tolerability, and symptoms related to prolonged pH monitoring using the Bravo system in Mexico. Am J Gastroenterol. 2005;100:2382-2386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Wenner J, Johnsson F, Johansson J, Oberg S. Wireless esophageal pH monitoring is better tolerated than the catheter-based technique: results from a randomized cross-over trial. Am J Gastroenterol. 2007;102:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Pandolfino JE. Bravo capsule pH monitoring. Am J Gastroenterol. 2005;100:8-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Holloway RH. Capsule pH monitoring: is wireless more? Gut. 2005;54:1672-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Hirano I, Zhang Q, Pandolfino JE, Kahrilas PJ. Four-day Bravo pH capsule monitoring with and without proton pump inhibitor therapy. Clin Gastroenterol Hepatol. 2005;3:1083-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Bhat YM, McGrath KM, Bielefeldt K. Wireless esophageal pH monitoring: new technique means new questions. J Clin Gastroenterol. 2006;40:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Tseng D, Rizvi AZ, Fennerty MB, Jobe BA, Diggs BS, Sheppard BC, Gross SC, Swanstrom LL, White NB, Aye RW. Forty-eight-hour pH monitoring increases sensitivity in detecting abnormal esophageal acid exposure. J Gastrointest Surg. 2005;9:1043-1051; discussion 1051-1052;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Ahlawat SK, Novak DJ, Williams DC, Maher KA, Barton F, Benjamin SB. Day-to-day variability in acid reflux patterns using the BRAVO pH monitoring system. J Clin Gastroenterol. 2006;40:20-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | des Varannes SB, Mion F, Ducrotté P, Zerbib F, Denis P, Ponchon T, Thibault R, Galmiche JP. Simultaneous recordings of oesophageal acid exposure with conventional pH monitoring and a wireless system (Bravo). Gut. 2005;54:1682-1686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |