Published online Jun 28, 2007. doi: 10.3748/wjg.v13.i24.3380
Revised: March 15, 2007
Accepted: March 21, 2007
Published online: June 28, 2007
AIM: To clarify the relationship between circumferential resection margin status and local and distant recurrence as well as survival of patients with middle and lower rectal carcinoma. The relationship between circumferential resection margin status and clinicopathologic characteristics of middle and lower rectal carcinoma was also evaluated.
METHODS: Cancer specimens from 56 patients with middle and lower rectal carcinoma who received total mesorectal excision at the Department of General Surgery of Guangdong Provincial People’s Hospital were studied. A large slice technique was used to detect mesorectal metastasis and evaluate circumferential resection margin status.
RESULTS: Local recurrence occurred in 12.5% (7 of 56 cases) of patients with middle and lower rectal carcinoma. Distant recurrence occurred in 25% (14 of 56 cases) of patients with middle and lower rectal carcinoma. Twelve patients (21.4%) had positive circumferential resection margin. Local recurrence rate of patients with positive circumferential resection margin was 33.3% (4/12), whereas it was 6.8% (3/44) in those with negative circumferential resection margin (P = 0.014). Distant recurrence was observed in 50% (6/12) of patients with positive circumferential resection margin; conversely, it was 18.2% (8/44) in those with negative circumferential resection margin (P = 0.024). Kaplan-Meier survival analysis showed significant improvements in median survival (32.2 ± 4.1 mo, 95% CI: 24.1-40.4 mo vs 23.0 ± 3.5 mo, 95% CI: 16.2-29.8 mo) for circumferential resection margin-negative patients over circumferential resection margin-positive patients (log-rank, P < 0.05). 37% T3 tumors examined were positive for circumferential resection margin, while only 0% T1 tumors and 8.7% T2 tumors were examined as circumferential resection margin. The difference between these three groups was statistically significant (P = 0.021). In 18 cancer specimens with tumor diameter ≥ 5 cm 7 (38.9%) were detected as positive circumferential resection margin, while in 38 cancer specimens with a tumor diameter of < 5 cm only 5 (13.2%) were positive for circumferential resection margin (P = 0.028).
CONCLUSION: Our findings indicate that circumferential resection margin involvement is significantly associated with depth of tumor invasion and tumor diameter. The circumferential resection margin status is an important predictor of local and distant recurrence as well as survival of patients with middle and lower rectal carcinoma.
- Citation: Wu ZY, Wan J, Li JH, Zhao G, Peng L, Yao Y, Du JL, Liu QF, Wang ZD, Huang ZM, Lin HH. Study of circumferential resection margin in patients with middle and lower rectal carcinoma. World J Gastroenterol 2007; 13(24): 3380-3383
- URL: https://www.wjgnet.com/1007-9327/full/v13/i24/3380.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i24.3380
It is well known that middle and lower rectal carcinomas are of the most common carcinomas in China. However, even after undergoing radical resection of primary tumors and lymph nodes, about 5%-40% of patients with rectal carcinoma report with local recurrence[1-5]. It has been reported that residual mesorectal metastasis may be the most important factor of local recurrence[6,7]. In the current study, circumferential resection margin was detected by pathological observation in cancer specimens from 56 patients with middle and lower rectal carcinoma. The associations of circumferential resection margin status and local recurrence, distant recurrence as well as clinicopathologic characteristics of patients with middle and lower rectal carcinoma were investigated. The relationships between circumferential resection margin status and clinicopathologic characteristics of middle and lower rectal carcinoma were also evaluated.
Cancer specimens resected from 56 patients with middle and lower rectal carcinoma who received total mesorectal excision at the Department of General Surgery of Guangdong Provincial People’s Hospital from November 2001 to July 2003 were studied. There were 37 men and 19 women, ranging in age from 30 to 86 years, with a mean age of 60.5 years. None of these patients had received preoperative chemotherapy or radiotherapy. There were 26 lower rectal carcinomas and 30 middle rectal carcinomas. Patients with tumor diameter ≥ 5 cm were in 18 cases, with tumor diameter < 5 cm in 38 cases. Low anterior resection was performed in 40 patients, abdominal perineal resection in 16 patients. According to the Ming’s criteria, 15 tumors were classified as expansive type carcinomas, 41 tumors classified as infiltrative type carcinomas. TNM stage status: stageIin 5 patients, stage II in 22 patients, and stage III in 29 patients. There were 14 patients with poorly differentiated carcinoma, 37 patients with moderately differentiated carcinoma, and 5 patients with well-differentiated carcinoma.
Two pathologists who had no knowledge of the clinico-pathological data observed the specimens independently. If tumor cells were detected within 1 mm of the circumferential margin, the status was classified as positive circumferential resection margin[8].
Statistical analysis was performed by the Pearson Chi-square test to examine the associations of circumferential resection margin status and local recurrence, distant recurrence as well as clinicopathologic characteristics of patients with middle and lower rectal carcinoma. The relationship between circumferential resection margin status and survival of patients with middle and lower rectal carcinoma was evaluated by Kaplan-Meier survival analysis and log-rank test. Statistical significance was defined as P < 0.05.
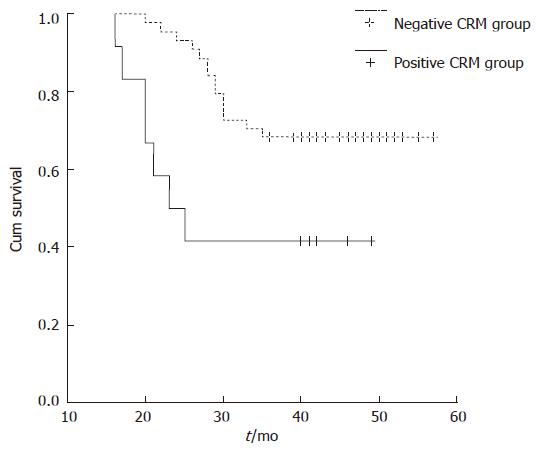
Local recurrence occurred in 12.5% (7 of 56 cases) of patients with middle and lower rectal carcinoma. Distant recurrence occurred in 25% (14 of 56 cases) of patients with middle and lower rectal carcinoma. Twelve patients (21.4%) had positive circumferential resection margin. Local recurrence rate of patients with positive circumferential resection margin was 33.3% (4/12), whereas it was 6.8% (3/44) in those with negative circumferential resection margin (P = 0.014). Distant recurrence was observed in 50% (6/12) of patients with positive circumferential resection margin; conversely, it was 18.2% (8/44) in those with negative circumferential resection margin (P = 0.024). Kaplan-Meier survival analysis showed significant improvements in median survival (32.2 ± 4.1 mo, 95% CI: 24.1-40.4 mo vs 23.0 ± 3.5 mo, 95% CI: 16.2-29.8 mo) for circumferential resection margin-negative patients over circumferential resection margin-positive patients (log-rank, P < 0.05) (Figure 1).
The circumferential resection margin involvement correlated significantly with depth of tumor invasion and tumor diameter. 37% T3 tumors were examined as positive circumferential resection margin, while only 0% T1 tumors and 8.7% T2 tumors were examined as circumferential resection margin. The difference between these three groups was statistically significant (P = 0.021). In 18 cancer specimens with tumor diameter ≥ 5 cm 7 (38.9%) were detected positive circumferential resection margin, while in 38 cancer specimens with tumor diameter < 5 cm only 5 (13.2%) were positive circumferential resection margin (P = 0.028). No significant correlations were found between circumferential resection margin involvement and other variables such as age (P = 0.815), gender (P = 0.961), diameter of tumor infiltration (P = 0.417), tumor differentiation (P = 0.074), Ming’s classification (P = 0.372) and lymph node metastases (P = 0.609) (Table 1).
| Circumferential resectionmargin involvement | ||||
| Variable | n | Negative (%) | Positive (%) | P |
| Gender | ||||
| Male | 37 | 29 (78.4) | 8 (21.6) | |
| Female | 19 | 15 (78.9) | 4 (21.1) | P = 0.961 |
| Age (yr) | ||||
| < 60 | 25 | 20 (80.0) | 5 (20.0) | |
| ≥ 60 | 31 | 24 (77.4) | 7 (22.6) | P = 0.815 |
| Superficial diameter (cm) | ||||
| < 5 | 38 | 33 (86.8) | 5 (13.2) | |
| ≥ 5 | 18 | 11 (61.1) | 7 (38.9) | P = 0.028 |
| Diameter of infiltration | ||||
| 1/4 | 8 | 7 (87.5) | 1 (12.5) | |
| 1/2 | 16 | 14 (87.5) | 2 (12.5) | |
| 3/4 | 18 | 14 (77.8) | 4 (22.2) | |
| 4/4 | 14 | 9 (64.3) | 5 (35.7) | P = 0.417 |
| Ming’s classification | ||||
| Expansive | 15 | 2 (13.3) | 13 (86.7) | |
| Infiltrative | 41 | 10 (24.4) | 31 (75.6) | P = 0.372 |
| Depth of invasion | ||||
| T1 | 6 | 6 (100.0) | 0 (0) | |
| T2 | 23 | 21 (91.3) | 2 (8.7) | |
| T3 | 27 | 17 (63.0) | 10 (37.0) | P = 0.021 |
| Histologic differentiation | ||||
| Well | 5 | 4 (80.0) | 1 (20.0) | |
| Moderate | 37 | 32 (86.5) | 5 (13.5) | |
| Poorly | 14 | 8 (57.1) | 6 (42.9) | P = 0.074 |
| Lymph node metastasis | ||||
| Positive | 29 | 22 (75.9) | 7 (24.1) | |
| Negative | 27 | 22 (81.5) | 5 (18.5) | P = 0.609 |
After radical resection of rectal carcinoma, the circum-ferential resection margin on the non-peritonealized surface of the resected specimen is of critical importance. 7.1%-35% of patients with rectal carcinoma were reportedly identified circumferential resection margin involvement[3,8-10]. In the present study, circumferential resection margin involvement in patients with middle and lower rectal carcinoma who underwent radical resection and total mesorectal excision were evaluated. 21.4% (12 of 56 cases) of patients had positive circumferential resection margin.
The correlation between circumferential resection margin status and local recurrence of patients with rectal carcinoma is still controversial presently[10-13]. Wibe et al[13] reported that positive circumferential resection margin had a significant and major prognostic impact on the rates of local recurrence of patients with rectal carcinoma who underwent total mesorectal excision. After a median follow-up of 29 (range 14-60) mo, the overall local recurrence rate was 7% (46 of 686 patients): 22% among patients with a positive resection margin and 5% in those with a negative margin. However, Luna-Perez[10] et al reported that circumferential resection margin involvement was not correlated significantly with local recurrence of patients with rectal adenocarcinoma (P = 0.33). Hall et al[11] reported that local recurrence rate of patients with positive circumferential resection margin was 15%, whereas it was 11% in those with negative circumferential resection margin. The difference between these two groups was not statistically significant (P = 0.38). Our results demonstrated that circumferential resection margin involvement had significant correlation with local recurrence of patients with middle and low rectal carcinoma. Local recurrence was more frequent in patients with positive circumferential resection margin (4 of 12 cases, 33.3%), compared with patients with negative circumferential resection margin (3 of 44 cases, 6.8%) (P = 0.014). We conclude that the circumferential resection margin status is an important predictor of local recurrence of patients with middle and low rectal carcinoma.
We also found that circumferential resection margin involvement was significantly correlated with distant recurrence and survival of patients with middle and low rectal carcinoma. Distant recurrence was observed in 50% (6/12) of patients with positive circumferential resection margin; conversely, it was 18.2% (8/44) in those with negative circumferential resection margin (P = 0.024). Kaplan-Meier survival analysis showed significant improvements in median survival for circumferential resection margin-negative patients over circumferential resection margin-positive patients (log-rank, P < 0.05). The consequences indicate that the circumferential resection margin status is an important predictor of local and distant recurrence as well as survival. For this reason, the circumferential resection margin status should be considered a major prognostic factor and should be validated in future trials as an early alternative clinical endpoint. Our results also support that histopathological examination of resected specimens must include careful assessment of the circumferential resection margin.
Many clinical studies reported the existence of circumferential resection margin involvement in patients with rectal carcinoma[8-15]. However, the relationships between circumferential resection margin status and clinicopathologic characteristics have not yet been explored. Therefore, the main objective of this study was to examine circumferential resection margin involvement and explore its relationship with clinicopathologic characteristics of patients with middle and lower rectal carcinoma. The circumferential resection margin involvement correlated significantly with depth of tumor invasion and tumor diameter. Positive circumferential resection margin was more frequent in T3 tumors (20 of 27 cases, 37%), compared with T2 tumors (2 of 23 cases, 8.7%) and T1 tumors (0 of 6 cases, 0%). The difference between these three groups was statistically significant (P = 0.021). 38.9 per cent (7 of 18 cases) of patients with tumor diameter ≥ 5 cm were detected as positive circumferential resection margin, while only 13.2% (5 of 38 cases) of patients with tumor diameter < 5 cm had circumferential resection margin involvement (P = 0.028). The result indicates that wider mesorectal excision should be followed in the management of patients with T3 tumors or tumor diameter ≥ 5 cm.
S- Editor Zhu LH L- Editor Alpini GD E- Editor Lu W
| 1. | Radice E, Dozois RR. Locally recurrent rectal cancer. Dig Surg. 2001;18:355-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Piso P, Dahlke MH, Mirena P, Schmidt U, Aselmann H, Schlitt HJ, Raab R, Klempnauer J. Total mesorectal excision for middle and lower rectal cancer: a single institution experience with 337 consecutive patients. J Surg Oncol. 2004;86:115-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, Abbott CR, Scott N, Finan PJ, Johnston D. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg. 2002;235:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 540] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 4. | Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B. Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group, Basingstoke Bowel Cancer Research Project. Lancet. 2000;356:93-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 591] [Cited by in RCA: 566] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 5. | Temple WJ, Saettler EB. Locally recurrent rectal cancer: role of composite resection of extensive pelvic tumors with strategies for minimizing risk of recurrence. J Surg Oncol. 2000;73:47-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998;133:894-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1037] [Cited by in RCA: 1054] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 7. | Wan J, Wu ZY, Du JL, Yao Y, Wang ZD, Lin HH, Luo XL, Zhang W. Mesorectal metastasis of middle and lower rectal cancer. Zhonghua WaiKe ZaZhi. 2006;44:894-896. [PubMed] |
| 8. | Hermanek P, Junginger T. The circumferential resection margin in rectal carcinoma surgery. Tech Coloproctol. 2005;9:193-199; discussion 193-199;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Tekkis PP, Heriot AG, Smith J, Thompson MR, Finan P, Stamatakis JD. Comparison of circumferential margin involvement between restorative and nonrestorative resections for rectal cancer. Colorectal Dis. 2005;7:369-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Luna-Pérez P, Bustos-Cholico E, Alvarado I, Maffuz A, Rodríguez-Ramírez S, Gutiérrez de la Barrera M, Labastida S. Prognostic significance of circumferential margin involvement in rectal adenocarcinoma treated with preoperative chemoradiotherapy and low anterior resection. J Surg Oncol. 2005;90:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Hall NR, Finan PJ, al-Jaberi T, Tsang CS, Brown SR, Dixon MF, Quirke P. Circumferential margin involvement after mesorectal excision of rectal cancer with curative intent. Predictor of survival but not local recurrence? Dis Colon Rectum. 1998;41:979-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 221] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol. 2002;26:350-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 558] [Cited by in RCA: 551] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 13. | Wibe A, Rendedal PR, Svensson E, Norstein J, Eide TJ, Myrvold HE, Søreide O. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002;89:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 522] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 14. | Mawdsley S, Glynne-Jones R, Grainger J, Richman P, Makris A, Harrison M, Ashford R, Harrison RA, Osborne M, Livingstone JI. Can histopathologic assessment of circumferential margin after preoperative pelvic chemoradiotherapy for T3-T4 rectal cancer predict for 3-year disease-free survival? Int J Radiat Oncol Biol Phys. 2005;63:745-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Laurent C, Nobili S, Rullier A, Vendrely V, Saric J, Rullier E. Efforts to improve local control in rectal cancer compromise survival by the potential morbidity of optimal mesorectal excision. J Am Coll Surg. 2006;203:684-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |