Published online Jan 21, 2007. doi: 10.3748/wjg.v13.i3.483
Revised: November 3, 2006
Accepted: December 7, 2006
Published online: January 21, 2007
Spontaneous gastrojejunal fistula formation is an extremely rare complication of gastric ulcer disease. We report a 77-year old woman who presented with diffuse abdominal pain, weight loss, malaise, nausea, and occasional dark stools. Laboratory tests showed extreme hyposideremic anemia with inflammatory syndrome. In addition, biochemical parameters of malnourishment were presented. Upper endoscopy revealed the patent esophagus along the full length without any pathological changes. Large and deep ulceration with perforation in the small intestine was detected in the posterior gastric wall. The small intestine loop was reached by endoscope through spontaneously developed gastrojejunal fistula. Polytopic biopsies of described ulcerative change were carried out. Histopathologically reepithelialized ulcerous zone was seen in the gastric mucosa. Also, gastrojejunal fistula was visualized after wide opening of hepatogastric and gastrocolic ligament. Jejunal loop 25 cm from ligament of Treitz was attached to mesocolon and posterior gastric wall because of ulcer penetration. Postoperative course was uneventful. Per oral intake started on the 4th postoperative day, and the patient was discharged on the 8th postoperative day. In summary, this case indicates that persistent symptoms of peptic ulcer disease associated with nutritional disturbances may be caused by gastrojejunal fistula.
- Citation: Ćulafić ĐM, Matejić OD, Đukić VS, Vukčević MD, Kerkez MD. Spontaneous gastrojejunal fistula is a complication of gastric ulcer. World J Gastroenterol 2007; 13(3): 483-485
- URL: https://www.wjgnet.com/1007-9327/full/v13/i3/483.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i3.483
The inflammatory response to deeply penetrating peptic ulcer can lead to formation of a fistula between the stomach and duodenum or any structure nearby. Fistulae to the pancreatic duct, biliary tract, and colon have been described more commonly. Fistula arising between the stomach and duodenum called “double pylorus” is also a well-recognized complication of peptic ulcer disease[1,2]. Rarely, duodenal ulcer can penetrate to adjoin vascular structures and induce aorto-enteric or cavo-enteric fistula[3,4]. Such fistulae are usually characterized by less acute symptoms and in some instances represent a very challenging problem. In each case in which fistula is identified, cancer must be considered in differential diagnosis. In general, the small intestine is not found in proximity to the stomach or duodenum, protected as it is by the transverse colon and mesocolon. However, fistula to the small intestine has been reported to occur with typical ulcer symptoms[5]. We present a case of gastric ulcer disease complicated by gastrojejunal fistula.
A 77-year old woman was admitted for diffuse abdominal pain, weight loss, malaise, nausea, and occasional dark stools. Physical examination revealed malnourished, pale skin and apparent mucosa. The abdomen was soft (no local or rebound tenderness), diffusely painful, mostly in epigastrium. Laboratory test showed extreme hyposideremic anemia (HGB = 39 g/L, RBC=2.38 × 1012/L, HCT = 13.4%, MCV = 5.64 × 10-14 L, and serum Fe = 5.6 μmol/L) and inflammatory syndrome (ESR = 44 mm/h, fibrinogen = 7.4 g/L, C-reactive protein = 38.0 mg/L, and PLT = 813 × 109/L). In addition, biochemical parameters of malnourishment were presented (such as cholesterol level = 3.0 mmol/L, triglycerides = 0.6 mmol/L, total proteins = 55.5 g/L, and serum albumins = 29 g/L). Upper endoscopy revealed the patent esophagus along the full length without any pathological changes. Large and deep ulceration with perforation in the small intestine was detected in the posterior gastric wall (Figure 1). The small intestine loop was reached by endoscope through spontaneously developed gastrojejunal fistula (Figure 2). Antrum, pylorus, bulbus and postbulbar duodenum were normal in appearance. Polytopic biopsies of described ulcerative change were carried out. A histopathologically reepithelialized ulcerous zone was seen in the gastric mucosa. The signs of chronic antral atrophic inflammation were noted around the ulcerous mucosal parts, with strong activity, and hypersecretory and partially regenerative foveolar hyperplasia. H pylori test result was negative. The signs of non-specific active non-homogenous inflammatory infiltration with occasional sero-hemorrhagic superficial exudation were present in the mucosa of the small intestine. Real-time abdominal ultrasonography and computerized tomography findings were normal.
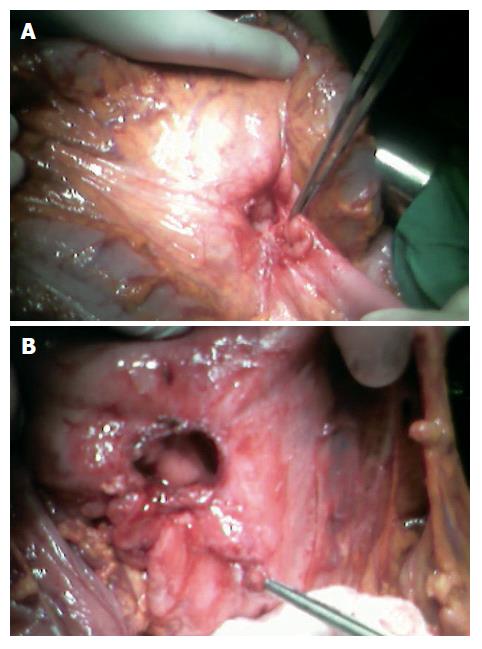
Upper central laparotomy was performed. A gastrojejunal fistula was visualized after wide opening of hepatogastric and gastrocolic ligament. The jejunal loop 25 cm from ligament of Treitz was attached to mesocolon and posterior gastric wall because of ulcer penetration (Figure 3A). After careful division of the jejunal loop from duodenojejunal reflection, the fistula was resected (Figure 3B). The jejunal loop defect was closed after wedge excision (histopathological verification ex tempore confirmed benign finding), with two-layer 4.0 vicryl (Ethicon) stitches. Subsequently, subtotal mastectomy was performed because of another giant gastric ulcer proximal to fistula. Gastrojejunostomy was created in the usual fashion (two layers of 4.0 vicryl) continuously with retro colic position of anatomists. After lavage and drainage of the right sub hepatic space, the abdominal wound was closed with Maxon-loop2 (Davis-Gecko). Postoperative course was uneventful. Per oral intake started on the 4th postoperative day, and the patient was discharged on the 8th postoperative day.
Spontaneous gastrojejunal fistula formation is rare and its differential diagnosis is multifactorial. Malignancy should be ruled out by careful endoscopic evaluation and appropriate imaging studies. Precise etiologic determination is necessary for proper management. In contrast to gastrocolic fistula, symptoms of the gastrojejunal fistula are those of the ulcer diathesis itself. However, if the target region of the fistula is very proximal, there is no short-circuiting of gastric contents; but if the target site is distal, the symptoms and nutritional disturbances may be similar to those observed with gastrocolic fistula[6].
Our patient manifested the symptoms of nutritional disturbances other than symptoms of ulceration, abdominal pains and recurring hemorrhage. Matsuoka et al[7] have described an 81-year old woman who had multiple recurrences of gastric ulcer after the left femoral head fracture, necessitating the mechanical bone head exchange operation. Gastro-endoscopic examination revealed a giant ulcer with long-axis diameter of more than 5 cm in the lesser curvature of stomach. Two weeks later, a fistula was formed between the stomach and jejunum. It was successfully managed by intravenous H2-antagonist and oral intake was restricted. Operative stress and application of ipriflavone appeared to have induced gastric ulcer recurrence. However, malnourishment of the patient contributed to the development of fistula between the stomach and jejunum which was very lean and had minimal mesenteric adipose tissue. Our patient was also lean with minimal mesenteric adipose tissue. However, risk factors, H pylori infection, nonsteroidal anti-inflammatory drug ingestion, and operative stress were absent. Indications for surgery are other complications such as free perforation, obstruction, refractory bleeding, or failure to heal with maximum medical therapy and persistent symptoms, rather than the fistula per se.
In case of our patient, surgical intervention was definitely indicated due to recurrent bleeding and symptoms of nutritional disturbances. In addition, gastrojejunal fistula secondary to gastric cancer is extremely rare. Choi et al[8] have described a 56-year-old man who was diagnosed with advanced gastric cancer. Fluoroscopic examination visualized two abnormal passages of contrast medium from the stomach: one to the colon, and the other to the jejunum. Fiber gastroscopy revealed a tumor in the greater curvature of stomach which appeared to penetrate in the colon, and a tumor in the antrum directly which invaded the jejunum. Souma et al[9] have described a 55-year old man seen for epigastralgia and weight loss. Barium radiography and endoscopic study revealed a gastric cancer associated with gastrojejunal fistula. At laparotomy, they found that the gastric tumor had extended to the transverse mesocolon, jejunum and pancreas, although no liver metastasis or peritoneal dissemination was seen. In addition, this patient, to their knowledge, is the fifth reported case in the world. In summary, this case indicates that persistent symptoms of peptic ulcer disease associated with nutritional disturbances may be caused by gastrojejunal fistula.
S- Editor Wang GP L- Editor Wang XL E- Editor Bi L
| 1. | Einhorn RI, Grace ND, Banks PA. The clinical significance and natural history of the double pylorus. Dig Dis Sci. 1984;29:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Hu TH, Tai DI, Changchien CS, Chen TY, Chang WC. Double pylorus: report of a longitudinal follow-up in two refractory cases with underlying diseases. Am J Gastroenterol. 1995;90:815-818. [PubMed] |
| 3. | Odze RD, Bégin LR. Peptic-ulcer-induced aortoenteric fistula. Report of a case and review of the literature. J Clin Gastroenterol. 1991;13:682-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Godwin TA, Mercer G, Holodny AI. Fatal embolization of intestinal contents through a duodenocaval fistula. Arch Pathol Lab Med. 1991;115:93-95. [PubMed] |
| 5. | Phifer TJ, Gladney JD, McDonald JC. Gastrojejunal fistula: a complication of peptic ulcer disease. South Med J. 1986;79:1015-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Tavenor T, Smith S, Sullivan S. Gastrocolic fistula. A review of 15 cases and an update of the literature. J Clin Gastroenterol. 1993;16:189-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Matsuoka M, Yoshida Y, Hayakawa K, Fukuchi S. Gastrojejunal fistula caused by gastric ulcer. J Gastroenterol. 1998;33:267-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Choi SW, Yang JM, Kim SS, Kang SH, Ro HJ, Song KS, Ha HK, Lim KW, Kim JS. A case of combined gastrojejunal and gastrocolic fistula secondary to gastric cancer. J Korean Med Sci. 1996;11:437-439. [PubMed] |
| 9. | Souma S, Ishimoto K, Ohyanagi H. A case of extended operation for gastric cancer accompanied with gastrojejunal fistula and pancreas invasion. Jpn J Gastroentrol Surg. 2004;37:1639-1643. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |