Published online Jan 21, 2007. doi: 10.3748/wjg.v13.i3.448
Revised: November 7, 2006
Accepted: December 4, 2006
Published online: January 21, 2007
AIM: To combine ultrasound-guided fine-needle aspiration (US-FNA) and Liu (Riu) stain to make a quick study on liver tumor lesions.
METHODS: Two hundred and twenty-eight aspirations from 232 patients were completely studied. The operator himself made the quick cytodiagnosis of US-FNA smear stained by Liu method within thirty minutes. The US-FNA specimen was also sent to the pathological department for cytological study and cellblock histology. The result of our Liu-stain quick cytodiagnosis in each patient was confirmed by the final cytopathological diagnosis from pathological report.
RESULTS: Among 228 samples, the quick cytodiagnosis revealed 146 malignancies, 81 benign lesions and one inadequate specimen. Cytopathological diagnosis from the pathological department revealed 150 malignancies, and 78 benign lesions. Four well-differentiated hepatocellular carcinomas (HCCs) were under-diagnosed by quick cytodiagnosis as benign and 3 benign lesions were over-diagnosed as well-differentiated HCCs. Compared with cytopathological diagnosis, quick cytodiagnosis correctly diagnosed 143 malignancies and 77 benign lesions. Except for the one inadequate specimen in quick cytodiagnosis, the accuracy of quick cytodiagnosis was 96.9% (220/227), and its sensitivity, specificity and positive and negative predictive values were 97.9%, 95.1%, 97.3% and 96.3%, respectively.
CONCLUSION: Liu-stain quick cytodiagnosis is a fast, convenient, safe and effective method for hepatologists in clinic practice to diagnose liver tumor. In few cases of well-differentiated HCC, Liu-stain quick cytodiagnosis has its limitation.
- Citation: Changchien CS, Wang JH, Lu SN, Hung CH, Chen CH, Lee CM. Liu-stain quick cytodiagnosis of ultrasound-guided fine needle aspiration in diagnosis of liver tumors. World J Gastroenterol 2007; 13(3): 448-451
- URL: https://www.wjgnet.com/1007-9327/full/v13/i3/448.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i3.448
Abdominal ultrasonography now is the first line to find liver tumor. Fine needle aspiration (FNA) is able to get tumor specimens for cytological interpretation[1]. Ultrasound-guided FNA (US-FNA) can get a correct specimen and provide a good diagnosis of liver tumor[2-4]. US-FNA is a safe and effective method for cytodiagnosis of liver tumor[2-4]. Tsou et al[5] reported that fine needle aspiration cytodiagnosis with Riu’s stain has its value in diagnosing liver tumors. The procedure of Liu (Riu) stain takes about two minutes. So, Liu stain for FNA smear is a quick method in cytological study. We tried to combine the ultrasound-guided FNA and Liu stain to shorten the time of cytodiagnosis of liver tumors.
From June 2004 to May 2005, 232 patients (128 males, 104 females) underwent US-FNA for liver nodular lesions with a diameter > 1 cm detected by abdominal sonography. US-FNA was done from one lesion in each patient who signed the informed consent. The diameter of lesions ranged 1-16 cm. The mean age of 232 patients was 56.9 (range 25-96) years. A total of 232 aspirations were done. The patients who had positive malignant result from the pathological department underwent tumor treatment modalities (such as pure ethanol injection or radiofrequency ablation for small tumors, or surgical resection of operable tumors, or transhepatic arterial embolization of larger tumors). The patients who had benign result from the pathological report were followed up for six to twelve months with no change in alpha-fetal protein level, ultrasound examination, and clinic course.
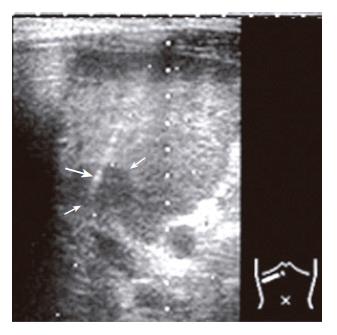
All US-FNAs were performed with Aloka SSD-680 or 2000 machine (Aloka Corp. Tokyo, Japan) using a 3.75-MHz lineal puncture probe or convex probe with a puncture adaptor. Needle aspiration was done under real-time US guidance with a 15-cm long 22-gauge Chiba needle (Hakko-Shoji, Tokyo) attached to a 20-mL syringe. The needle was advanced into the liver nodular lesion through the abdominal wall and liver parenchyma under the direct guidance of US (Figure 1). The piston of the syringe was pulled back and maintained in a maximal aspiration position to obtain the maximal negative pressure. The needle was quickly moved back and forth several times (about 3-5 passes) in the lesion under US observation. After this, the piston of the syringe was released and the pressure returned to normal, and the needle was withdrawn. The aspiration material was ejected and smeared onto glass slides (average 3-5 slides). One to two slides were stained by Liu stain solution and cytological reading was immediately done by the operator himself and Dr. Wang, and had cytological training at the Department of Pathology, Kurume University School of Medicine. The Liu stain solution for blood smear containing 2 kinds of solution, Liu A and B was used. The cytological smear for quick cytodiagnosis was directly (without dry-up) stained with Liu A for 30 s and then with Liu B for 1 min. After the stain solution was washed softly with water and the slide was dried by tissue paper, cytological reading was done, it took about 10 min. The cytological reader had the clinical data as assistant information. The total time of quick cytodiagnosis of US-FNA with Liu stain was within thirty minutes (including US-FNA procedure).
The remaining 2-3 slides were fixed in 95% ethanol and sent to the pathological department for hematoxylin and eosin (H & E) and/or papanicolaou staining. The remaining small, cohesive tissue fragments were also collected into a tube containing 10% neutral buffered formalin and processed for cell block histology study. The tissue was held using 2% agarose and paraffin-embeded. The pathologists studied the ethanol-fixed cytology and cellblock histology. The smear for quick cytodiagnosis was not sent for pathological study.
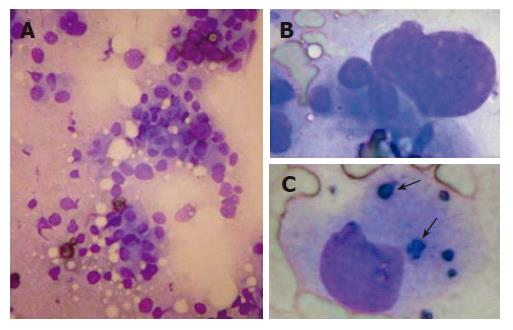
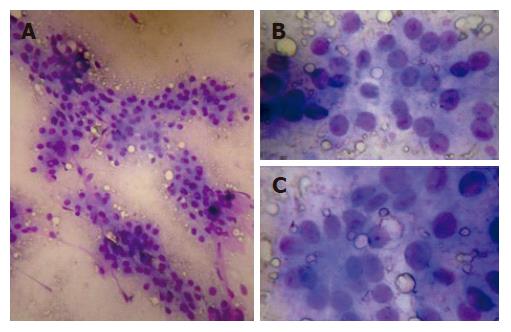
The quick cytodiagnosis was made depending on the findings on any slides. The cytological results were categorized into four groups: benign, suspicious for malignancy, positive for malignancy, and inadequate specimen. The positive malignancy encompassed both primary (hepatocellular carcinoma and cholangocarcinoma) and metastatic malignancies. The diagnosis of hepatocellular carcinoma (HCC) by quick cytology depended on the high cellularity with high nuclear/cytoplasmic ratios, polygonal outlines, dense granular cytoplasm, central nuclei and obvious morphologic kinship of tumor cells similar to ordinary hepatocytes. The characteristic findings in trabecular pattern and/or bile production (Figures 2 and 3) were also a clue to HCCs. The result of our Liu-stain quick cytodiagnosis in each patient was confirmed by the final cytopathological diagnosis from the pathological report. The diagnostic accuracy of quick cytodiagnosis was compared with that of cytopathological diagnosis. Sensitivity and specificity were calculated using conventional methods. Diagnostic accuracy was calculated as follows: (TP+TN)/(TP + TN+FP + FN), where TP = true positive, TN = true negative, FP = true positive and FN = false negative.
Four patients were excluded due to inadequate specimens for both quick Liu-stain cytodiagnosis and cytopathological diagnosis. Among the 228 patients enrolled, the quick cytodiagnosis revealed 142 malignancies (Figure 2), 4 suspicious malignancies, 81 benign lesions and one inadequate specimen. Cytopathological diagnosis from the pathological department revealed 150 malignancies, and 78 benign lesions. Four suspicious malignancies by quick cytodiagnosis were 2 suspicious HCCs and 2 necrotic tissues with ghost cells. The former two were finally diagnosed as HCC and the latter two as metastatic adenocarcinoma and lymphoma respectively. One inadequate specimen by quick cytodiagnosis was proved to be adenocarcinoma by cytopathological diagnosis.
A total of 146 cases were diagnosed as malignancy by quick cytodiagnosis. Among them, 115 cases were diagnosed as HCC (1.2 cm-over 10 cm in diameter). For the 115 HCCs by quick cytodiagnosis, 14 were initially diagnosed as well-differentiated HCCs (Figure 3). Among them, 5 were well-differentiated, 6 moderately-differentiated and 3 non-malignancies by cytopathological diagnosis. The diameter of these three non-malignancies ranged 1.2 cm-1.6 cm. Of the 81 benign lesions by quick cytodiagnosis, four were proved to be well-differentiated HCCs and one to be adenomyolipoma with fat by cytopathological diagnosis. The overall quick cytodiagnosis rate was 96.5% (143 + 77/228). Except for one inadequate specimen in quick cytodiagnosis, the accuracy of quick cytodiagnosis was 96.9% (220/227), and the sensitivity, specificity, positive and negative predictive values were 97.9%, 95.1%, 97.3% and 96.3%, respectively.
Among the 143 malignancies, 13 cases of malignancy by quick cytodiagnosis did not match the final cytopathological diagnosis. Four HCCs became adenocarcinoma, 3 adenocarcinomas became HCC, and 6 malignancies without identification of cell nature became three adenocarcinomas, two HCCs and one transitional cell carcinoma.
The final diagnosis of 150 cytopathological malignancies revealed 126 HCCs, 18 adenocarcinomas (including 3 cholangiocarcinomas), 2 lymphomas, 2 unidentified malignancies, one squamous cell carcinoma, and one transitional cell carcinoma. The 78 benign lesions included fibroconnective tissue (regeneration nodule), focal nodular hyperplasia (6 cases), abscess (8 cases), hemangioma (2 cases), and others (leiomyoma, adenomyolipoma). No complication in relation with quick cytodiagnosis was found in the study.
The specimen was sent to our pathological department, and cytopathological diagnosis was made by hematoxylin and eosin (H & E) and/or Papanicolaou staining and cell block histology. Special staining (in some cases) was also done to identify the nature of malignancy. It was reported that cytodiagnosis of liver tumors has good sensitivity and specificity[4], suggesting that our final results based on the cytopathological diagnosis from our pathological department are reliable.
In this study, the overall quick cytodiagnosis rate was 96.5% (143+77/228). The accuracy of quick cytodiagnosis in 227 cases of liver tumor was 96.9% (220/227), and its sensitivity, specificity, positive and negative predictive values were 97.9%, 95.1%, 97.3% and 96.3%, respectively. The results of Liu-stain quick cytodiagnosis were acceptable, compared with the reported sensitivity of 67%-100% and specificity of 80%-100%[1], and 93.3 % sensitivity and 100% specificity by Riu’s stain study[5]. The process of Liu stain on smears takes about 2 min. Including FNA aspiration procedure and cytological reading, the quick cytodiagnosis in this study took about thirty minutes to make a diagnosis. The procedure of cytodiagnosis was fast and effective in diagnosing liver tumors. It is very convenient for a hepatologist to diagnose liver tumors.
In most of our cases, Liu stain provided sufficient diagnostic elements, such as nuclear/cytoplasmic ratio, nuclear pattern, hyperchromatin, etc, to make a correct diagnosis of malignant or benign tumors. However, the nature of malignancy in quick cytodiagnosis was hard to identify in 13 cases, because special staining and cellblock histology were not available. This is the limitation of quick Liu stain cytodiagnosis. Although some limitations in diagnosing the nature of malignancies, quick cytodiagnosis can identify malignant from benign tumors except in some conditions such as well-differentiated HCCs.
In this series, incorrect diagnosis was made in 7 cases by quick cytodiagnosis. Four well-differentiated HCCs were under-diagnosed as benign tumors and 3 benign lesions were over-diagnosed as well-differentiated HCC. The mistake always occurs in the cases of well-differentiated HCC. Through the under-diagnosed cases of well-differentiated HCC in this study, we have got experience and increased our ability to diagnose well-differentiated HCC. Although the improvement in diagnosing well-differentiated HCC, we are still not able to make a perfect diagnosis of well-differentiated HCC, because the Liu stain alone cannot provide the complete information on the diagnosis of well-differentiated HCC. Boer et al[6] suggested that FNA cytodiagnosis of well-differentiated HCC should pay close attention to the architectural features and reticulin stain in both smears and cell blocks. The reticular pattern is an important criterion in diagnosing malignancy[7,8]. Without cell block and reticulin stain, the reticular pattern in aspiration cytological smear is hard to identify. Since the architecture features in Liu stain cytology show a poor reticular pattern, it was difficult to make a differentiation between the well-differentiated HCC and benign lesion in our 7 cases. In this study, although we made a correct diagnosis of 11 well-differentiated HCCs by quick cytodiagnosis, Liu-stain quick cytodiagnosis is not sufficient in diagnosing well-differentiated HCC.
Under ultrasound-guidance, FNA may correctly get specimens from small lesions less than 1 cm in diameter (Figure 1). FNA is also safer than core biopsy in getting specimens from liver to which it is difficult to approach. The Liu stain is a very simple and quick method in cytological study. In practice, we usually achieve one-shot aspiration to get specimens[5]. The quick Liu-stain is done immediately and the operator reads the cytological findings. If the specimen is inadequate or not informative, a second or third shot of aspiration should be done. The conventional cytopathology preparation cannot provide the opportunity to do a second aspiration. Liu-stain quick cytodiagnosis can minimize the failure of FNA aspiration. In this study, it was as lower as 2.2% (5/232). Therefore, Liu-stain quick cytodiagnosis may avoid inadequate specimens and improve cytodiagnosis. The process of Liu stain needs no air-drying of smears, the biosafety is stable, even in infective cases.
In conclusion, Liu-stain quick cytodiagnosis is a fast, safe, convenient and effective method for hepatologists to diagnose liver tumors and may provide a quick decision in HCC treatment. However, Liu-stain quick cytodiagnosis had its limitation in diagnosing well-differentiated HCC.
US-FNA cytodiagnosis of liver tumors has been confirmed, US-FNA Liu-stain cytodiagnosis makes a correct and quick cytodiagnosis of liver tumors.
Diagnosis of liver malignancy by quick cytodiagnosis should be performed as early as possible. When the specimen is inadequate or not informative, subsequent US-FNA aspiration should be performed to avoid the failure of cytodiagnosis.
The manuscript is interesting and could help obtain more informative histological data without loosing time and significant impact in clinical hepatology.
S- Editor Liu Y L- Editor Wang XL E- Editor Bi L
| 1. | Hertz G, Reddy VB, Green L, Spitz D, Massarani-Wafai R, Selvaggi SM, Kluskens L, Gattuso P. Fine-needle aspiration biopsy of the liver: a multicenter study of 602 radiologically guided FNA. Diagn Cytopathol. 2000;23:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Chiu KW, Chang-Chien CS, Chen L, Liaw YF. Ultrasonically-guided needle aspiration with preparation of cell blocks in the diagnosis of liver tumors. Hepatogastroenterology. 1994;41:30-33. [PubMed] |
| 3. | Tsai YY, Lu SN, Changchien CS, Wang JH, Lee CM, Eng HL, Chang WC. Combined cytologic and histologic diagnosis of liver tumors via one-shot aspiration. Hepatogastroenterology. 2002;49:644-647. [PubMed] |
| 4. | Kuo FY, Chen WJ, Lu SN, Wang JH, Eng HL. Fine needle aspiration cytodiagnosis of liver tumors. Acta Cytol. 2004;48:142-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Tsou MH, Lin YM, Lin KJ, Ko JS, Wu ML. Fine needle aspiration cytodiagnosis of liver tumors. Results obtained with Riu's stain. Acta Cytol. 1998;42:1359-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | de Boer WB, Segal A, Frost FA, Sterrett GF. Cytodiagnosis of well differentiated hepatocellular carcinoma: can indeterminate diagnoses be reduced? Cancer. 1999;87:270-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Zainol H, Sumithran E. Combined cytological and histological diagnosis of hepatocellular carcinoma in ultrasonically guided fine needle biopsy specimens. Histopathology. 1993;22:581-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Rapaccini GL, Pompili M, Caturelli E, Fusilli S, Trombino C, Gomes V, Squillante MM, Castelvetere M, Aliotta A, Grattagliano A. Ultrasound-guided fine-needle biopsy of hepatocellular carcinoma: comparison between smear cytology and microhistology. Am J Gastroenterol. 1994;89:898-902. [PubMed] |