Published online Apr 14, 2007. doi: 10.3748/wjg.v13.i14.2108
Revised: January 2, 2007
Accepted: January 10, 2007
Published online: April 14, 2007
AIM: To investigate the relationship between the staging by endoscopic ultrasonography (EUS) and the expression of carcinoma metastasis associated gene in the patients with gastric carcinoma.
METHODS: Sixty-three patients with gastric cancer were diagnosed by electric gastroscopy and EUS. The preoperative staging of gastric cancer was measured by EUS and compared with pathologic staging and MMP-9 expression. Peripheral serum level of MMP-9 was measured with enzyme-linked immunosorbent assay (ELISA), while the expression of MMP-9 protein was tested with immunohistochemistry and hybridization in situ in the gastric carcinoma tissues.
RESULTS: The total accuracy of EUS in estimating invasive depth of gastric cancer was 80.95%, while that in estimating lymphatic metastasis was 73.02%. Serum MMP-9 levels were consistent with the expression of MMP-9 protein and MMP-9 mRNA in tissue, a result closely correlated with invasive degree, staging with EUS and lymphatic metastasis in gastric cancer (P < 0.05). The total accuracy of estimating invasive depth in gastric cancer was 95.22% using both EUS and MMP-9.
CONCLUSION: The MMP-9 level of preoperative serum presents the reference value for preoperative staging by EUS in the patients with gastric cancer. When serum MMP-9 level in gastric cancer is significantly high, physicians should pay closer attention to the metastasis which reaches the serosa or beyond. Combining EUS and MMP-9 improves the accuracy in deciding the invasion and metastasis in the patients with gastric carcinoma.
- Citation: Tan SY, Wang JY, Shen L, Luo HS, Shen ZX. Relationship between preoperative staging by endoscopic ultrasonography and MMP-9 expression in gastric carcinoma. World J Gastroenterol 2007; 13(14): 2108-2112
- URL: https://www.wjgnet.com/1007-9327/full/v13/i14/2108.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i14.2108
Correct preoperative staging of gastric carcinoma plays a crucial role in choosing the right therapeutic strategy, applying a proper surgical operation, improving curative effect and the patient's living quality after operation. Endoscopic ultrasonography (EUS), playing the role of both endoscope and ultrasound, is remarkably superior to computed tomography (CT) and magnetic resonance imaging (MRI), as it displays high demixing image for alimentary tract[1,2]. EUS has become a routine process for preoperative examination of patients with gastric cancer in clinical practice abroad[3,4]. However, how to avoid overstaging and understaging in the preoperative staging by EUS in gastric carcinoma remains an issue to tackle.
In order to probe into the relationship between pre-operative staging with EUS and genic expression in tumor metastasis, serum level of matrix metalloproteinase 9 (MMP-9), this study simultaneously explores the preoperative staging by EUS, postoperative pathologic stage and the protein expression of MMP-9.
A total of 63 patients (aged between 29 and 75 years) with gastric carcinoma were included in this research. The mean age of the 63 patients was 58.4 ± 15.3 years, of whom 37 patients were males and others were females. The foci of 31 subjects lied in gastric antrum and gastric angle, 13 cases in the body of the stomach, and 19 cases in cardias. Each patient was examined with gastroscope and EUS before operation. Cancerous tissue and peri-carcinoma tissue (5 cm beyond the edge of foci), which were taken immediately in surgery, were fixed with 10% formaldehyde and routinely dehydrated; then they were embedded by paraffin and cut into serial sections of 4 μm in thickness. The final diagnosis of HE-staining sections was made by two pathologists respectively. No subjects received treatment against gastric carcinoma and 3 mL of fasting peripheral venous blood were taken in the day before and a week after surgery. The supernatant liquid of blood specimens was taken and quickly stored in a refrigerator of -80°C for preparation after blood clotting. A superficial gastritis group comprised 30 subjects (aged between 26 and 72 years), among whom 18 were males and others were females; the mean age was 56.8 ± 14.2 years. Of the 30 normal control subjects (aged between 28 and 74 years), 19 subjects were males and others were females; the mean age was 57.5 ± 13.8 years.
Main instruments: Olympus GF-240 electronic gastro-scope; GF-UMQ 240 electro-ultrasonic gastroscope, 360-degree circular scan, frequency range: 7.5 MHz to 20 MHz.
Main reagents: MMP-9 mouse monoclonal antibody, S-P Kit (Fuzhou Maixin biotechnology Co, Ltd.); MMP-9 probe, hybridization in situ kit (Boster Biotechnology Co. Ltd, Wuhan, China); MMP-9 ELISA Kits (Jingmei Company, Shenzhen, China).
EUS inspection: Such methods as the water-filled balloon method, water immersion or both were adopted to inspect different foci. The hierarchical structure of foci and peri-foci was scanned with a ultrasonic transducer, and lymph nodes around stomach were inspected from the greater curvature to a lesser curvature in sequence.
Histopathological staging of gastric cancer: all patients in question were operated within two weeks after the EUS inspection; examinations performed include detailed pathologic examinations on the depth of gastric wall invasion, the invasion of surrounding tissue and lymphatic metastasis. The postoperative pathologic TN staging was selected for comparison.
MMP-9 detection: MMP-9 level in gastric carcinoma tissue was detected with S-P immunohistochemical technique; expression of MMP-9 mRNA was detected with hybridization in situ. MMP-9 level of peripheral serum was detected with ELISA.
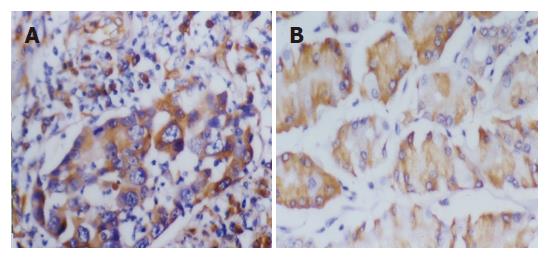
Classification criteria: Tumor cells which contain brownish yellow grains were regarded as positive. Four different visual fields were pinpointed under a high power microscope, identifying 200 cancer cells in each field. These cells were classified into four grades according to the percentage of their positive grains: no cell with positive grains was marked (-), cells with positive grains below 30% were marked (+), those with positive grains from 30% to 50% were marked (++), and those with positive grains above 50% were marked (+++). Those marked (++) or (+++) were regarded positive in immunohistochemistry and hybridization in situ. Each stained slice was reviewed in a double-blind manner.
Statistical analysis was made using the software package SPSS10.0 for Windows. The results of immunohisto-chemistry and in situ hybridization were examined by χ2 test. The results of ELISA were expressed as mean ± SD, and examined by t test. Probability value (P) below 0.05 was considered statistically significant.
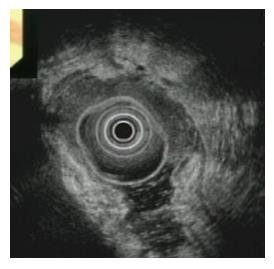
Combining gastroscope and biopsy histopathology, the diagnostic accuracy reached 93.7% (59/63) in this group (Figure 1). The diagnostic accuracy of EUS was 92.1% (58/63) (Figure 2); with gastroscope and EUS inspection combined, the diagnostic accuracy reached 100%. The preoperative stagings with EUS for 63 patients with gastric carcinoma found 9 cases (T1), 14 cases (T2); 28 cases (T3); 12 cases (T4), respectively. As for lymphatic metastases (N), 32 cases were N0, and 31 cases were N+. When pathologic staging was taken as the gold standard, the accuracy with EUS for each stage was: T1 87.50% (7/8), T2 73.33% (11/15), T3 85.19% (23/27), T4 76.92% (10/13) respectively. Seven cases were under-staged while 5 cases were over-staged; the total accuracy was 80.95% in the judgment of invasion depth in gastric cancer. The accuracy with EUS for cases staged N0 and N+ was 80.00% (20/25) and 68.4% (26/38) respectively. The staging results of 46 cases staged with EUS were in line with pathologic staging. The total accuracy of lymphatic metastasis was 73.02% (46/63).
The MMP-9 serum level of 63 preoperative patients with gastric carcinoma [(380.20 ± 295.76) ng/L] were obviously higher than that of normal group [(98.79 ± 86.43) ng/L] and that of chronic gastritis group [(110.28 ± 90.35) ng/L] (P < 0.01); the MMP-9 serum level [(145.17 ± 133.84) ng/L] of postoperative patients dropped dramatically within one week (P < 0.01), approaching normal levels. Compared with the normal control, the discrepancy was of no statistical significance (P > 0.05). The positive expression rate of MMP-9 protein was 63.49% (40/63) in 63 cases with gastric carcinoma (Figure 3A). Twenty-nine cases (78.38%) were MMP-9 positive in the tissue among 37 cases of poorly differentiated carcinoma or signet-ring cell carcinoma, while only 11 cases were MMP-9 positive among 26 cases of well-differentiated or moderately differentiated adenocarcinoma (42.31%); the discrepancy between the positive expression rates was remarkable (P < 0.05). Of 40 cases with confirmed invasion of serous membrane or further, 30 cases were MMP-9 positive (75.00%); however, among 23 cases without invaded serous membrane, only 10 cases were reported positive (43.48%). The discrepancy is statistically significant (P < 0.05). With respect to lymphatic metastasis, 29 cases (76.32%) were MMP-9 positive among 38 cases which had lymphatic metastasis; and 11 cases (44.00%) were MMP-9 positive among 25 cases without lymphatic metastasis. The discrepancy is also of statistical significance (P < 0.05) (Table 1).
| MMP-9proteinexpression | Well differentiated and moderatelydifferentiatedadencarcinoma | Poorly differentiated carcinoma and signet-ring cell carcinoma | T1 | T2 | T3 | T4 | N0 | N+ |
| --+ | 15 | 8 | 5 | 8 | 7 | 3 | 14 | 9 |
| ++-+++ | 11 | 29 | 3 | 7 | 20 | 10 | 11 | 29 |
| P | < 0.05 | < 0.05 | < 0.05 | |||||
MMP-9 and MMP-9 mRNA positive expression was not detected in 30 cases of normal gastric mucosa, while weakly positive staining was detected in 63 cases of peri-tumor tissue. In the tissues of gastric carcinoma, MMP-9 mRNA was mainly found in the matrix of cancer cells; and the positive expression rate was 63.49% (40/63), which was consistent with the results of MMP-9 immunohistochemistry (Figure 3B). The serum level and the tissue expression of MMP-9 in patients with gastric carcinoma was not interrelated with gender, age, location and dimension of tumor (P < 0.05).
The correlation between preoperative EUS staging and MMP-9 expression of gastric carcinoma was concluded (Table 2).
| EUS staging | n | Accuracy of EUS | Preoperative serum level of MMP-9 | Expression rate of MMP-9 |
| (%) | (ng/L, mean ± SD) | (%) | ||
| Depth of invasion | ||||
| T1 | 9 | 87.5 | 188.8 ± 114.6 | 25 |
| T2 | 14 | 73.3 | 230.5 ± 197.3 | 40 |
| T3 | 28 | 85.2 | 271.7 ± 251.1 | 70 |
| T4 | 12 | 76.9 | 485.6 ± 351.3 | 76.9 |
| Lymphatic metastasis | ||||
| N0 | 25 | 80.0 | 297.2 ± 201.7 | 40 |
| N+ | 38 | 68.4 | 506.6 ± 358.7 | 71.1 |
The mean level of MMP-9 in stage T1 was 188.75 ± 114.63 ng/L, and the preoperative serum level of MMP-9 rose gradually along with the depth of cancerous invasion; the MMP-9 level of stage T4 reached (485.60 ± 351.36) ng/L, which was the highest in all stages. In addition, the expression level of MMP-9 in tissue was consistent with that in serum as well; the MMP-9 level of stage T4 was also the highest among all stages. Although the mean serum level and tissue expression of MMP-9 in stage T1 and stage T2 were different, the discrepancy was of no statistical significance (P > 0.05); however, compared with stage T1 and T2, increment was observed in MMP-9 serum level in stage T3 and T4; and the MMP-9 serum levels were much higher in stage N+ than that in stage N0, which was of statistical significance (P < 0.05).
There was a positive correlation between MMP-9 ex-pression and EUS staging. In the 12 cases which were not correctly staged, 2 cases of stage T2 were staged T1, 2 cases of stage T3 and 3 cases of stage T4 staged T2, 1 case of stage T1 staged T2, 2 cases of stage T2 staged T3, and 2 cases of stage T3 staged T4. Among 7 cases which were under-staged, 5 cases were turned out to be stage T3 or T4; the serum level of MMP-9 reached 410 ng/mL, though they were confirmed as stage T2 by EUS. Among 5 cases which were over-staged, 4 cases were pathologically confirmed stage T2 or T3; the MMP-9 serum level was 220 ng/L. Combining EUS inspection and detection of MMP-9 level, the total accuracy for the determination of invasion depth of gastric cancer reached 95.22%.
The correct staging for carcinoma is significant for reaching a reasonable treatment option and evaluating the prognosis; therefore, preoperative staging plays an important role in the diagnostic model of modern medicine. In the preoperative diagnosis of gastric cancer, EUS is greatly superior to other methods available in that the ultrasound transducer installed on the tip of the endoscope can get closer to foci inside the body, presenting a more accurate and de-tailed resultant ultrasound image than those obtained with traditional ultrasound[4]. Moreover, high consistency can be identified between results of EUS and that of postoperative pathology. It is indicated in our research that the diagnostic accuracy with EUS was 87.50% (T1), 73.33% (T2), 85.19% (T3), 76.92% (T4), respectively; and the diagnostic accuracy for lymphatic metastasis was 80.00% (N0), and 68.42% (N+), respectively. The results were basically consistent with current literature[5]. However, further efforts are expected to avoid overstaging or understaging and to reflect the biological characteristics of gastric cancerous tissue through preoperative staging.
Matrix metalloproteinases (MMPs) are a group of proteinases that can digest extra-cellular matrix and basal membrane. In the process of invasion and metastasis of cancer cells, it is necessary for them to break the barrier formed by extra-cellular matrix and basal membrane[6,7]. MMP-9 is an important member of MMP-9 family; it is widely regarded as proteinase that correlates closely with invasion and metastasis of tumor. MMP-9 can degrade extra-cellular matrix and basal membrane and promote invasion and metastases of cancer cells. In our research, the serum levels of MMP-9 in 63 preoperative patients with gastric carcinoma was remarkably higher than that of normal control and that of chronic gastritis group (P < 0.01). The MMP-9 serum levels rose gradually along with the depth of cancerous invasion in patients with gastric carcinoma; the MMP-9 serum levels in patients with invaded serous membrane (T3, T4) were much higher than that of those without suffered (T1, T2). Furthermore, the MMP-9 serum levels are obviously higher in patients with lymphatic metastasis than those without. Our research identifies the consistency between MMP-9 serum levels and MMP-9 protein expression in tissue of our subjects. There is a high MMP-9 protein expression in the tissue of subjects with high MMP-9 serum levels; the MMP-9 serum levels are much higher in subjects with positive expression of MMP-9 protein than those without. It indicates that gastric cancer tissue can secrete much MMP-9, which participates in the degradation of collage IV of basal membrane. Not only can MMP-9 make invasion in situ but break extracellular membrane (ECM) barrier and vessel wall, and finally prepare for successful metastasis.
Preoperative EUS reflects the extent of invasion of gastric cancer; it is not yet satisfactory, even if the total accuracy of depth of cancerous invasion and lymphatic metastases by EUS was 80.95% and 73.02% respectively. It is worthwhile mentioning that 7 cases were under-staged and 5 cases were over-staged with EUS. Combining preoperative EUS and the detection of MMP-9 serum level combined, the accuracy of judgment on the depth of invasion will be significantly raised up to 95.22%. This combination can also make up for insufficiencies of EUS staging. Possible causes for unsatisfactory EUS staging are as follows: with respect to early gastric cancer, routine EUS is not satisfactory in diagnostic accuracy of invasion depth, especially when scanning the gastric antrum or gastric notch. This setback may be caused by the ultrasonic transducer placed too close to the gastric wall, preventing ultrasound from efficiently focusing on foci. However, a water-filled space between the transducer and gastric wall will press gastric wall directly, which obscures the display of the inner three layers of gastric wall. It is difficult to come to a precise judgment on the depth of the invasion. Besides, the overstaging of early gastric cancer is correlated with deep-seated fibrosis. It seems that EUS with a small ultrasonic transducer is superior to the routine EUS when scanning superficial or small foci. In evaluation of the invasion depth, EUS is optimal for progressive gastric cancer, as the mean accuracy is over 80%. In addition, it is also effective in the evaluation of peri-gastric lymphatic metastases. Failure to detect the tiny invasive foci outside the sub-mucosa should be responsible for the understaging of progressive stage gastric cancer. Combining EUS with detection of preoperative MMP-9 serum level will help improve the accuracy of evaluation on the invasion and metastases of gastric cancer.
We are grateful to all the colleagues in our laboratory for their contributions in maintaining standard conditions of the research.
In gastric carcinoma, the expression of MMP-9 was related to invasion and lymph node metastasis, but not to age and gender. High expression of MMP-9 promotes tumor metastasis. Patients with high MMP-9 expression are found with a low survival rate. However, there exists no significant relationship between MMP-9 and stage of bladder cancer.
EUS is one of the most accurate methods for assessing the locoregional extent of neoplasia in alimentary tract; it plays an important role in preoperative T and N staging of gastric carcinoma, but further efforts are expected to avoid overstaging or understaging, and to identify metastatic lymph nodes.
MMP-9 was reported to be associated with tumor biological characteristic. Inhibition of the enzyme activity of MMP-9 might become a novel therapeutic strategy of cancer. EUS and EUS-guided techniques are found superier not only in diagnosis but also in treatment of pathological changes.
MMP-9 was reported as playing an important role in the development and metastasis in such cancers as hepatocellular carcinoma, gastric carcinoma, and bladder cancer. Some reports found MMP-9 level in serum or tissue likewise associated with tumor stage. EUS was widely used in diagnosing and judging the location and resectability of carcinoma; however, few reports probe into the combination of EUS and MMP-9 level. Our research found improved accuracy of EUS in staging tumors when used together with MMP-9 level detection.
Endoscopic color Doppler ultrasonography (ECDUS) can further increase the accuracy of diagnosis by clearly presenting blood signal of tissue. High resolution EUS (HREUS) can display distinctly the five-layer structure of the alimentary tract, which is superior to MRI and CT. Among mushrooming new techniques, EUS emerges as a superior technique in clinical practice, such as EUS-guided pancreatic pseudocyst drainage, EUS-guided celiac plexus neurolysis (EUS-CPN), endoscopic mucosal resection (EMR), EUS-guided radio frequencv ablation (EUS-RFA), EUS-guided needle injection (EUS-FNI), to name a few.
Endoscopic Ultrasonography (EUS): A procedure that combines endoscopy and ultrasound to obtain images and information on the digestive tract and the surrounding tissue and organs. In EUS, a small ultrasound transducer is installed on the tip of the endoscope, allowing the transducer to get closer to the organs inside the body. Therefore, the resultant ultrasound images are often more accurate and detailed than those obtained by traditional ultrasound; Matrix Metalloproteinase: A member of a group of enzymes that can break down proteins, such as collagen, that are normally found in the spaces between cells in tissues. Because these enzymes need zinc or calcium atoms to work properly, they are called metalloproteinases. They are involved in wound healing, angiogenesis, and tumor cell metastasis; Enzyme-linked Immunosorbent Assay (ELISA): A sensitive laboratory test method that relies on an enzymatic conversion reaction and is used to detect the presence of specific substances (such as enzymes or viruses or antibodies or bacteria); hybridization in situ: A laboratory test that locates a gene or gene product by adding specific radioactive or chemically tagged probes for the gene and locates the radioactivity or chemical on the chromosome or in the cell after hybridization.
The approach of combining EUS and a MMP-9 as biomarker is an innovative way of studying prognosis in gastric cancer by means of translational research; it gives a clear delineation of the research background, objectives, materials and methods, results and conclusions. The design of the controls is rational. Tables and figures reflect the major findings of the study and they are appropriately presented, and the references are appropriate.
S- Editor Wang J L- Editor Ma JY E- Editor Liu Y
| 1. | Huang YH, Jia XJ, Wan GS, Xie YR. Comparison of value between the preoperative staging of digestive tract cancer of EUS and that of CT. Zhonghua Chaosheng Yingxiangxue Zazhi. 2000;9:681-685. |
| 2. | Li YQ, Zhong L, Li WJ, Chen J, Yu T, Zhao YA. The value of diagnosis of fine needle aspiration biopsy guided by EUS to the diseases of upper gastrointestinal tract and neighbor organs. Zhonghua Chaosheng Yingxiangxue Zazhi. 2004;13:910-912. |
| 3. | Willis S, Truong S, Gribnitz S, Fass J, Schumpelick V. Endoscopic ultrasonography in the preoperative staging of gastric cancer: accuracy and impact on surgical therapy. Surg Endosc. 2000;14:951-954. [PubMed] [DOI] [Full Text] |
| 4. | Massari M, Cioffi U, De Simone M, Bonavina L, D'elia A, Rosso L, Ferro C, Montorsi M. Endoscopic ultrasonography for preoperative staging of gastric carcinoma. Hepatogastroenterology. 1996;43:542-546. [PubMed] |
| 5. | Chen CH, Yang CC, Yeh YH. Preoperative staging of gastric cancer by endoscopic ultrasound: the prognostic usefulness of ascites detected by endoscopic ultrasound. J Clin Gastroenterol. 2002;35:321-327. [PubMed] [DOI] [Full Text] |
| 6. | Parsons SL, Watson SA, Brown PD, Collins HM, Steele RJ. Matrix metalloproteinases. Br J Surg. 1997;84:160-166. [PubMed] [DOI] [Full Text] |
| 7. | Kabashima A, Maehara Y, Kakeji Y, Baba H, Koga T, Sugimachi K. Clinicopathological features and overexpression of matrix metalloproteinases in intramucosal gastric carcinoma with lymph node metastasis. Clin Cancer Res. 2000;6:3581-3584. [PubMed] |