INTRODUCTION
The prevalence of small intestinal diverticula on autopsy ranges from 0.06% to 1.3%[1]. The prevalence increases with age, peaking at the sixth and seventh decades[2]. Eighty percent of diverticula occur in the jejunum, 15% in the ileum and 5% in both[3]. Coexistent colonic and duodenal diverticula have been reported suggesting an associated or common etiology[4]. Most small bowel diverticula are thought to be acquired pulsion lesions. The clinical presentations of acquired jejunoileal diverticulosis are vague and diverse. As a result, identification of the disorder can be quite difficult. Presenting complaints such as intermittent abdominal pain, constipation and diarrhea, akin to those seen in irritable bowel syndrome, have been demonstrated in up to 90% of the patients[4] and imaging tests have mostly atypical appearance without key diagnostic features and may not correlate with the clinical symptoms. As a result, the diagnosis is frequently made incidentally either by radiographic examination or upon laparotomy due to complications. Thus, clinical recognition of the disease depends primarily on an awareness of the condition and the various ways in which it may present.
The reported complications of jejunoileal diverticulosis include chronic abdominal pain, malabsorption, hemorrhage, diverticulitis, obstruction, abscesses in the mesentery and perforation, and occur in 10%-30% of patients[5-7]. Jejunoileal diverticulitis is quite uncommon and has a mortality rate as high as 24%[8,9]. We report a case of complicated jejunal diverticulits in conjunction with sigmoid diverticulits and review its presentation, clinical features, and management.
CASE REPORT
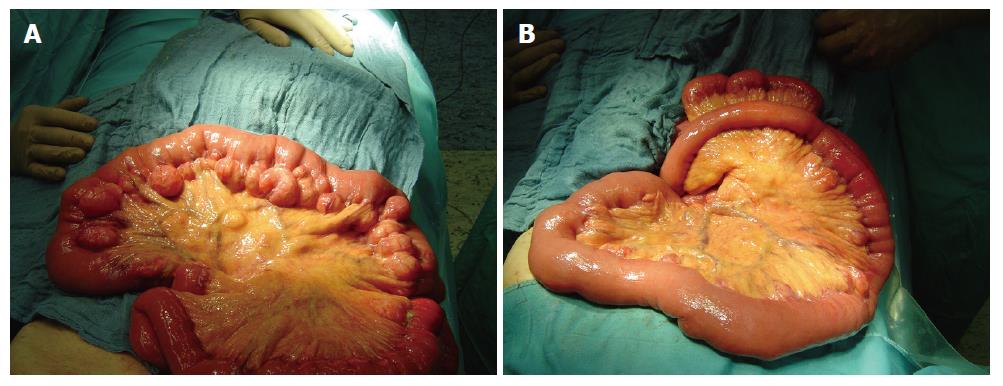
An 85-year old man with a history of ischemic heart disease, chronic obstructive pulmonary disease (COPD), atrial fibrillation and myocardial infarction was admitted to our hospital because of abdominal pain. He was taking regular medications for the above mentioned conditions including warfarin for prevention of systemic embolism owing to atrial fibrillation. He had previously episodes of pneumonia with fever, and chills that were managed conservatively. He had been otherwise well since then. The patient underwent no surgical procedure in the past. The abdominal pain was diffuse and severe. He denied shortness of breath and changes in eating or bowel habits. Physical examination revealed tenderness and distention of the abdomen and no palpable mass. On admission, elevated white blood cell count (12 900/mm3; normal 4000-9000/mm3) and C-reactive protein (32.48 mg/L; normal < 5.0 mg/L) were found. All other laboratory data were within normal limits. Computed tomography of the abdomen revealed no abnormalities except for prostate hypertrophy. Pneumoperitoneum was not visible. Because of this unclear condition, the patient was subjected to laparoscopic evaluation of the abdomen. A jejunal diverticulosis complicated by diverticulitis and abscesses in the mesentery (Figure 1A and B) and coexisting sigmoid diverticulitis was found. Laparoscopy was converted to laparotomy which confirmed multiple diverticula in a 100-cm segment of jejunum, commencing 20 cm distal to the ligament of Treitz with massive inflammation and abscesses at locations of 2 diverticula. One of the diverticula was supposed to be perforated. However, a free perforation within the peritoneal cavity was not seen. The remainder of the small bowel appeared normal. Coexisting diverticulosis of the left colon with sigmoid diverticulitis was also found. Since both diverticular conditions could be the cause of the presenting symptom of the patient (peritonitis), resection of the entire diverticula-bearing segment of jejunum with primary anastomosis and sigmoid colectomy with temporary end colostomy (Hartmann’s procedure) were carried out. Final pathology confirmed evidence of a perforated diverticulitis and purulent peridiverticulitis with peritonitis. Furthermore, inflammation, scaring and stenosis of large intestinal lining indicating a chronic process were found. The postoperative course was complicated due to wound infection and pneumonia. However, he recovered after appropriate medical management and was discharged home.
Figure 1 Laparotomy showing multiple diverticula in a segment of jejunum with massive inflammation and small abscesses in the mesentery of a 85-yr old man with jejunal diverticulosis.
DISCUSSION
Acquired jejunoileal diverticulosis was first described in 1794 by Sommering and later in 1807 by Sir Astley Cooper and is characterized by herniation of mucosa and submucosa through the muscular layer of the bowel wall (false diverticula) on the mesenteric border of the bowel[10]. For several reasons, despite its 213-year history as a defined anatomic entity, the true prevalence of this disorder is difficult to ascertain. It is likely that many surgeons have not documented the presence of these lesions simply because little clinical significance has been attributed to them. Furthermore, as diverticula are frequently buried in the mesenteric fat, success in demonstrating them is related to the effort expended in searching for them. Diverticula are usually multiple, in contrast to the true congenital Meckel’s diverticulum and tend to be larger and higher in number in the proximal jejunum and smaller and fewer caudally[9]. Coexistent diverticula are found in the colon in 20%-70%, in the duodenum in 10%-40%, in the esophagus and stomach in 2% of patients and may partly indicate associated common etiology[11,12].
Regarding the etiology of jejunoileal diverticula, the current hypothesis focuses on abnormalities in the smooth muscle or myenteric plexus. Careful microscopic evaluation of jejunal specimens with diverticula has shown that these abnormalities are of three types[13]: fibrosis and decreased numbers of normal muscle cells, consistent with progressive systemic sclerosis; fibrosis and degenerated smooth muscle cells, suggestive of a visceral myopathy; neuronal and axonal degeneration indicative of visceral neuropathy. Any of these abnormalities could lead to distorted smooth muscle contractions of the affected small bowel generating increased intraluminal pressure. The result is herniation of mucosa and submucosa through the weakest mesenteric site of the bowel wall with penetration induced by paired blood vessels from the mesentery.
Usually, the disorder is clinically silent until it presents with complications. If symptomatic, vague and chronic abdominal pain of varying severity, localized epigastrically or periumbilically with a bloating sensation after food intake is frequent and may be the earliest symptom. Unfortunately, the only means of confirming a diverticular source is cessation of the pain after surgical resection of the involved segment of small bowel. Complications requiring surgical intervention occur in 8%-30% of patients[11]. Common acute complications of jejunoileal diverticulosis include diverticulitis, bleeding, perforation and intestinal obstruction.
Jejunoileal diverticulitis with or without perforation and abscess occurs in about 2%-6% of cases[6]. Patients usually present with a localized or diffuse peritonitis like in our case. However, presenting symptoms vary widely and are nonspecific. Therefore, the clinical picture can be confused with other intra-abdominal acute conditions such as appendicitis, cholecystitis, colonic diverticulitis, perforated ulcer and others. In general, there are no reliable diagnostic tests that can confirm the presence of complicated jejunoileal diverticulosis highlighting the diagnostic challenges of this disorder. Computed tomography (CT) may visualize localized inflammatory masses such as a large abscess confined to one quadrant[14]. However, owing to lack of key diagnostic features it may fail to identify diffuse inflammatory changes like in the presented case and, under normal circumstances, does not have additional benefits. Endoscopy (capsule endoscopy and double-balloon enteroscopy) is of benefit in diagnosing small-bowel disorders[15]. However, its utility in emergency situations like in the presented case is limited[16]. Mechanical obstruction as a result of pressure on the intestinal wall from inflammatory mass, or scarring and stenosis of the intestinal lining associated with diverticulitis, intussusception, and adhesions that influence insertion depth, are some of the limiting factors. As a result, the diagnosis is exclusion of one of the factors and seldom made before diagnostic laparoscopy or exploratory laparotomy[17]. Diagnostic laparoscopy is very useful in evaluating patients with a complicated course. It ensures an accurate diagnosis and avoids the risk of unnecessary laparotomy if not indicated[17]. Conclusive diagnosis in our patient was made by diagnostic laparoscopy, resulting in prompt and appropriate surgical treatment. In the presence of laparoscopic intraoperative findings such as perforation, abscesses, and mechanical obstruction, exploratory laparotomy with resection of the diseased bowel and primary anastomosis is appropriate. Other procedures, such as simple closure or excision are associated with a three-fold mortality rate[18]. Moreover, compared with duodenal diverticula, jejunoileal diverticula are nearly 4 times more likely to develop complications, and nearly 18 times more likely to perforate and develop abscesses[8]. Based on these data, a more aggressive surgical approach can be justified in treating jejunoileal diverticulosis even in patients with chronic symptoms, hence the potential benefit of resecting symptomatic multiple jejunoileal diverticula outweighs the small risk of morbidity after elective small bowel resection[5].
In conclusion, jejunoileal diverticulosis is a rare condition that continues to present formidable challenges in diagnosis and treatment. It should not be regarded as an insignificant finding, and should be highly suspected in older patients presenting with unexplained abdominal symptoms, because it may lead to life-threatening complications and death. For patients with chronic abdominal pain, bacterial overgrowth, and syndromes of malabsorption related to jejunoileal diverticulosis, conservative management is the initial treatment option. If unresponsive to conservative treatment, and in the presence of complications, surgical resection with primary anastomosis is the preferred treatment option.