Published online May 28, 2007. doi: 10.3748/wjg.v13.i20.2855
Revised: March 3, 2007
Accepted: March 8, 2007
Published online: May 28, 2007
AIM: To prove that the terminal ileum is intussuscepted into the cecum creating the ileocecal junction, contrary to previous valvular concept which has been widely believed.
METHODS: This study is based on gross and microscopic examinations of fresh specimens derived from colonic operations (right hemicolectomy or subtotal colectomy). Data compiled from observing and dissecting of specimens of seven patients are used to examine both gross and microscopic appearance of ileocecal junction.
RESULTS: Intussusception of the terminal ileum was found in every specimen. However, the length of intussusception was different in each specimen.
CONCLUSION: Gross and microscopic appearance studies suggest that the terminal ileum is intussuscepted into the cecum.
- Citation: Awapittaya B, Pattana-arun J, Tansatit T, Kanjanasilpa P, Sahakijrungruang C, Rojanasakul A. New concept of ileocecal junction: Intussusception of the terminal ileum into the cecum. World J Gastroenterol 2007; 13(20): 2855-2857
- URL: https://www.wjgnet.com/1007-9327/full/v13/i20/2855.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i20.2855
The anatomy of the ileocecal junction (IC junction) was first described as ileocecal valve concept; fold of mucosa into the lumen of cecum[1,2]. Later studies described a thickened muscular eminence, and the concept of sphincter at IC junction was emerged. Manometric studies had shown characteristic of IC junction[3-8]. A four-centimeter zone of elevated pressure was demonstrated at the junction[3]. Physiological study of the IC junction has suggested that "ceco-ileal excitatory reflex", initiated by Ileal distension stimulate the reflex relaxation of IC junction and cecal, is the main mechanism in allowing the chime to pass into the cecum. Cecal distension appears to evoke reflex ileal and IC junction, thus preventing ceco-ileal reflux[4]. Kumar and Phillips[1,8] proposed that competency of IC junction is facilitated by angulation of the ileum on the cecum, an anatomic arrangement which maintained by external (superior and inferior ileocecal) ligaments.
However, from our observation, during the operation and examination of specimens reveal that the appearance of ileocecal junction as the terminal ileum was intussuscepted into the cecum, of which is the point that this study attempts to prove.
Seven specimens of colon and terminal ileum (including ileocecal junction) from seven patients were collected for this study.
(1) Specimens derived from right hemicolectomy or extended right hemicolectomy; (2) Specimens derived from subtotal colectomy.
(1) Specimens of patients who had disease or pathology of ileocecal junction; (2) Specimens of patients who underwent appen-dectomy.
Gross anatomy examination is conducted to investigate the possibility of terminal ileum intussuscepted into the cecum. In case of detecting the intussusception, the length of the terminal ileum which is intussuscepted in to the cecum will be measured.
Microscopic examination with H&E staining is conducted to determine the intussusception of terminal ileum into the cecum by dissecting specimens from the ileocecal junction area.
Seven specimens from seven patients were used in this study. Details of patients are shown in Table 1.
| Patient’s diagnosis | Age (yr) | Gender | Operation |
| Colonic cancer of the ascending colon | 58 | Male | Right hemicolectomy |
| Colonic cancer of the hepatic flexure | 64 | Male | Right hemicolectomy |
| Colonic cancer of the sigmoid colon | 53 | Male | Subtotal colectomy |
| Bleeding diverticulosis | 70 | Female | Subtotal colectomy |
| Colonic cancer of the hepatic flexure | 74 | Male | Extended right hemicolectomy |
| Colonic cancer of the hepatic flexure | 64 | Female | Extended right hemicolectomy |
| Colonic cancer of the transverse colon | 64 | Male | Extended right hemicolectomy |
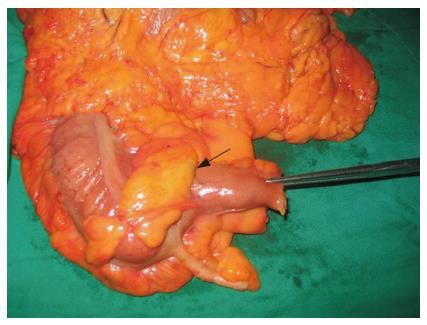
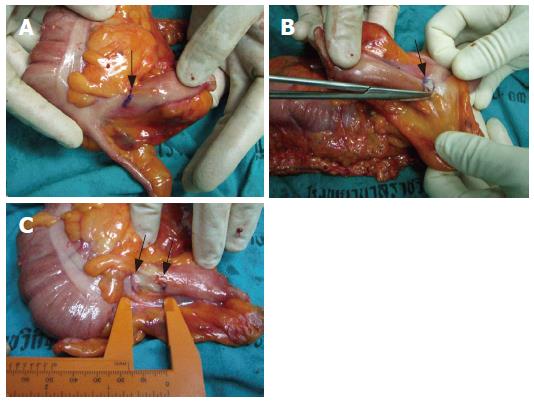
Findings of gross appearance reveal that the terminal ileum is intussuscepted into the cecum in all seven specimens (Figures 1 and 2). However, the length of the intussusception is different as shown in Table 2.
