INTRODUCTION
Small bowel obstruction is a common surgical emergency and a frequently encountered problem in abdominal surgery[1,2]. It is a major cause of morbidity and medical cost in hospitals around the world[3] and a significant cause of admissions for emergency surgical treatment[2]. It is a highly severe conditions, requiring quick and correct diagnosis as well as immmediate, rational and effective therapy[4]. Although small bowel obstruction is common, persistent omphalomesenteric duct as a cause of this condition, particularly in adult patients, is an exceptional finding.
The omphalomesenteric duct remnant is one of the rare congenital anomalies associated with the primitive yolk stalk[5,6]. Most omphalomesenteric duct remnants tend to be Meckel’s diverticulum while the occurrence of a persistent omphalomesenteric duct is infrequent[5,6]. An omphalomesenteric duct remnant may induce intestinal obstruction, abdominal pain, melena, and umbilical hernia or drainage that tend to occur most frequently during childhood[5,6]. An extremely rare case of persistent omphalomesenteric duct causing small bowel obstruction in an adult patient is herein presented.
CASE REPORT
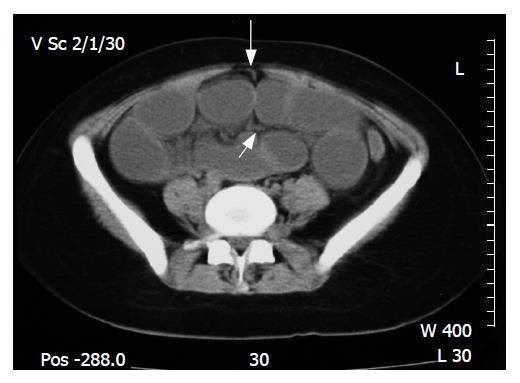
A 20-year-old female patient without any medical history or history of previous abdominal operation presented in our department with colicky abdominal pain, vomiting, absence of passage of gas and feces, and abdominal distension of 24 h duration. Physical examination and blood tests were normal. Abdominal X-ray revealed small bowel obstruction with marked small bowel air-fluid levels (Figure 1). Ultrasound of the abdomen showed dilated small bowel loops. Abdominal computed tomography (CT) demonstrated dilated small bowel and a band originating from the umbilicus and continuing between the small bowel loops; an omphalomesenteric duct remnant was suspected (Figure 2).
Figure 1 Abdominal X-ray revealing marked small bowel air-fluid levels.
Figure 2 CT scan demonstrating dilated small bowel and a band originating from the umbilicus (big white arrow) and continuing between the small bowel loops (small white arrow).
The patient was managed with restriction of oral intake, nasogastric suction, and intravenous hydration. Since no resolution of the obstruction or improvement of the clinical picture of the patient was observed in the following 12 h, and due to the suspicion of a persistent omphalomesenteric duct in the CT scan, an operative intervention was decided. In exploratory laparotomy, a fibrous cord extending from the anti-mesenteric border of the preterminal ileum to the posterior wall of the umbilicus was identified, justifying the suspicion of persistent omphalomesenteric duct, causing closed loop ileal obstruction. The persistent omphalomesenteric duct was resected and the obstruction was resolved without bowel resection. The patient had an uneventful recovery and was discharged on the 5th postoperative day.
DISCUSSION
Acute mechanical small bowel obstruction is a common surgical emergency[1,2]. Immediate and correct diagnosis of this condition and its etiology are essential and appropriate treatment is of utmost importance[4]. The clinical picture, however, of these patients[4,7] along with the etiology of obstruction[1,3] may be variable while appropriate management remains controversial[1-3,8,9].
The most frequent symptoms and signs of patients with small bowel obstruction, although variable, are abdominal pain, vomiting, constipation, abdominal distension and tenderness[4,7]. Adhesions, incarcerated hernias, and large bowel cancer constitute the most frequent causes of obstruction while adhesions are the leading cause accounting for 45%-80%[1,3,8,10]. Other less common causes reported in the literature are Crohn’s disease, gallstones, bowel volvulus, and intussusception accounting for 2%-14% of small bowel obstruction cases[3,8,10]. Small bowel obstruction, however, due to persistent omphalomesenteric duct, particularly in adult patients, is extremely rare with very few cases reported in the literature[11-17].
Omphalomesenteric duct remnants (vitelline duct anomalies) have been reported to be congenital anomalies associated with the primitive yolk stalk[5,6]. The omphalomesenteric duct is the embryonic structure connecting the primary yolk sac to the embryonic midgut that normally becomes a thin fibrous band, which eventually disintegrates and is absorbed spontaneously at the 5th-10th wk of gestation[5,6]. The omphalomesenteric duct will continue to grow if it fails to completely atrophy and disintegrate; the failure of such closure may result in various lesions (omphalomesenteric duct remnants): Meckel’s diverticulum, patent omphalomesenteric duct (umbilicoileal fistula), omphalomesenteric duct (umbilical) sinus, omphalomesenteric duct (umbilical) cyst, umbilical mucosal polyp or a fibrous cord connecting the ileum to the umbilicus[5,6,18]. Meckel diverticulum is the most common omphalomesenteric duct anomaly[5,6].
Omphalomesenteric duct remnants may persist in approximately 2% of infants[18]. Although these malformations are found with equal frequency between the sexes, a significantly greater incidence of symptoms is encountered in males[6]. Even though they may be asymptomatic, common symptoms of omphalomesenteric duct malformations include abdominal pain, rectal bleeding, intestinal obstruction, umbilical drainage, and umbilical hernia[5,6], and all these symptoms appear to be age-dependent. Most of the symptoms usually appear before the age of 4 years[5]. Eighty-five percent of infants younger than 1 mo and 77% of children aged 1 mo to 2 years have a symptomatic presentation[5]. It has also been reported that 40% of the children with this anomaly have symptomatic lesions, while this anomaly is usually asymptomatic in adults[5].
There are many mechanisms for small bowel obstruction from a persistent omphalomesenteric duct. These mechanisms include intussusception, in case of a patent omphalomesenteric duct, volvulus or internal hernia (closed loop obstruction) from a patent omphalomesenteric duct or a fibrous connection between the umbilicus and the ileum[11-17]. A fibrous cord connecting the umbilicus to the ileum, such as in the presented case, results from an atrophic omphalomesenteric duct that is not completely obliterated and absorbed. Congenital fibrous bands are clinically significant because they may lead to intestinal obstruction, as in our patient[11-14,17].
In general, appropriate treatment of small bowel obstruction as well as timing of surgery still remain controversial[1-3,8,9]. Management of this condition requires careful assessment and awareness while the appropriate treatment needs to be tailored to the individual situation[9]. An important share of these patients, particularly those with adhesive small bowel obstruction, can be safely and effectively treated nonoperatively[2,3,7-10]. Great caution should be paid, however, since the incidence of bowel strangulation is quite high[7,8,10]. In the reported case, since there was no history of previous abdominal operation and no resolution of the obstruction or improvement of the clinical picture of the patient was observed, and due to the suspicion of a persistent omphalomesenteric duct in the CT, an operative intervention was decided. Operative findings justified such treatment of our patient.
In conclusion, persistent omphalomesenteric duct constitutes an extremely infrequent cause of small bowel obstruction in adult patients, with very few cases reported in the literature. It should be taken into consideration, however, in adults with acute mechanical small bowel obstruction without any previous history of surgery.