Published online May 7, 2007. doi: 10.3748/wjg.v13.i17.2510
Revised: January 31, 2007
Accepted: February 14, 2007
Published online: May 7, 2007
Colonic lipoma is a well-documented benign neoplasia, endoscopically appearing as a smooth round yellowish polyp with a thick stalk or broad-based attachment. We describe a 63-year old woman with persistent abdominal pain, in whom colonoscopy revealed a cecal mass with malignant features. Based on the colonoscopy findings, right hemicolectomy was laparoscopically performed for a presumptive diagnosis of a cecal adenocarcinoma, but histological examination revealed a colonic lipoma with overlying mucosal ulceration.
- Citation: Katsinelos P, Chatzimavroudis G, Zavos C, Pilpilidis I, Lazaraki G, Papaziogas B, Paroutoglou G, Kountouras J, Paikos D. Cecal lipoma with pseudomalignant features: A case report and review of the literature. World J Gastroenterol 2007; 13(17): 2510-2513
- URL: https://www.wjgnet.com/1007-9327/full/v13/i17/2510.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i17.2510
Lipomas are rare and slow-growing benign nonepithelial tumors that can be found in the gastrointestinal tract[1,2]. Lipomas develop only infrequently in the colon, and are usually asymptomatic and detected incidentally at colonoscopy, surgery or autopsy[3]. The occurrence of symptoms appears to be related to the size of lipoma. Those larger than 2 cm may occasionally cause abdominal pain, changes of bowel habits, rectal bleeding and bowel obstruction, intussusception or prolapse[3-5]. The common endoscopic picture consists of a smooth, spherical polyp, usually sessile and rarely penduculated that is slightly yellow, while the overlying mucosa is intact[1-6]. In rare cases the mucosa presents necrotic and/or ulcerative lesions that resemble malignant tumors[7,8]. The decision for selecting the most suitable treatment of a colonic lipoma mainly depends on the tumor's size and is either endoscopic resection or surgical removal. Lipomas with a diameter less than 2 cm can be safely removed endoscopically, whereas larger lesions should be removed by segment resection[9-11].
We describe a patient with persistent abdominal pain who underwent laparoscopic right hemicolectomy for the presumptive endoscopic diagnosis of cecal adenocarcinoma that turned out to be a lipoma on histological examination.
A 63-year old woman with abdominal pain for several weeks was referred to our department by a private gas-troenterologist for further investigation of a 2 cm broad-based cecal polypoid mass, revealed during colono-scopy.
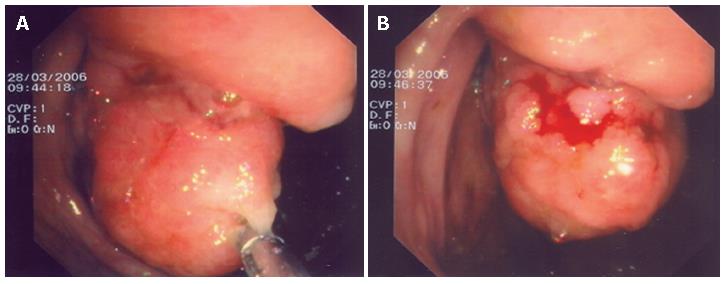
The patient did not report any episodes of constipation, diarrhea, hematochezia or melena, and her medical history did not include consumption of alcohol or non-steroid anti-inflammatory drugs (NSAIDs). Examination of the abdomen revealed no mass or tenderness. Detailed laboratory studies were within normal ranges, including complete peripheral blood cell count, blood coagulation and carcinoembryonic antigen (CEA). Colonoscopy performed in our department revealed a sessile tumor of about 2 cm in diameter, proximal to the ileocecal valve. The overlying mucosa was ulcerated and nodular with red color, while on palpation with biopsy forceps, the mass was felt to be stiff, not compressible and easy bleeding (Figure 1A and B). Although histopathological examination of biopsy specimens showed only non-specific ulcerations, malignancy could not be excluded according to the endoscopic findings. Further investigation included an abdominal ultrasound, which was negative for liver metastases and a computed tomography (CT) scan which showed a sessile neoplasm protruding into the lumen of cecum with a medium tissue density.