| Specimen | Intussusception | Length of intussusception (cm) |
| Patient 1’s specimen | Yes | 1.6 |
| Patient 2’s specimen | Yes | 1 |
| Patient 3’s specimen | Yes | 0.5 |
| Patient 4’s specimen | Yes | 2 |
| Patient 5’s specimen | Yes | 1.4 |
| Patient 6’s specimen | Yes | 1.6 |
| Patient 7’s specimen | Yes | 1.9 |
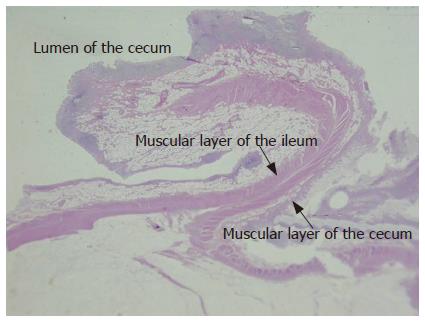
The microscopic examination supports our postulation that there is the intussusception of the terminal ileum into the cecum at the ileocecal junction. Figures 3 and 4 show both muscular layers of the terminal ileum and the cecum in the area of intussusception.
In 1859 John Hunter proposed his valvular concept of the ileocecal junction of which the mucosa fold extending into the cecum (Flap-valve)[1]. However, our findings from the observation during the operation of the ileocecal junction area and examination of specimens, revealed that there is an intussusception of the terminal ileum into the cecum in every specimen. Cross section of ileocecal junction display both muscular and mucosal layers of the terminal ileum fold into the cecum wall (Figuers 3 and 4). The intussusceptum can be reduced from the cecum by dissection between layers of the terminal ileum and cecum. These findings further refute the flap-valve concept previously believed. Moreover, additional microscopic study reveals that the terminal ileum and cecum are bundled together. Muscle fibers of the cecum and terminal ileum can be depicted separately though bundled up together in the ileocecal junction.
According to these findings, our impression that all layers of the terminal ileum is intussuscepted into the cecum wall is the important role in the anatomy of ileocecal junction which contrary to the previous belief of merely the mucosa.
We will later explore the relationship between the intussusception of the terminal ileum into the cecum and the competency for the ileocecal junction.
The authors are grateful to Dr. Paiboon Jivapaisarnpong, Colorectal Division, Department of Surgery, Rajavithi Hospital and Dr. Jirawat Pattana-arun, Colorectal Division, Department of Surgery, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University who kindly inspired us to challenge the flap-valve concept of the ileocecal junction.
S- Editor Wang J L- Editor Alpini GD E- Editor Zhou T
| 1. | Kumar D, Phillips SF. The contribution of external ligamentous attachments to function of the ileocecal junction. Dis Colon Rectum. 1987;30:410-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Rosenberg JC, DiDio LJ. Anatomic and clinical aspects of the junction of the ileum with the large intestine. Dis Colon Rectum. 1970;13:220-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Cohen S, Harris LD, Levitan R. Manometric characteristics of the human ileocecal junctional zone. Gastroenterology. 1968;54:72-75. [PubMed] |
| 4. | Shafik A, El-Sibai O, Shafik AA. Physiological assessment of the function of the ileocecal junction with evidence of ileocecal junction reflexes. Med Sci Monit. 2002;8:CR629-CR635. [PubMed] |
| 5. | Corazziari E, Barberani F, Tosoni M, Boschetto S, Torsoli A. Perendoscopic manometry of the distal ileum and ileocecal junction in humans. Gastroenterology. 1991;101:1314-1319. [PubMed] |
| 6. | Barberani F, Corazziari E, Tosoni M, Badiali D, Materia E, Ribotta G, Montesani C, Boschetto S, Torsoli A. Perendoscopic manometry of the distal ileum and ileocecal junction: technique, normal patterns, and comparison with transileostomy manometry. Gastrointest Endosc. 1994;40:685-691. [PubMed] |
| 7. | Nasmyth DG, Williams NS. Pressure characteristics of the human ileocecal region--a key to its function. Gastroenterology. 1985;89:345-351. [PubMed] |
| 8. | Nivatvongs S, Gordon PH. Surgical anatomy. Principles and practice of surgery for colon, rectum and anus. 2nd ed. St. Louis: Quality Medical Publishing 1999; 33-39. |