Published online May 14, 2007. doi: 10.3748/wjg.v13.i18.2600
Revised: February 15, 2007
Accepted: March 26, 2007
Published online: May 14, 2007
AIM: To investigate the hypothesis that duodenal bulb (DB) inhibition on pyloric antrum (PA) contraction is reflex.
METHODS: Balloon (condom)-tipped tube was introduced into 1st duodenum (DD) and a manometric tube into each of PA and DD. Duodenal and antral pressure response to duodenal and then PA balloon distension with saline was recorded. These tests were repeated after separate anesthetization of DD and PA.
RESULTS: Two and 4 mL of 1st DD balloon distension produced no pressure changes in DD or PA (10.7 ± 1.2 vs 9.8 ± 1.2, 11.2 ± 1.2 vs 11.3 ± 1.2 on H2O respectively, P > 0.05). Six mL distension effected 1st DD pressure rise (30.6 ± 3.4 cm H2O, P < 0.01) and PA pressure decrease (6.2 ± 1.4 cm H2O, P < 0.05); no response in 2nd, 3rd and 4th DD. There was no difference between 6, 8, and 10 mL distensions. Ten mL PA distension produced no PA or 1st DD pressure changes (P > 0.05). Twenty mL distension increased PA pressure (92.4 ± 10.7 cm H2O, P < 0.01) and decreased 1st DD pressure (1.6 ± 0.3 cm H2O, P < 0.01); 30, 40, and 50 mL distension produced the same effect as the 20 mL distension (P > 0.05). PA or DD distension after separate anesthetization produced no significant pressure changes in PA or DD.
CONCLUSION: Large volume DD distension produced DD pressure rise denoting DD contraction and PA pressure decline denoting PA relaxation. PA relaxation upon DD contraction is postulated to be mediated through a reflex which we call duodeno-antral reflex. Meanwhile, PA distension effected DD relaxation which we suggest to be reflex and termed antro-duodenal reflex. It is suggested that these 2 reflexes, could act as investigative tools in diagnosis of gastroduodenal motility disorders.
- Citation: Shafik A, El Sibai O, A Shafik A. Study of the duodenal contractile activity during antral contractions. World J Gastroenterol 2007; 13(18): 2600-2603
- URL: https://www.wjgnet.com/1007-9327/full/v13/i18/2600.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i18.2600
The stomach has two functions: secretion and motility. The main function of the proximal stomach is secretion, and so its motility pattern in the fed state takes the form of prolonged relaxation to delay intragastric food passage and provide ample time for contact with gastric enzymes[1-3]. The proximal stomach is often described as a receptive reservoir. Meanwhile the distal stomach functions to mechanically mix and crush the solid particles. Its motility pattern in the fed state presents a strong antral peristalsis that continues until complete evacuation of the chyme is achieved[1-3]. The antral peristalsis may be so strong as to raise the antral pressure to about 100 mm Hg[4].
The stomach and duodenum possess adaptive cytoprotection which represents an important defensive phenomenon[5]. However, this protection may be antagonized by drugs such as indomethacin. Nitric oxide increases HCO3-secretion in the duodenum. This action depends on cGMP- related COX-1 activation and is mediated by prostaglandins[6].
The antral mechanical contractions are believed to be under the control of a gastric pacemaker located at the junction of the upper with the lower two thirds of the greater curvature[7]. In the fed state, the duodenal bulb contracts but, unlike the antrum, not continuously throughout the fed state. Duodenal bulb contractions cease intermittently to allow gastric emptying[7-9]. The mechanism of duodenal bulb inhibition upon antral contraction is not exactly known; is it a direct or reflex action between the antrum and duodenal bulb? We hypothesized that the mechanism of duodenal bulb relaxation upon antral contraction for gastric emptying is reflex. This hypothesis was investigated in the current study.
Thirty-two healthy volunteers (mean age 38.2 ± 9.7 SD, range 27-48, 20 men, 12 women) were enrolled in the study after giving informed written consent. The subjects were selected to have no gastrointestinal complaint in the past or at the time of enrollment. Physical examination, includ-ing neurological assessment, was normal. The results of examination of blood count, renal and hepatic functions as well as electrocardiography were unremarkable. Endoscopies for esophagus, stomach, and duodenum showed normal findings. The study was approved by the Review Board and Ethics Committee of the Cairo University Faculty of Medicine.
The subjects fasted for 12 h. A condom was applied to the distal end of a Ryle stomach tube (8 French, Pharma Plast Int AS/DK 3540, Lynge, Denmark) containing multiple lateral apertures. One tie was applied at each end of the condom to fashion a high compliance balloon. A silver clip was applied to the distal end of the tube for radiologic control. A mechanical puller was used for automatic tube withdrawal (9021 H, Disa, Copenhagen). The tube with the empty condom was swallowed by the volunteers and the condom was directed to lie in the 1st part of the dudodenum (DD). The tube was connected to a strain gauge pressure transducer (Statham 230B, Oxnard, CA, USA).
Simultaneous measurement of the pressure in the PA and DD was performed by means of a perfused open-ended tube of 1 mm internal and 1.5 mm external diameter. One tube was introduced into each of the PA and 1st DD. Each tube was connected to a Statham pressure transducer. The position of these manometric tubes was accurately determined from the previously performed barium enemas and from the fluoroscopic screening. For the latter, a silver clip had been applied to the distal end of each tube. The pressure recordings were performed 20 min after tubal positioning so that the gut could have adapted to the presence of the tubes.
The resting (basal) pressure was recorded in the PA and in each of the 4 parts of the DD. The condom, while lying in the 1st DD, was filled in increments of 2 mL up to 10 mL and the pressure in the PA and the 1st DD was recorded at each of the volumes. The condom was then emptied and placed successively in the 2nd, 3rd, and 4th parts of the DD, and the aforementioned test was repeated. The emptied condom was then pulled under guidance of the screen to lie in the PA as was confirmed under the screen. It was filled with normal saline in increments of 10 mL up to 50 mL and the pressure in the PA and 1st DD was recorded at each of the volumes. The test was repeated while the manometric tube was managed to lie successively in the 2nd, 3rd, and 4th DD. For fear of antral or duodenal injury, we did not fill the condom with saline quantities beyond the mentioned volumes.
The effect of distension of the anesthetized DD on the PA pressure was examined. The DD was anesthetized by instilling 10 mL of 2 percent of lidocaine through the tube placed in the DD. The PA response to distension of the anesthetized DD was determined after 20 min and 2 h later when the anesthetic effect had waned. The test was repeated using normal saline instead of lidocaine. After 2 d,
the response of the DD pressure to distension of the anesthetized PA was recorded. The PA was anesthetized by means of 50 mL of 2 percent lidocaine instilled through the tube in the PA. The effect of distension of the anesthetized PA on the DD was registered after 20 min and again after 2 h of anesthetization. The test was repeated using normal saline instead of lidocaine.
To ensure reproducibility of the results, the aforemen-tioned recordings were repeated at least twice in the individual subject and the mean value was calculated. The results were analyzed statistically using the Student's t test and values were given as the mean ± SD. Differences assumed significance at P < 0.05.
The study was completed in all of the subjects with no adverse side effects. The mean resting pressure in the PA was 11.2 ± 1.2 cm H2O (range 10-13), and in the 1st DD 10.7 ± 1.2 cm H2O (range 9-12); the pressure of the 2nd, 3rd, and 4th DD was similar to that of the 1st DD (P > 0.05).
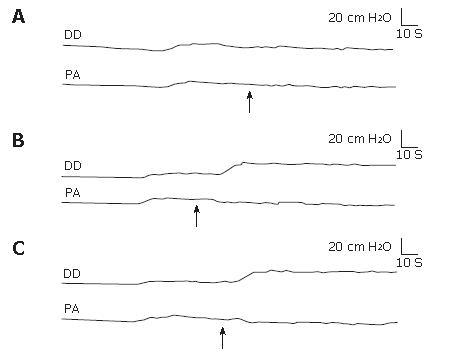
Response of the DD and PA pressures to duodenal balloon distension. Duodenal balloon distension with 2 and 4 mL of normal saline effected no significant pressure changes to the 4 duodenal parts or the PA (P > 0.05, Figure 1A). The duodenal pressure recorded a mean of 9.8 ± 1.2 cm H2O (range 8-12) with no significant differences in the 4 duodenal segments, and the PA a mean of 11.3 ± 1.2 cm H2O (range 10-13). Meanwhile 6 mL balloon distension of the 1st DD produced a significant duodenal pressure elevation and a PA pressure decrease (Figure 1B); no significant pressure changes occurred in the 2nd, 3rd, and 4th DD. The pressure in the 1st DD recorded a mean of 30.6 ± 3.4 cm H2O (range 26-34, P < 0.01) and the PA pressure 6.2 ± 1.4 cm H2O (range 4-8, P < 0.05), and the balloon was dispelled to the 2nd DD; the 2nd, 3rd, and 4th parts of the DD recorded a mean of 10.2 ± 1.2 cm H2O (range 9-12, P > 0.05). Balloon distension of the 1st DD with 8 and 10 mL of saline produced duodenal and PA pressure changes similar to the 6 mL balloon distension (P > 0.05, Figure 1C).
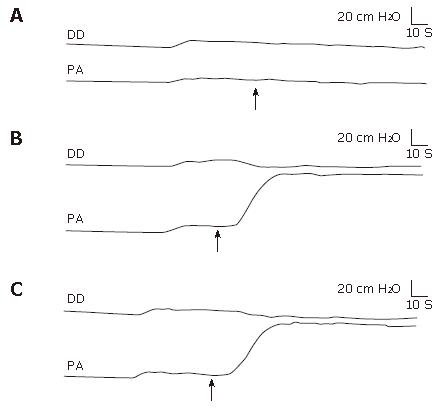
Response of the PA and DD pressures to pyloric antral balloon distension. Pyloric antral distension with 10 mL of saline did not effect significant pressure changes in the PA (P > 0.05) or the 1st, 2nd, 3rd, and 4th DD (P > 0.05, Figure 2A). The PA pressure recorded a mean of 10.9 ± 1.2 cm H2O (range 10-13). The duodenal pressure recorded a mean of 10.3 ± 1.2 cm H2O (range 8-12) in the four segments of the DD with no significant difference in the pressure response between them. Twenty mL balloon distension of the PA produced a significant increase of the PA pressure and a decrease of the 1st DD pressure, so that the balloon was dispelled to the 1st DD (Figure 2B); no significant pressure changes occurred in the remaining 3 DD segments. The 1st DD recorded a mean pressure of 1.6 ± 0.3 cm H2O (range 1-2.4, P < 0.01) and the other 3 parts of the DD a mean of 10.6 ± 1.2 (range 8-12, P > 0.05, Figure 2B). The PA pressure recorded a mean of 92.4 ± 10.7 cm H2O (range 81-108, P < 0.01). Pyloric antral balloon distension with 30, 40, and 50 mL of normal saline produced pressure changes in the DD and PA similar to those produced by the 20 mL distension (P > 0.05, Figure 2C).
Twenty minutes after the DD or PA had been separately anesthetized, saline balloon distension of either with up to 10 mL in the DD and 50 mL in the PA resulted in no significant pressure changes in the DD (P > 0.05). Two hours later when the anesthetic effect had waned, duodenal or antral balloon distension effected DD pressure responses similar to those prior to anesthetization (P > 0.05). Distension of the saline-containing DD or PA induced a DD pressure response similar to that recorded without the use of saline (P > 0.05).
The aforementioned results were reproducible with no significant difference (P > 0.05) when the tests were repeated in the individual subject.
The current study could shed some light on the response of the DD to the chyme bolus delivery from the PA. After the gastric content in the PA has been triturated to small particles, the PA contracts, the pyloric sphincter relaxes, and the chyme is passed to the DD[10-12]. The present investigation has shown that the PA did not respond to small chyme volumes; small volume balloon distension of the PA did not effect pressure changes in the PA or 1st DD. Meanwhile, large volumes of pyloric antral distension produced a significant PA pressure increase and a 1st DD pressure decrease, which presumably denotes PA contraction and DD relaxation; however, the rest of the DD exhibited no pressure changes. Thus, it appears that the 1st DD relaxes upon PA contraction, provided the PA distension is effected by a large bolus. The 1st DD seems to relax to accommodate the delivered bolus.
The study has also demonstrated that a large volume balloon distension of the DD produced increase of the duodenal pressure and decrease of the PA pressure. This presumably denotes that a large bolus entering the 1st DD causes DD contraction and PA relaxation. PA relaxation seems to prepare the PA for receiving new food boli for grinding, while 1st DD contraction delivers the chyme to the remaining DD segments hence become clear for receiving the following food bolus. Thus, it appears that during food digestion in the stomach, the chyme is transmitted to the DD through cycles of PA contraction and 1st DD relaxation followed by DD contraction and PA relaxation. These cycles of successive contraction and relaxation of the PA and DD and vice versa apparently continue until the stomach evacuates its contents.
The question that needs to be addressed is the PA relation to the 1st DD: is it a direct or reflex relationship?
Relaxation of the PA upon DD contraction postulates a reflex relationship between the 2 actions. This relationship was reproducible and its reflex nature is evidenced by its absence on individual anesthetization of the assumed two arms of the reflex arc, namely the PA or DD. We call this reflex relationship the 'duodeno-antral reflex' (DAR). This reflex apparently functions to relax the PA preparatory to receiving the next bolus of gastric contents for grinding; meanwhile contraction of the 1st DD pushes its contents to the remaining 3 DD segments, which eventually clears the 1st DD to receive new chyme boli. The current study further demonstrates that the 1st DD relaxes on PA contraction. This relationship was also reproducible, and its suggested reflex nature is evidenced by its absence on anesthetization of the 2 arms of the reflex arc: PA or DD. We call this reflex relationship the 'antro-duodenal reflex' (ADR). The 1st DD presumably relaxes to receive the chyme from the contracting PA.
Balloon distension of the PA or 1st DD apparently stimulates the antral or duodenal mechanoreceptors. Nerve impulses are transmitted to the spinal cord which sends impulses to the PA or DD. Anesthetization of the PA or DD seems to block their innervation so that nerve impulses cannot be transmitted to the spinal cord. Lidocaine blocks the sensory fibers (C and A α-fibers) which are responsible for pain and reflex activity[13-14]. Whether these reflex impulses are transmitted via extrinsic or intrinsic nerves needs further studies. However, investigators have recently reported on the effect of intraduodenal capsaicin on the interdigestive gastric contractions[15]. They found that duodenal afferent fibers stimulated by capsaicin inhibited the gastric contraction via a nitric oxide-independent extrinsic neural factor.
These 2 reflexes may prove to be of diagnostic significance in gastroduodenal motile disorders. Detectable changes in the DD reflex response to PA distension or of the PA to DD distension might denote a motility disorder of the PA or DD, or both. The reflex may thus be included as an investigative tool in the diagnosis of motility disorders in the gastroduodenum, provided further studies are performed in this respect.
In conclusion, the study has demonstrated the relaxation of the PA on duodenal contraction, and DD relaxation on PA contraction. This effect between the PA and the DD appears to be mediated through two reflexes which we call the 'duodeno-antral' and the 'antro-duodenal' reflexes. These reflexes seem to allow the chyme to pass to the 1st DD and from the latter to the rest of the DD. Further studies are required to investigate the functional and diagnostic significance of these 2 reflexes.
Margot Yehia assisted in preparing the manuscript.
S- Editor Liu Y L- Editor Alpini GD E- Editor Chen GJ
| 1. | Kelly KA. Gastric emptying of liquids and solids: roles of proximal and distal stomach. Am J Physiol. 1980;239:G71-G76. [PubMed] |
| 2. | Houghton LA, Read NW, Heddle R, Maddern GJ, Downton J, Toouli J, Dent J. Motor activity of the gastric antrum, pylorus, and duodenum under fasted conditions and after a liquid meal. Gastroenterology. 1988;94:1276-1284. [PubMed] |
| 3. | Brown BP, Schulze-Delrieu K, Schrier JE, Abu-Yousef MM. The configuration of the human gastroduodenal junction in the separate emptying of liquids and solids. Gastroenterology. 1993;105:433-440. [PubMed] |
| 4. | Quigley EM, Donovan JP, Lane MJ, Gallagher TF. Antroduodenal manometry. Usefulness and limitations as an outpatient study. Dig Dis Sci. 1992;37:20-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 63] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Mise S, Tonkic A, Pesutic V, Tonkic M, Mise S, Capkun V, Batelja L, Blagaic AB, Kokic N, Zoricic I. The presentation and organization of adaptive cytoprotection in the rat stomach, duodenum, and colon. Dedicated to André Robert the founder of the concept of cytoprotection and adaptive cytoprotection. Med Sci Monit. 2006;12:BR146-BR153. [PubMed] |
| 6. | Furukawa O, Kawauchi S, Mimaki H, Takeuchi K. Stimulation by nitric oxide of HCO3- secretion in bullfrog duodenum in vitro--roles of cyclooxygenase-1 and prostaglandins. Med Sci Monit. 2000;6:454-459. [PubMed] |
| 7. | Sanders KM, Vogalis F. Organization of electrical activity in the canine pyloric canal. J Physiol. 1989;416:49-66. [PubMed] |
| 8. | Brophy CM, Moore JG, Christian PE, Egger MJ, Taylor AT. Variability of gastric emptying measurements in man employing standardized radiolabeled meals. Dig Dis Sci. 1986;31:799-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 65] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Lin HC, Meyer JH. Disorders of gastric emptying. Textbook of Gastroenterology. Philadelphia: JB Lippincott Co 1991; 1213-1240. |
| 10. | Cooke AR. Control of gastric emptying and motility. Gastroenterology. 1975;68:804-816. [PubMed] |
| 11. | McCallum RW. Motor function of the stomach in health and disease. Gastrointestinal Disease: Pathophysiology, Diagnosis, Management. Philadelphia: Saunders 1989; 675-713. |
| 12. | Treacy PJ, Dent J, Jamieson GC. Antropyloric pressure and isolated pyloric waves are major regulators of gastric emptying of liquids. Gastroenterology. Philadelphia: Saunders 1988; 464-468. |
| 13. | Yokoyama O, Komatsu K, Kodama K, Yotsuyanagi S, Niikura S, Namiki M. Diagnostic value of intravesical lidocaine for overactive bladder. J Urol. 2000;164:340-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Silva C, Ribeiro MJ, Cruz F. The effect of intravesical resiniferatoxin in patients with idiopathic detrusor instability suggests that involuntary detrusor contractions are triggered by C-fiber input. J Urol. 2002;168:575-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 101] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Shibata C, Naito H, Ueno T, Jin XL, Funayama Y, Fukushima K, Matsuno S, Sasaki I. Intraduodenal capsaicin inhibits gastric migrating motor complex via an extrinsic neural reflex in conscious dogs. Neurogastroenterol Motil. 2002;14:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |