Published online Jun 21, 2007. doi: 10.3748/wjg.v13.i23.3268
Revised: April 1, 2007
Accepted: April 7, 2007
Published online: June 21, 2007
A 79-year-old previously healthy man presented with acute acalculous cholecystitis with obstruction of the biliary tract. He was successfully treated with antibiotics and percutaneous transhepatic gallbladder drainage, but returned to the hospital two days after discharge with a rare complication of this technique, biliopleural fistula. A thoracostomy tube was inserted to drain the pleural effusion, and the patient’s previous antibiotics reinstated. After two weeks of drainage and antibiotics, the fistula healed spontaneously without the need for further intervention.
- Citation: Lee MT, Hsi SC, Hu P, Liu KY. Biliopleural fistula: A rare complication of percutaneous transhepatic gallbladder drainage. World J Gastroenterol 2007; 13(23): 3268-3270
- URL: https://www.wjgnet.com/1007-9327/full/v13/i23/3268.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i23.3268
A biliopleural fistula (BF) can occur after events damaging both the diaphragm and adjacent liver (eg, rupture of a hydatid cyst, abscess), and is a rare complication of percutaneous transhepatic gallbladder drainage (PTGBD)[1-3].
We report a case of BF that developed after PTGBD was used to treat a patient with acute cholecystitis with biliary tract obstruction. Our experience, and a review of the literature, indicates that this complication can be managed non-surgically[4-8].
A 79-year-old previously healthy male was seen with complaints of right upper quadrant pain, loss of appetite, and fever (38.8°C). Physical examination revealed icteric sclera and positive Murphy’s sign. Heart rate was 92 beats/min, respiratory rate was 26 breaths/min. Blood count was remarkable for a white blood cell (WBC) count of 11 010 cells/μL with 87.7% neutrophils. Abdominal ultrasonography showed distention of the gallbladder with biliary sludge. Gallbladder distention was also seen on computed tomography (CT) imaging. Admission diagnosis was acute acalculous cholecystitis with biliary tree obstruction. Percutaneous gallbladder aspiration was attempted, however, the fluid was viscous and debris filled and obstructed the needle.
ERCP was considered, but the patient disclosed a history of allergic reaction to contrast media. Emergency laparoscopic cholecystectomy (LC) was considered. However, LC in cases of complete obstruction of the biliary tree is frequently associated with difficulty dissecting the cystic duct, high risk of biliary tract injury, high rate of conversion to open cholecystectomy, and a high incidence of postoperative bile leakage[9-11]. In order to avoid the aforementioned complications, drainage of the gallbladder was performed with consideration of LC after the patient’s condition had stabilized.
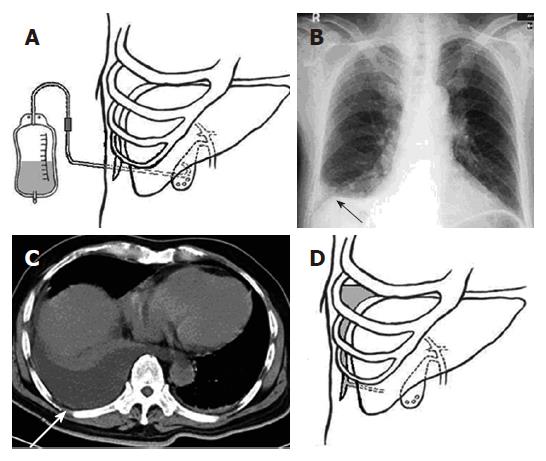
With the patient in the left decubitus position, a PTGBD tube was inserted at the mid-axillary line, through the liver and into the gallbladder cavity under direct ultrasound guidance by an attending radiologist with 7 years experience (Figure 1A). The ultrasound view was observed during inhalation. About 150 mL of bile was drained. Empiric antibiotic therapy of cefazolin 1 mg every 6 h, and gentamicin 80 mg every 12 h was administered. Culture was subsequently positive for Klebsiella pneumoniae, sensitive to the current antibiotic regime. The patient’s symptoms subsided by d 5 and he declined laparoscopic cholecystectomy. The PTGBD tube was clamped on d 8, antibiotics discontinued on d 10, and PTGBD tube was removed on d 12. The patient was discharged the following day.
Two days after discharge, the patient returned complaining of fever, dyspnea, and discomfort in the right chest. Physical examination revealed a temperature of 39.4°C, and decreased breath sounds in the right lower chest. Laboratory studies were remarkable for a WBC count of 11 450 cells/μL with 79.3% neutrophils, total bilirubin 1.1 mg/dL, and direct bilirubin 0.3 mg/dL. Chest roentgenogram showed blunting of the right costophrenic angle secondary to pleural effusion (Figure 1B). CT scan of the chest and abdomen revealed right pleural effusion and mild distention of the gallbladder (Figure 1C).
A percutaneous pleural drainage tube was inserted and approximately 550 mL of dark-green, viscous fluid was drained. A BF was suspected (Figure 1D). Biochemical studies of this fluid revealed: glucose 5 mg/dL, total bilirubin 16.7 mg/dL, direct bilirubin 9.7 mg/dL, and lactic dehydrogenase 670 mg/dL. A diagnosis of BF was made based on clinical findings and a pleural fluid/serum ratio of total bilirubin > 1.0[2].
The previous antibiotic regimen was administered and drainage maintained. The initial drainage rate was 100 to 150 mL/d, and diminished over 2 wk. Cultures of the fluid were positive for K. pneumoniae and E. coli. Chest roentgenogram 2 wk after admission was normal. The BF had spontaneously closed. The drainage tube was removed, antibiotics discontinued, and the patient was discharged.
PTGBD is often used in the treatment of obstructive gallbladder disease to relieve symptoms prior to laparoscopic cholecystectomy, or palliatively in patients who are poor candidates for surgery[1,9-12]. Because the catheter may pass through the pleural cavity before crossing the diaphragm en route to the gallbladder when a transhepatic approach is used, the potential for BF formation exists (Figure 1A). The likelihood of fistula development increases with duration of catheter placement and is the primary factor leading to fistula formation[2]. One study reported that fistula formation around a PTGBD occurs within 3 wk of placement[10]. Blockage of the biliary tree also increases the likelihood of fistula development due to increased bile pressure[2].
Early diagnosis of BF can reduce complications requiring surgery, and must be ruled out in any individual with previous PTGBD who develops a right pleural effusion[5]. Ultrasonography, CT, and radionuclide scan can identify bile collections, but cannot determine fistula location[5]. A definitive diagnosis requires thoracentesis to demonstrate bile in the pleural fluid and a total pleural bilirubin level higher than that in serum[2]. Empyema should also be ruled out[7].
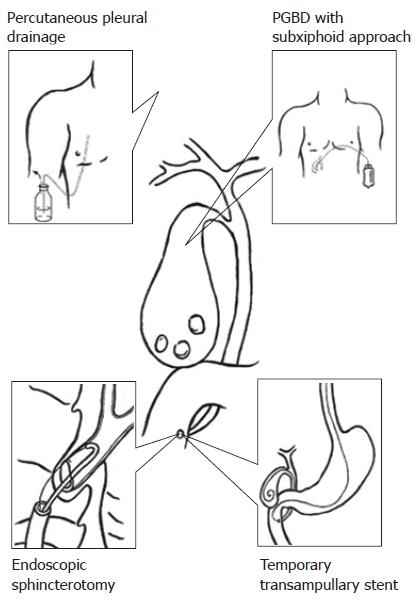
Bile drainage from the pleural cavity can be done conservatively with drainage tubes (Figure 2), or surgically. Flexible, small diameter catheters are less traumatic to insert and more comfortable for the patient, while large diameter catheters drain more rapidly. Currently, no data from randomized studies provide evidence for optimal size[8]. Surgery is required if the fistula is large or if diseased tissue must be debrided. If drainage is unsuccessful, the pressure gradient driving bile into the thorax should be relieved by opening the cystic duct, either through sphincterotomy and/or placement of a stent (Figure 2). Some authors recommend endoscopic sphincterotomy when symptoms persist more than 72 to 96 h after initial drainage[5]. Sphincterotomy reduces the mean basal sphincter of Oddi pressure to 1 ± 1 mmHg, favoring the flow of bile into the duodenum[5]. Stenting has been shown to significantly decrease morbidity and mortality compared to surgical intervention[4,5].
The failure of bile drainage in acalculous cholecystitis is thought to be due to ineffective contraction of gallbladder smooth muscle. The somatostatin analog, octreotide, has been used because it indirectly contracts gallbladder smooth muscle and relaxes the sphincter of Oddi. However, no randomized controlled trials using somatostatin or octreotide for this indication have been conducted[5,6]. The use of antibiotics as an adjunct to bile drainage is important because: (1) bacteria can enter along the catheter path, (2) bile is often infected, and (3) bile stasis encourages bacterial growth. Because the likelihood of fistula formation is related to the length of time the catheter is in place, prevention relies on decreasing the duration of time the catheter is in place.
Our patient was a 79-year-old male who suffered one episode of acute cholecystitis with biliary tract obstruction. The delay in performing a LC due to the high risk of complications, including conversion to open cholecystectomy, was warranted. We employed the transhepatic approach for drainage because of our experience with this procedure and its desirable angle of entry into the gallbladder. BF develops in a small percentage, but considerable number, of patients who undergo the PTGBD. Decreasing the length of time the catheter is in place will reduce the likelihood of fistula formation; however, a stepwise approach to management is important. Conservative treatment including pleural drainage, prophylactic antibiotics, and possible use of somatostatin or an analog should be considered. Sphincterotomy and stenting should be considered if conservative treatment is ineffective. Surgical intervention is warranted if the above stated measures fail.
S- Editor Zhu LH L- Editor Alpini GD E- Editor Ma WH
| 1. | Herschman Z, Amin D, Lehrfield A. Bilious pleural effusion as a complication of attempted percutaneous biliary drainage. Crit Care Med. 1991;19:128-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Strange C, Allen ML, Freedland PN, Cunningham J, Sahn SA. Biliopleural fistula as a complication of percutaneous biliary drainage: experimental evidence for pleural inflammation. Am Rev Respir Dis. 1988;137:959-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Oparah SS, Mandal AK. Traumatic thoracobiliary (pleurobiliary and bronchobiliary) fistulas: clinical and review study. J Trauma. 1978;18:539-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Chua HK, Allen MS, Deschamps C, Miller DL, Pairolero PC. Bronchobiliary fistula: principles of management. Ann Thorac Surg. 2000;70:1392-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Singh B, Moodley J, Sheik-Gafoor MH, Dhooma N, Reddi A. Conservative management of thoracobiliary fistula. Ann Thorac Surg. 2002;73:1088-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Ong M, Moozar K, Cohen LB. Octreotide in bronchobiliary fistula management. Ann Thorac Surg. 2004;78:1512-1513; author reply 1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Light RW. Pleural effusions after coronary artery bypass graft surgery. Curr Opin Pulm Med. 2002;8:308-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Davies RJ, Gleeson FV. The diagnosis and management of pleural empyema. Curr Opin Infect Dis. 1998;11:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Kim KH, Sung CK, Park BK, Kim WK, Oh CW, Kim KS. Percutaneous gallbladder drainage for delayed laparoscopic cholecystectomy in patients with acute cholecystitis. Am J Surg. 2000;179:111-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Watanabe Y, Sato M, Abe Y, Iseki S, Sato N, Kimura S. Preceding PTGBD decreases complications of laparoscopic cholecystectomy for patients with acute suppurative cholecystitis. J Laparoendosc Surg. 1996;6:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Early scheduled laparoscopic cholecystectomy following percutaneous transhepatic gallbladder drainage for patients with acute cholecystitis. Surg Endosc. 2002;16:1704-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Verbanck JJ, Demol JW, Ghillebert GL, Rutgeerts LJ, Surmont IP. Ultrasound-guided puncture of the gallbladder for acute cholecystitis. Lancet. 1993;341:1132-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Soehendra N, Binmoeller KF, Seifert H, Schreiber HW. Sphincterotomy. Therapeutic Endoscopy Color Atlas of Operative Techniques for the Gastrointestinal Tract. 1st ed. New York: Thieme Med Pub 1998; 105-117. |
| 14. | Soehendra N, Binmoeller KF, Seifert H, Schreiber HW. Biliary Stent Drainage. Therapeutic Endoscopy Color Atlas of Operative Techniques for the Gastrointestinal Tract. 1st ed. New York: Thieme Med Pub 1998; 135-156. |