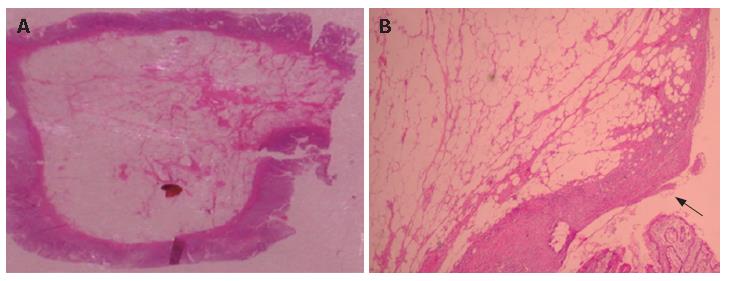
Given the suspicion of the malignant nature of the tumor, the patient underwent a laparoscopic right hemicolectomy. Macroscopic assessment of the resected specimen revealed a round polypioid tumor of 2.1 cm × 2.4 cm × 1.8 cm in size, with firm characteristics and nodular surface. Pathological examination of the resected lesion revealed a cecal lipoma with ulcerative lesions on the overlying mucosa (Figure 2A and B). The postoperative course was uneventful, and the patient was free of symptoms during a 10-month follow-up period.
Colonic lipomas are relatively uncommon tumors of mesenchymal origin, composed of well-differentiated adipose tissue supported by fibrous tissue, that rarely cause symptoms and are usually detected incidentally[1-3]. They arise from the submucosa, but occasionally extend into the muscularis propria; up to 10% are subserosal[12]. The incidence of lipomas relative to all polypioid lesions of the large intestine is reported to range from 0.035% to 4.4%[1,2]. However, they represent the third most common benign tumors after hyperplastic and adenomatous polyps[13]. They are usually solitary, but multiple lesions are reported in 10% to 25% of cases[1,3]. A rare polyposis syndrome has been described, with numerous lipomas throughout the bowel (colonic lipomatosis)[14]. Colonic lipomas are mainly found on the right-side of the colon and cecum[15]. Most of these tumors are asymptomatic and usually detected incidentally during colonoscopy and laparotomy. Only 25% of patients with colonic lipoma develop symptoms. When lipomas are larger than 2 cm in diameter, they may cause symptoms including bleeding with anemia, diarrhea or constipation, abdominal intestinal obstruction, and rarely, intussusception[16].
Various imaging modalities can imply the diagnosis of colonic lipomas. Barium enema may reveal an ovoid filling defect with well-defined borders. A so-called squeeze sign, indicating a change in size and shape of a radiolucent lesion in response to peristalsis, is frequently noted[17]. CT scans of colonic lipomas can provide a definite diagnosis because the mass typically has characteristic fatty densitometric values[18,19]. On CT, lipomas appear ovoid or pear shaped, with sharp margins and absorption densities of -40 to -120 Hounsfield units, typical of fatty composition[20,21]. However, these features are evident only in large lesions, as smaller tumors are not detectable due to artifacts and partial volume averaging[22]. Correspondingly, in our case, abdominal CT was not diagnostic for lipoma possibly due to the tumor's relatively small size. Magnetic resonance imaging (MRI) may be particularly useful in the detection of lipomas as the signal intensity is characteristic of adipose tissue on T1-weighted and fat-suppressing images[23,24]. Endoscopic ultasonography (EUS) is a potent adjunct modality for characterization of submucosal tumors. Colonic lipomas appear as hyperechoic lesions with regular borders in the three layers and can be distinguished from smooth muscle tumors, lymphangiomata, and invasive or metastatic malignancies[25]. EUS can be used to determine any extension into the muscularis propria before injection-assisted polypectomy of symptomatic lipomas[26]. Recently, CT colonographic examination (virtual colonoscopy) has been performed to detect colonic lipomas[27].
Endoscopy can usually distinguish lipomas from gas-trointestinal cancer or other tumors. Lipomas are seen as smooth, rounded yellowish polyps with a thick stalk or broad-based attachment[1-6]. Typical colonoscopic features are the "cushion sign" or "pillow sign" (pressing forceps against the lesion results in depression or pillowing of the mass) and the naked fat sign (extrusion of yellowish fat at biopsy site)[4,12,28,29]. Although the mucosa overlying a colonic lipoma is usually not involved, in rare cases, as in our patient, colonoscopy may reveal ulcerations and stiffness on palpation that may lead to a mistaken impression of carcinoma. Eleven such cases[7,8,30-36] reported over 3 decades are summarized in Table 1. Among these patients the most common indications for endoscopy were hematochezia and persistent abdominal pain. The location of lesion was in the cecum in three cases, ascending and transverse colon in one respectively, descending colon in two and rectosigmoid in four cases. In cases where biopsy specimens were taken, only hemorrhagic necrosis or ulceration of the mucosa was identified. In all but one case treatment consisted of operative resection.
| Author | Year | Age | Sex | Clinical presentation | Site of lipoma | Size (cm) | Treatment | Histological findings of endoscopic biopsies |
| Loludice[7] | 1980 | 43 | M | Hematochezia | Descending | 3.9 | Left hemicolectomy | Ulcerated mucosal |
| Lera[30] | 1982 | 70 | F | Abdominal pain | Hepatic flexure | 4 | Right hemicolectomy | - |
| Snover[8] | 1984 | 57 | M | Occult blood | Sigmoid | 3 | Sigmoid colectomy | Ulcerated mucosa |
| McGrew[31] | 1985 | 75 | M | Hematochezia | Rectosigmoid | 5 | Endoscopic resection | - |
| Taylor[32] | 1987 | 62 | M | Hematochezia | Sigmoid | 10 | Sigmoid colectomy | Ulcerated mucosa |
| Ibrazullah[33] | 1992 | 50 | M | Hematochezia | Descending | 3 | Left hemicolectomy | Inflammatory tissue |
| El-Khalil[34] | 2000 | 64 | M | Hematochezia | Sigmoid | 7.8 | Left hemicolectomy | Focal hemorrhagic necrosis |
| Caterino[35] | 2002 | 60 | M | Abdominal pain | Hepatic flexure | 5 | Right hemicolectomy | - |
| Meghoo[36] | 2003 | 60 | F | Hematochezia | Cecum | 6 | Right hemicolectomy | Ulcerated mucosa |
| Huh[16] | 2006 | 62 | M | Intussusception | Sigmoid | 3.5 | Anterior resection | Focal hemorrhagic necrosis and inflammation |
| Katsinelos | 2006 | 62 | F | Abdominal pain | Cecum | 2.4 | Laparoscopic right hemicolectomy | Non-specific ulceration |
The indications for performing colonoscopic snare polypectomy to remove colonic lipomas remain con-troversial[9,28,37]. Most authors agree that colonic lipomas with a diameter larger than 2 cm should be removed surgically, because in these cases endoscopic resection is associated with a high rate of complications[9,10,38,39]. However, especially for large penduculated lipomas, the size of the stalk seems to be a more important factor than the diameter of the lipoma when colonoscopic removal is considered[10,38]. In our opinion, if a lipoma is sessile or broadly-based, endoscopic removal is risky because the fatty tissue is an inefficient conductor for electric current and may result in a significantly high rate of complications like perforation or hemorrhage.
A wide range of operative techniques using conventional laparotomy[9] and mini-laparotomy[40] have been described including enucleation, colostomy, excision and segmental colonic resection. However, only a few cases of laparosco-pic resection of colonic lipomas have been reported so far[13,15,39,41-47]. Advantages of laparoscopic surgery include less postoperative pain, shorter hospitalization and faster recovery than conventional laparotomy. The latest publish-ed data referring to the comparison of laparoscopic versus open colorectal resection for cancer[48-49] indicate that laparoscopic resection of colonic lipomas should become the gold standard method for removal of lipomas greater than 2-3 cm in diameter, even in cases where the malignancy of the tumor could not be excluded preoperatively.
In conclusion, our case emphasizes that a colonic lipoma can simulate a malignant neoplasm and underscores the laparoscopic resection as the recommended operation for symptomatic colonic lipomas.
S- Editor Liu Y L- Editor Wang XL E- Editor Zhou T
| 1. | Corman ML. Colon and rectal surgery. 4th ed. Philadelphia: Lippincott-Raven 1998; 913-915. |
| 2. | Castro EB, Stearns MW. Lipoma of the large intestine: a review of 45 cases. Dis Colon Rectum. 1972;15:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Vecchio R, Ferrara M, Mosca F, Ignoto A, Latteri F. Lipomas of the large bowel. Eur J Surg. 1996;162:915-919. [PubMed] |
| 4. | Pfeil SA, Weaver MG, Abdul-Karim FW, Yang P. Colonic lipomas: outcome of endoscopic removal. Gastrointest Endosc. 1990;36:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Rogy MA, Mirza D, Berlakovich G, Winkelbauer F, Rauhs R. Submucous large-bowel lipomas--presentation and management. An 18-year study. Eur J Surg. 1991;157:51-55. [PubMed] |
| 6. | Bahadursingh AM, Robbins PL, Longo WE. Giant submucosal sigmoid colon lipoma. Am J Surg. 2003;186:81-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | LoIudice TA, Lang JA. Submucous lipoma simulating carcinoma of the colon. South Med J. 1980;73:521-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Snover DC. Atypical lipomas of the colon. Report of two cases with pseudomalignant features. Dis Colon Rectum. 1984;27:485-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Chung YF, Ho YH, Nyam DC, Leong AF, Seow-Choen F. Management of colonic lipomas. Aust N Z J Surg. 1998;68:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Stone C, Weber HC. Endoscopic removal of colonic lipomas. Am J Gastroenterol. 2001;96:1295-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | de Ruijter SH, van Marle AG, Doornewaard H, Melse JC. Submucosal lipoma of the colon: abdominal cramps with rectal bleeding and weight loss. Ned Tijdschr Geneeskd. 2006;150:1990-1993. [PubMed] |
| 12. | De Beer RA, Shinya H. Colonic lipomas. An endoscopic analysis. Gastrointest Endosc. 1975;22:90-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Chiba T, Suzuki S, Sato M, Tsukahara M, Saito S, Inomata M, Orii S, Suzuki K. A case of a lipoma in the colon complicated by intussusception. Eur J Gastroenterol Hepatol. 2002;14:701-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Tatsuguchi A, Fukuda Y, Moriyama T, Yamanaka N. Lipomatosis of the small intestine and colon associated with intussusception in the ileocecal region. Gastrointest Endosc. 1999;49:118-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Cossavella D, Clerico G, Rosato L, Galetto PV, Paino O, Trompetto M, Luc AR, Pozzo M. Lipoma of the colon as an unusual cause of recurring partial intestinal occlusion. Clinical case and review of the literature. Minerva Chir. 1998;53:277-280. [PubMed] |
| 16. | Huh KC, Lee TH, Kim SM, Im EH, Choi YW, Kim BK, Jung DJ, Choi WJ, Kang YW. Intussuscepted sigmoid colonic lipoma mimicking carcinoma. Dig Dis Sci. 2006;51:791-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Buetow PC, Buck JL, Carr NJ, Pantongrag-Brown L, Ros PR, Cruess DF. Intussuscepted colonic lipomas: loss of fat attenuation on CT with pathologic correlation in 10 cases. Abdom Imaging. 1996;21:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Kakitsubata Y, Kakitsubata S, Nagatomo H, Mitsuo H, Yamada H, Watanabe K. CT manifestations of lipomas of the small intestine and colon. Clin Imaging. 1993;17:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Wulff C, Jespersen N. Colo-colonic intussusception caused by lipoma. Case reports. Acta Radiol. 1995;36:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Heiken JP, Forde KA, Gold RP. Computed tomography as a definitive method for diagnosing gastrointestinal lipomas. Radiology. 1982;142:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 64] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Megibow AJ, Redmond PE, Bosniak MA, Horowitz L. Diagnosis of gastrointestinal lipomas by CT. AJR Am J Roentgenol. 1979;133:743-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Younathan CM, Ros PR, Burton SS. MR imaging of colonic lipoma. J Comput Assist Tomogr. 1991;15:492-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Liessi G, Pavanello M, Cesari S, Dell'Antonio C, Avventi P. Large lipomas of the colon: CT and MR findings in three symptomatic cases. Abdom Imaging. 1996;21:150-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Kameyama H, Niwa Y, Arisawa T, Goto H, Hayakawa T. Endoscopic ultrasonography in the diagnosis of submucosal lesions of the large intestine. Gastrointest Endosc. 1997;46:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Ochiai T, Akahoshi K, Hamada S, Chijiiwa Y, Nawata H, Namoto M. Endoscopic resection of a colonic lipoma under endoscopic ultrasound guidance. Endoscopy. 1998;30:S65-S66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Johnson CD, Hara AK, Reed JE. Computed tomographic colonography (Virtual colonoscopy): a new method for detecting colorectal neoplasms. Endoscopy. 1997;29:454-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Christie JP. The removal of lipomas. Gastrointest Endosc. 1990;36:532-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Zhang H, Cong JC, Chen CS, Qiao L, Liu EQ. Submucous colon lipoma: a case report and review of the literature. World J Gastroenterol. 2005;11:3167-3169. [PubMed] |
| 30. | Lera JM, Gómez-Portilla A, Fakih A, Vicente F, Zornoza G. Submucosal lipomas of the colon. Rev Med Univ Navarra. 1982;26:185-187. [PubMed] |
| 31. | McGrew W, Dunn GD. Colonic lipomas: clinical significance and management. South Med J. 1985;78:877-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Taylor BA, Wolff BG. Colonic lipomas. Report of two unusual cases and review of the Mayo Clinic experience, 1976-1985. Dis Colon Rectum. 1987;30:888-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Ibrarullah M, Aggarwal R, Choudhuri G, Tandon P, Kapoor VK. Colonic lipoma, masquerading as malignant tumour. Indian J Cancer. 1992;29:4-6. [PubMed] |
| 34. | El-Khalil T, Mourad FH, Uthman S. Sigmoid lipoma mimicking carcinoma: case report with review of diagnosis and management. Gastrointest Endosc. 2000;51:495-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Caterino S, Tiziano G, Mercantini P, Ziparo V. Rectorrhagia caused by lipoma of the hepatic flexure of the colon. A case report and review of the literature. G Chir. 2002;23:205-208. [PubMed] |
| 36. | Meghoo CA, Cook PR, McDonough CA, Bowser LK, Waddell BE. Large colonic lipoma with mucosal ulceration mimicking carcinoma. Gastrointest Endosc. 2003;58:468-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Yu JP, Luo HS, Wang XZ. Endoscopic treatment of submucosal lesions of the gastrointestinal tract. Endoscopy. 1992;24:190-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Tamura S, Yokoyama Y, Morita T, Tadokoro T, Higashidani Y, Onishi S. "Giant" colon lipoma: what kind of findings are necessary for the indication of endoscopic resection? Am J Gastroenterol. 2001;96:1944-1946. [PubMed] |
| 39. | Abou-Nukta F, Gutweiler J, Khaw J, Yavorek G. Giant lipoma causing a colo-colonic intussusception. Am Surg. 2006;72:83-84. [PubMed] |
| 40. | Nakagoe T, Sawai T, Tsuji T, Tanaka K, Nanashima A, Shibasaki S, Yamaguchi H, Yasutake T. Minilaparotomy approach for removal of a large colonic lipoma: report of two cases. Surg Today. 2004;34:72-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Peters MB, Obermeyer RJ, Ojeda HF, Knauer EM, Millie MP, Ertan A, Cooper S, Sweeney JF. Laparoscopic management of colonic lipomas: a case report and review of the literature. JSLS. 2005;9:342-344. [PubMed] |
| 42. | Hackam DJ, Saibil F, Wilson S, Litwin D. Laparoscopic management of intussusception caused by colonic lipomata: a case report and review of the literature. Surg Laparosc Endosc. 1996;6:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Ladurner R, Mussack T, Hohenbleicher F, Folwaczny C, Siebeck M, Hallfeld K. Laparoscopic-assisted resection of giant sigmoid lipoma under colonoscopic guidance. Surg Endosc. 2003;17:160. [PubMed] |
| 44. | Saclarides TJ, Ko ST, Airan M, Dillon C, Franklin J. Laparoscopic removal of a large colonic lipoma. Report of a case. Dis Colon Rectum. 1991;34:1027-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 45. | Jelenc F, Brencic E. Laparoscopically assisted resection of an ascending colon lipoma causing intermittent intussusception. J Laparoendosc Adv Surg Tech A. 2005;15:173-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 46. | Chiu CC, Wei PL, Huang MT, Wang W, Chen TC, Lee WJ. Colonoscopic-assisted laparoscopic resection of a colon lipoma. J Laparoendosc Adv Surg Tech A. 2006;16:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 47. | Scoggin SD, Frazee RC. Laparoscopically assisted resection of a colonic lipoma. J Laparoendosc Surg. 1992;2:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 48. | Zerey M, Burns JM, Kercher KW, Kuwada TS, Heniford BT. Minimally invasive management of colon cancer. Surg Innov. 2006;13:5-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 49. | Lezoche E, Guerrieri M, De Sanctis A, Campagnacci R, Baldarelli M, Lezoche G, Paganini AM. Long-term results of laparoscopic versus open colorectal resections for cancer in 235 patients with a minimum follow-up of 5 years. Surg Endosc. 2006;20:546-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |