Published online Mar 21, 2007. doi: 10.3748/wjg.v13.i11.1755
Revised: January 3, 2007
Accepted: February 25, 2007
Published online: March 21, 2007
A 26-year-old woman with ulcerative colitis was transferred to our hospital with left hemiparesis due to cerebral infarction. Cervical ultrasonography and magnetic resonance imaging angiography revealed thrombosis at the right common carotid artery and the right internal carotid artery. Antithrombotic and anticoagulant therapies were commenced. After about 2 wk of the treatment, the frequency of her diarrhea increased. She underwent emergency subtotal colectomy, but 10 d later an abundant hemorrhage from the remnant rectum occurred, so the remnant rectum was resected and an ileal pouch anal anastomosis was performed. Antithrombotic and anticoagulant therapies were continued, but neither her neurological status nor magnetic resonance imaging angiography findings showed subsequent changes. She was discharged 3 mon after operation. This is a rare case of common carotid arterial thrombosis occurring as a complication of ulcerative colitis, in which antithrombotic and anticoagulant therapies are considered to provoke a deterioration of the patient’s bowel disease.
- Citation: Nogami H, Iiai T, Maruyama S, Tani T, Hatakeyama K. Common carotid arterial thrombosis associated with ulcerative colitis. World J Gastroenterol 2007; 13(11): 1755-1757
- URL: https://www.wjgnet.com/1007-9327/full/v13/i11/1755.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i11.1755
Ulcerative colitis (UC) is often complicated with various extra-intestinal manifestations during the course of the disease. Of the secondary conditions, thromboembolic events are rare but well-recognized[1-4]. Furthermore, cerebral infarction due to arterial thrombus occurs as a very rare complication. However, the treatment of thrombosis associated with UC is controversial, and the indications for surgery have not been established. Here, we report a case of UC in a young woman who suffered from cerebral infarction due to thrombosis of the common carotid artery.
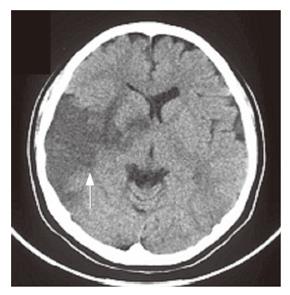
A 26-year-old woman was admitted to another hospital on January 23, 2004 for frequent bloody diarrhea. A diagnosis of UC relapse was made and she was administered soluble prednisolone. Three days after admission, she was found lying on the floor. She was conscious and alert, but physical examination revealed left hemiparesis. Urgent computed tomography showed an area of low density in the right temporal lobe (Figure 1), and a diagnosis of cerebral infarction was made. Because of concerns that bleeding from the large intestine might increase, she did not undergo aggressive anticoagulant therapy, but only received osmotic diuretics. After 1 wk of the therapy, no improvement was found in her bloody diarrhea and hemiparesis, so she was transferred to our hospital on February 3, 2004.
On admission, she was moderately emaciated (48 kg, 162 cm), and her temperature was 37.8°C. She was conscious, with left hemiparesis but no pathological reflexes. The conjunctivae were anemic but not icteric. A total dose of steroids of 8350 mg was administered for about 4 years. Her electrocardiogram was normal but biochemical tests revealed severe anemia (hemoglobin, 6.7 g/dL, hematocrit, 21.5%), hypoproteinemia (total protein, 4.6 g/dL, albumin, 2.3 g/dL) and an elevation of her C-reactive protein levels and erythrocyte sedimentation rate. A coagulation test revealed no signs of hypercoagulability such as thrombocytosis. Immunological examination revealed no autoimmunoantibody, and Lupus anti-coagulant was also negative. Her protein C level (105%), APL (111%) and PLG (93%) were within normal range.
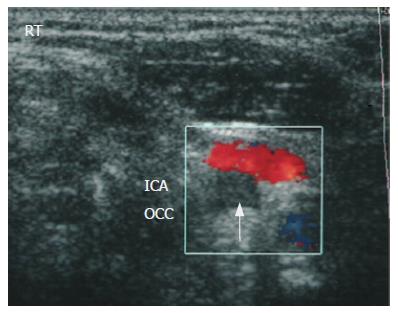
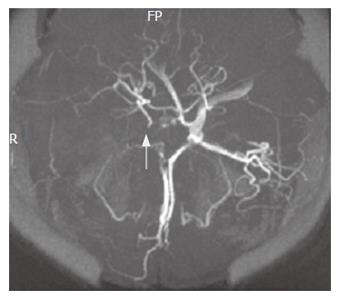
Cervical ultrasonography found a complete occlusion of the right internal carotid artery (Figure 2). In magnetic resonance imaging angiography (MRA), the right common carotid artery was occluded (Figure 3) and the right middle cerebral artery was not detectable (Figure 4). Ultrasonic cardiography did not reveal any thrombus in the left atrium. It was suspected that the cerebral infarction was a complication of her UC. Heparin (15 000 units/d) was administered for the cerebral infarction, and conservative treatment for UC (soluble prednisolone) was continued. Fourteen days after admission, remarkable bloody diarrhea occurred (53 episodes/d), and we decided to perform an emergency subtotal colectomy. As thrombosis was still an active disease, we decided to continue the anticoagulant therapy. Ten days after the first operation, massive bleeding from the remnant rectum occurred, so we resected the remnant rectum and colon, and performed an ileal pouch anal anastomosis, with a diverting ileostomy. Antithrombotic therapy was continued. No subsequent changes were observed in the patient’s neurologic status, including her left hemiparesis. Three months after operation, she was transferred to another hospital for rehabilitation.
Thromboembolic complications of UC are uncommon with a reported incidence of 1.2%-7.5%, but well recognized because of their high mortality[1-4]. Cerebral infarction associated with UC is particularly rare, but is clinically important because of its high morbidity and mortality[5-7]. Prior to this case, there had been only 2 reported instances of cerebral infarction caused by carotid arterial thrombosis in association with UC[8,9].
The pathogenesis of thrombosis in UC remains unclear[7,10-15]. Many reports have suggested that hypercoagulability in UC may predispose patients to arterial and venous thromboses[11-15]. Previous reports also indicated that prothrombotic events occur more frequently during the active phase of UC than during remission[8,9,11,15]. However, there have been some case reports of thromboembolic events occurring during the remission phase of UC. In the present case, the cerebral infarction occurred during a rapid recurrence of UC, and the relapse of UC may have triggered the thrombosis.
Antithrombotic therapies for thromboembolism associated with inflammatory bowel disease (IBD) are controversial[16,17]. Anticoagulant therapy is considered by some authors to be unnecessary and potentially dangerous, because of the possibility that it may promote mucosal bleeding from the UC lesion. In contrast, others have suggested that aggressive anticoagulant therapy may be useful for thrombosis that arises as a complication of IBD[18,19]. In the present case, only an osmotic diuretic was used in the early stage of the cerebral infarction. We should mention that it was late to use heparin for thrombosis. Although the hemorrhage might deteriorate, we used aggressive anticoagulant therapy because thrombosis of the common carotid artery was detected by cerebral ultrasonography and MRA. Unfortunately, her bloody stool increased markedly, and she twice required emergency surgery. After ileal pouch anal anastomosis, her general condition improved, and anticoagulant therapy was continued safely. However, her left hemiparesis did not improve and thrombus was still detected at the right common carotid artery by cervical ultrasonography and MRA. Although the thrombus unlikely disappear, anticoagulant therapy has been continued to prevent extension of the thrombus. Ongoing rehabilitation will be needed to improve her mobility.
Several factors may explain thromboembolism in IBD. Platelets and coagulation cascade abnormalities are likely to play a key role in clot formation in IBD[11,12,20]. Thrombophilias are found in 33%-50% of patients in the general population with venous thromboembolism[21,22], and factor V Leiden mutation or activated protein C (APC) resistance is the most frequent genetic abnormality[15]. In IBD patients, the incidence of APC resistance or factor V Leiden mutation might no be increased[13,23,24]. While APC resistance itself is not possibly associated with IBD, it does appear to increase the risk of thromboembolic events when present[14]. In this case, the platelet count was within the normal range, but neither platelet aggregation nor coagulation cascade activation was examined, and no thrombophilia evaluation was performed.
Craig et al[15] suggested that due to the relatively high frequency of identifiable thrombophilia, all IBD patients with venous thromboembolism should undergo a comprehensive thrombophilia evaluation. They also suggested that the presence of a hypercoagulable condition might be a relative indication for lifelong anticoagulation with Warfarin[18].
Some authors have reported that medically treated patients develop thrombotic complications more often than surgically treated patients[2,3]. However, a rare instance of cerebral venous thrombus 10 years after panproctocolectomy has been recorded[25], and Craig et al[15] reported that proctocolectomy is not protective for recurrent thromboembolism. Our patient needed proctocolectomy for abundant hemorrhage from the large intestine in poor general condition. It is unlikely that marked bloody diarrhea is associated with conditions that promote the development of thrombus. If evaluations for thrombophilias were performed and at least one of them was identified, bloody diarrhea might be a relative indication for proctocolectomy. We consider that early proctocolectomy should have protected our patient from thromboembolism.
We have described here our experience with one case of common carotid arterial embolism associated with UC. Cervical ultrasonography and MRA were useful for identification of the thrombus. Further work is required to clarify the correlation between IBD and the thrombophilias, and to evaluate the role of anticoagulant therapy and proctocolectomy in the management of these patients.
S- Editor Liu Y L- Editor Ma JY E- Editor Zhou T
| 1. | Miehsler W, Reinisch W, Valic E, Osterode W, Tillinger W, Feichtenschlager T, Grisar J, Machold K, Scholz S, Vogelsang H. Is inflammatory bowel disease an independent and disease specific risk factor for thromboembolism? Gut. 2004;53:542-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 343] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 2. | Grip O, Svensson PJ, Lindgren S. Inflammatory bowel disease promotes venous thrombosis earlier in life. Scand J Gastroenterol. 2000;35:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 89] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. III. Complications. Gut. 1964;5:1-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 516] [Cited by in RCA: 483] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001;85:430-434. [PubMed] |
| 5. | Das R, Vasishta RK, Banerjee AK. Aseptic cerebral venous thrombosis associated with idiopathic ulcerative colitis: a report of two cases. Clin Neurol Neurosurg. 1996;98:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Lam A, Borda IT, Inwood MJ, Thomson S. Coagulation studies in ulcerative colitis and Crohn's disease. Gastroenterology. 1975;68:245-251. [PubMed] |
| 7. | Novotny DA, Rubin RJ, Slezak FA, Porter JA. Arterial thromboembolic complications of inflammatory bowel disease. Report of three cases. Dis Colon Rectum. 1992;35:193-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Schneiderman JH, Sharpe JA, Sutton DM. Cerebral and retinal vascular complications of inflammatory bowel disease. Ann Neurol. 1979;5:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 91] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Chetri K, Ghoshal UC, Somani SK, Aggarwal R, Sinha N, Jain M, Naik SR. Common carotid artery occlusion causing cerebral infarction in ulcerative colitis. Indian J Gastroenterol. 2002;21:122-123. [PubMed] |
| 10. | Lee LC, Spittell JA, Sauer WG, Owen CA, Thompson JH. Hypercoagulability associated with chronic ulcerative colitis: changes in blood coagulation factors. Gastroenterology. 1968;54:76-85. [PubMed] |
| 11. | Talbot RW, Heppell J, Dozois RR, Beart RW. Vascular complications of inflammatory bowel disease. Mayo Clin Proc. 1986;61:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 408] [Cited by in RCA: 413] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 12. | Webberley MJ, Hart MT, Melikian V. Thromboembolism in inflammatory bowel disease: role of platelets. Gut. 1993;34:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 178] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 13. | Liebman HA, Kashani N, Sutherland D, McGehee W, Kam AL. The factor V Leiden mutation increases the risk of venous thrombosis in patients with inflammatory bowel disease. Gastroenterology. 1998;115:830-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Novacek G, Miehsler W, Kapiotis S, Katzenschlager R, Speiser W, Vogelsang H. Thromboembolism and resistance to activated protein C in patients with inflammatory bowel disease. Am J Gastroenterol. 1999;94:685-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Solem CA, Loftus EV, Tremaine WJ, Sandborn WJ. Venous thromboembolism in inflammatory bowel disease. Am J Gastroenterol. 2004;99:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 233] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 16. | Karacostas D, Mavromatis J, Artemis K, Milonas I. Hemorrhagic cerebral infarct and ulcerative colitis. A case report. Funct Neurol. 1991;6:181-184. [PubMed] |
| 17. | Musio F, Older SA, Jenkins T, Gregorie EM. Case report: cerebral venous thrombosis as a manifestation of acute ulcerative colitis. Am J Med Sci. 1993;305:28-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Tsujikawa T, Urabe M, Bamba H, Andoh A, Sasaki M, Koyama S, Fujiyama Y, Bamba T. Haemorrhagic cerebral sinus thrombosis associated with ulcerative colitis: a case report of successful treatment by anticoagulant therapy. J Gastroenterol Hepatol. 2000;15:688-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Hishiyama M, Kato Y, Shibui T, Hamabe Y, Sazaki N, Momoi M, Araki A. Cerebral sinus thrombosis associated with ulcerative colitis. Nihon Naika Gakkai Zasshi. 2001;90:2287-2290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Smith CJ, Haire WD, Kaufman SS, Mack DR. Determination of prothrombin activation fragments in young patients with inflammatory bowel disease. Am J Gastroenterol. 1996;91:1221-1225. [PubMed] |
| 21. | Murin S, Marelich GP, Arroliga AC, Matthay RA. Hereditary thrombophilia and venous thromboembolism. Am J Respir Crit Care Med. 1998;158:1369-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Martinelli I. Risk factors in venous thromboembolism. Thromb Haemost. 2001;86:395-403. [PubMed] |
| 23. | Zauber NP, Sabbath-Solitare M, Rajoria G, Mogan G. Factor V Leiden mutation is not increased in patients with inflammatory bowel disease. J Clin Gastroenterol. 1998;27:215-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Papa A, Danese S, Grillo A, Gasbarrini G, Gasbarrini A. Review article: inherited thrombophilia in inflammatory bowel disease. Am J Gastroenterol. 2003;98:1247-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Yerby MS, Bailey GM. Superior sagittal sinus thrombosis 10 years after surgery for ulcerative colitis. Stroke. 1980;11:294-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |