INTRODUCTION
Since its first description in 1674[1], intussusception is considered a disease of infancy and early childhood and is the leading cause of acute abdomen in this age group, second only to appendicitis[2]. However, in approximately 5% of cases, it may also be encountered in adulthood accounting for 1% of adult intestinal obstructions[3,4].
Structural lesions are responsible for the majority of the cases in adults with only a minority being idiopathic in contrast to childhood intussusception[5]. In addition, the possibility of malignancy as the causative lesion should be considered in adult intussusception mandating surgical exploration in the majority of cases[6].
Adult patients with intussusception may present with acute abdominal pain necessitating surgical consultation (acute abdomen) but intermittent bowel obstruction with negative clinical and radiological findings is the usual case scenario[7]. The diagnosis can be elusive for a long period and is frequently established during laparotomy for the obstructive symptoms.
Neoplasia, both benign and malignant, is the leading cause of intestinal intussusception in adults[6]. Lipomas of the small intestine are rare benign tumors with no malignant potential, most commonly encountered incidentally, since they are usually asymptomatic. Symptomatic lipoma manifestations are hemorrhage or intestinal obstruction[8]. Due to their intramural location, lipomas can also serve as the leading point for intussusception.
We report on a case of an adult patient that presented to our department for investigation of recent episodes of lower gastrointestinal bleeding and colicky abdominal pain. The causative lesion proved to be a jejunojejunal intussusception due to a lipoma. A review of the literature is also performed regarding this rare association revealing the diagnostic and therapeutic debates that exist.
CASE REPORT
A 55-year-old man was admitted to our department with a 3-mo history of intermittent rectal bleeding. During this period, he had two episodes of hematochezia and acute abdominal pain located in the upper abdomen. During the first episode, physical and endoscopic (esophagogastroduodenoscopy and colonoscopy) examination revealed no pathology. The patient had no past history of peptic ulcer disease, alteration in bowel habits, melena or weight loss. Furthermore, diagnostic procedures including barium enema, abdominal computed tomography (CT), angiography, and serum tumor markers were normal. A decrease of hemoglobin levels from 14 to 12 g/dL was noted. He received no blood transfusion and was discharged.
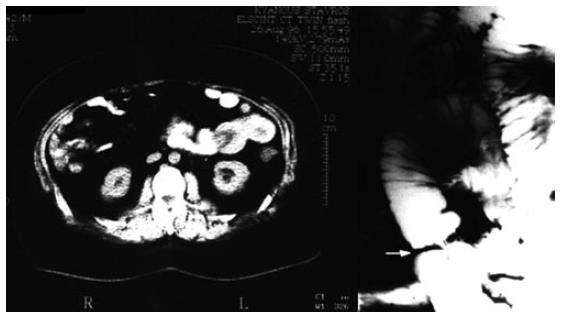
During the second episode, hemoglobin was 8.8 g/dL and the pain had become constant. Repetition of esophagogastroduodenoscopy and colonoscopy revealed no special findings. On the contrary, CT scan showed marked small bowel wall thickening and also detected a leading point with fat density (Figure 1). Small intestinal intussusception caused by a lipoma was considered to be a probable diagnosis. Abdominal conventional radiographs showed dilation of the jejunum and enteroclysis demonstrated an obstructing lesion (Figure 1).
Figure 1 Abdominal computed tomography showed an obstructive lesion of the jejunum with dilatation of the edematous adjacent bowel loops.
Enteroclysis showed a circular obstructive lesion of the jejunum with apple-core appearance. Close observation of the lesion shows the presence of radiation-lucent linear markings, with barium fillings on either side, projecting to the adjacent loop consistent with the walls of the intussusceptum.
At laparotomy, 40 cm distal to the ligament of Treitz, a jejunojejunal intussusception was identified. Manual reduction of the intussusception was performed. Palpation of an intraluminal mass forced us to make an enterotomy incision that revealed a 4 cm × 4 cm pedunculated lipoma (Figure 2). The presence of irreversible ischemia in a small portion of the intussusceptum necessitated segmental resection and primary anastomosis. Pathologic examination of the lesion confirmed our clinical impression of a lipoma. The postoperative period was uneventful and the patient was discharged on the seventh postoperative day. At 3 years following surgery he is free of symptoms without any evidence of recurrence.
Figure 2 A pedunculated lesion, measuring 4 cm × 4 cm, was the lead point of the intussusception.
The lesion was covered with mucosa and was composed of smooth submucosal fat. The clinical diagnosis of jejunal lipoma was subsequently confirmed at pathologic evaluation.
DISCUSSION
Intussusception in adulthood is unusual, with an incidence of approximately 2-3 cases per population of 1000000 per year[9]. There are distinctive features of adult intussusception compared to the childhood cases in causes, presentation and management.
Although childhood intussusception is considered idiopathic in 90% of cases, a demonstrable mechanical cause can be revealed in adult intussusception in over 90% of cases[3,5]. Moreover, the majority of intussusceptions in pediatric patients are seen during the first year of life and have no demonstrable structural cause while cases occurring later than the 5th year of life commonly have a causative lesion such as polyps, lymphoma, Meckel's diverticulum, or Henoch-Schonlein purpura[10].
Neoplasms are the most frequent causes of adult intussusception. The site of the intussusception is associated with the possibility of malignancy with colocolonic intussusception reported having a neoplasia as the lead point in 69% of cases and malignancy in 70% of them[6]. In the small bowel, neoplasia is also the leading causative lesion (57%) but malignancy is less frequent (30%)[6]. Adenocarcinoma is the most common malignant lesion in the colon whereas metastatic melanoma accounts for the majority of the malignant cases in the small bowel. Rarely, adenocarcinoma, lymphoma and leiomyosarcoma have been reported to be the leading point of small bowel intussusception[3,4]. Benign lesions acting as lead points of intussusceptions are most commonly pedunculated such as polyps, adenomatous in colon or Peutz-Jeghers in the small bowel, and lipomas. Less common aetiologies include postoperative factors (adhesions, suture lines, intestinal tubes) as well as Meckel's diverticulum, celiac sprue, HIV infection and intramural hematoma[3,4].
Lipomas of the gastrointestinal tract (GIT) are encountered with decreasing order of frequency in the colon (65%-75%), small intestine (20%-25%), stomach, and esophagus. They are the second most common benign small bowel tumors, leiomyomas being the most frequent. Their usual location in the small intestine is ileum (50%) while jejunum is the least common. The peak age of incidence is in the 6th-7th decades of life and it appears that females are more prone to lipomas. Malignant degeneration has never been reported.
GIT lipomas originate in the submucosa in 90% of cases and usually are solitary (85%-90%) with variable size ranging from 1 to 30 cm. In general, they form an intramural, discrete, smooth or lobulated, round or ovoid, soft mass covered by intact mucosa but occasionally they protrude subserosally. Although usually asymptomatic, they can give rise to symptoms related to their size and location. Lesions less than 1 cm are considered incapable of producing symptoms, while 75% of those greater than 4 cm are symptomatic. The symptoms of lipomas are the result of intussusception (16%-19% of lipoma-associated surgery), intestinal obstruction (occlusion of lumen by a large protruding lesion, retrograde prolapse of a polypoid lipoma of duodenum into pylorus, volvulus of the small intestine due to subserosal lipoma) and hemorrhage due to ulceration of the overlying mucosa caused by direct pressure from the lipoma or due to intussusception per se[8,11,12].
The unique features of adult intussusception compared to childhood type also involve symptomatology apart from aetiology. In contrast to the acute presentation of childhood intussusception, the adult type usually has a subacute or chronic onset. Fewer than 20% of cases present acutely with complete bowel obstruction. A palpable abdominal mass is present in only 7% to 42% of cases[4,11,12] . Therefore, a high index of suspicion is required. Long standing colicky abdominal pain, nausea, vomiting, distention and GIT bleeding are common but nonspecific. The diagnosis is often made at the time of laparotomy, since the presenting symptoms and signs are commonly non-diagnostic. According to the literature, only 32% to 50% of cases are diagnosed preoperatively, despite the evolution of imaging methods[3-5,13,14].
Imaging studies aid the diagnostic process. Plain abdominal films are non-specific and commonly demonstrate the presence of multiple air-fluid levels suggestive of mechanical obstruction. Rarely, a mass lesion or intraluminal air trapped between the walls of the intussusceptum and intussuscipiens (air crescent sign) can be shown in the plain abdominal radiograph but both findings lack specificity and sensitivity to diagnose intussusception[15]. Barium meal or enema may demonstrate the intussusception with the characteristic finding of the coiled spring appearance while the stretched spring sign has been associated with vascular compromise[16]. Barium examinations are restricted to the work up of a patient with subtle findings and should be avoided in the acute setting due to the risk of bowel rupture and barium peritonitis.
Ultrasound is usually the first modality to be recruited. It may evaluate acute abdominal complaints and bowel obstruction in both children and adults in the emergency room. Intussusception can be diagnosed based on the findings of the "target-like" sign, the "doughnut" sign when the transducer is oriented transversely to the intussusception, the "trident" sign when the transducer is positioned longitudinally, and the "pseudo kidney" sign when it is visualized obliquely [17-19]. Ultrasound has the advantages of being a fast and real time examination and, with the use of the color Doppler capabilities; it can be helpful in the determination of vascular obstruction. However, it is operator-dependent and the presence of distended bowel decreases the ability to demonstrate the site of the obstruction.
Computed tomography is the imaging method of choice for diagnosing intussusception[12]. Intussusception, on CT scans, appears as one of the following: (1) a mass lesion, representing a thickened segment of bowel, (2) a crescent-like, eccentric low-attenuation fatty mass, representing entrapped mesenteric fat, (3) a rim of contrast material encircling the intussusceptum, representing coating of the opposing bowel walls of the intussusceptum and intussuscipiens, (4) air bubbles peripheral to the upper part of the intussusception, which, like contrast material, may enter between the opposing bowel walls, and (5) a leading mass[12,20,21]. Furthermore, CT can give indirect signs of bowel ischemia such as the presence of intraperitoneal fluid and the status of fluid or gas collection in the intestinal wall. Although CT diagnosis of intussusception is relatively straightforward in the majority of cases, negative findings do not preclude intussusception. The sensitivity of CT scan to correctly diagnose intussusception has been reported from 71.4%-87.5% while its specificity in adults has been reported to be 100% as verified by the subsequent surgery [21-24]. However, particular caution should be instituted in the cases of incidentally discovered intussusception in an otherwise asymptomatic patient during abdominal CT examination. Follow up examinations rather than surgery should be employed in such cases as long as no lead point can be identified and the intussusception is less than 3.5 cm long[25,26].
A diagnostic technique that may be used, depending on the nature of symptoms, is capsule endoscopy. Although obstructive symptoms are contradictory to capsule endoscopy, this new modality for the evaluation of the small bowel could be very helpful in cases with long standing abdominal pain and negative radiologic examination, either CT or barium studies, to exclude the possibility of malignancy. Intussusception in capsule endoscopy has been reported to appear as a mass lesion of the small bowel[27,28]. The evaluation of incidentally discovered intussusception in adults for the presence of a structural lead point could be another indication for capsule endoscopy[29]. Moreover, enteroscopy with the push enteroscope can examine approximately 70-150 cm of the small bowel and double balloon enteroscopy can examine the full length of the small bowel both antegrade and retrograde[30]. Those techniques are advantageous over capsule endoscopy in that a biopsy specimen can be acquired from any lesion discovered and even endoscopic polypectomy is feasible through the working channel of these scopes [31].
The treatment plan for adult intussusception consists of segmental resection and primary restoration of the continuity of the gastrointestinal tract, given the high incidence of structural causes and the 6% to 30% malignant nature of the lesions in adults[3-7,12-16]. However, the extent of resection and whether or not the intussusception should be initially reduced remain controversial. The dangers of transperitoneal, vascular, and intraluminal seeding after exposing and handling friable and edematous malignant tissues has led many surgeons to advocate en bloc resection of the lesion. Others argue that routine en bloc resection might result in unnecessarily extensive bowel resection. All surgeons agree, though, that reduction should not be attempted if there are signs of irreversible bowel ischemia, inflammation or when malignancy is being suspected[1,13,31,32]. Intussusceptions of the duodenum or rectum are possible exceptions to en-block resection because reduction could result in preservation of the duodenum and avoidance of abdominoperineal resection, respectively.
We believe that reduction could also be tried safely in cases where diagnosis of a benign lesion has been reached preoperatively. In our case, CT density measurement had shown that the lead point was consistent with a lipoma of the small bowel. Although reduction was successful and enterotomy verified the CT findings, resection was deemed mandatory due to ischemia of a small portion of the small bowel wall that failed to reverse.