Published online Feb 21, 2006. doi: 10.3748/wjg.v12.i7.1157
Revised: July 2, 2005
Accepted: July 20, 2005
Published online: February 21, 2006
Primary liver liposarcoma is a rare disease. Because of its rarity, the knowledge of the clinical course, management, and prognosis of primary liver liposarcoma are all limited for clinicians. A 61-year-old female patient who suffered from a huge primary liposarcoma in the central portion of the liver had the clinical presentations of fever, nausea, vomiting, jaundice, and body weight loss. The huge tumor was resected successfully. However, the tumor recurred repeatedly and she had repeated hepatectomies to remove the tumor. The tumor became aggravating after repeated surgeries. Eventually, the patient had cervical spinal metastasis of liposarcoma and she survived for 26 months after liver liposarcoma was diagnosed. Although the tumor may become aggrava-ting after repeated surgeries, repeated hepatectomies are still the best policy to achieve a long-term survival for the patients.
- Citation: Kuo LM, Chou HS, Chan KM, Yu MC, Lee WC. A case of huge primary liposarcoma in the liver. World J Gastroenterol 2006; 12(7): 1157-1159
- URL: https://www.wjgnet.com/1007-9327/full/v12/i7/1157.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i7.1157
Liver neoplasm is not an uncommon disease in Asian countries. Cavernous hemangioma, adenoma, and focal nodular hyperplasia are the most common benign tumors in the liver. Hepatocellular carcinoma and cholangiocarcinoma are the most common malignant ones. Liver tumors derived or transformed from other mesenchymal cells, however, are rare. Therefore, the precise diagnosis of a benign tumor other than cavernous hemangioma, adenoma and focal nodular hyperplasia, or a malignant tumor other than hepatocellular carcinoma and cholangiocarcinoma is difficult.
Liposarcoma is not an uncommon malignant mesenchymal neoplasm. However, it is extremely rare in the liver. To our knowledge, most liposarcomas are found in lower extremities, shoulders and retroperitoneum[1]. Only few cases of primary liver liposarcoma have been reported[2]. Furthermore, most of the articles describing liver liposarcoma focus only on histopathologic and image studies. The clinical course and prognosis of primary liver sarcoma are rarely mentioned. Hence, we have presented a case of a primary huge liver liposarcoma with the clinical course and have described the outcome of the patient.
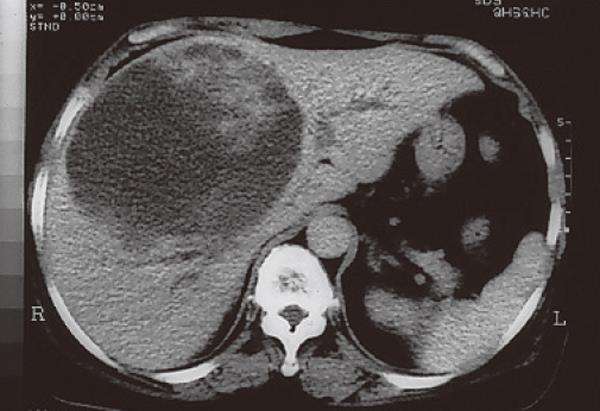
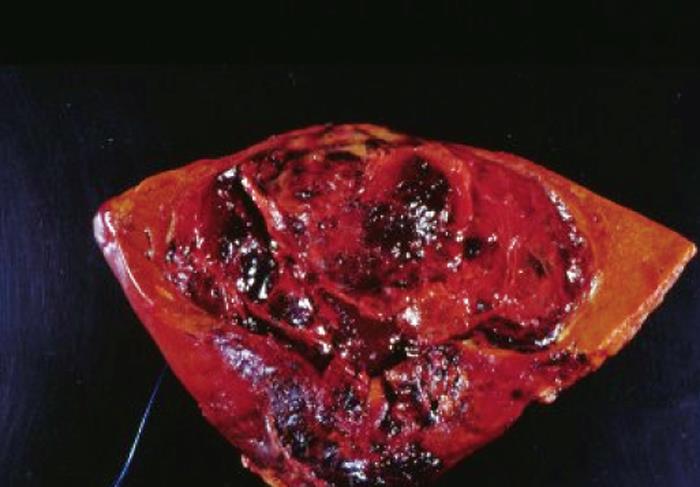
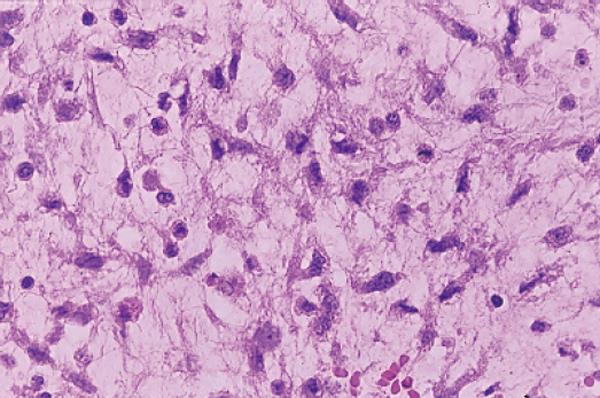
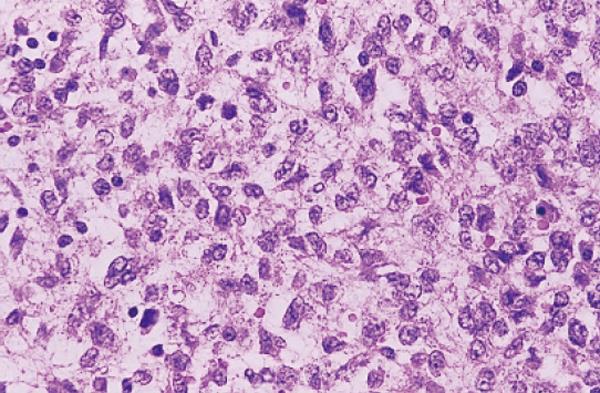
A 61-year-old woman was admitted because she had fever, nausea, vomiting, jaundice, and tea-colored urine for a week. She had lost 5 kg of body weight within a month. Physical examination revealed that she had hepatomegaly, icteric sclera, and a palpable mass over the right upper quadrant of the abdomen. Laboratory studies showed 61 mg/L total bilirubin, 702 u/L alkaline phosphate, 277 u/L gamma-glutamyl-transpeptidase, 61 u/L aspartate aminotransferase, and 18 u/L alanine aminotransferase. Virologic examination revealed that she was not infected with hepatitis B or C virus. Serum levels of α-fetoprotein and CEA were measured and both were within the normal limits. However, CA-199 was up to 92.2 U/mL (normal: <37 U/mL at this hospital). Abdominal ultrasonography showed a huge lobulated cystic lesion in the central portion of the liver. Computed tomography (CT) scan was done and demonstrated that a huge cystic lesion was located at segments 4, 5, and 8, and bilateral intrahepatic ducts were compressed (Figure 1). Aspiration cytology was done but failed to demonstrate any malignant cells. Since this patient had fever and her bilateral intrahepatic ducts were compressed by the tumors, biliary tract infection could not be ruled out as she was treated with antibiotics first. Although the tumor was difficult to locate, surgical resection was still feasible according to the imaging studies. Therefore, surgical resection of the tumor was done and a three-segmentectomy with the preservation of bilateral main intrahepatic ducts was performed. Grossly, the tumor was a cystic tumor, 11 cm × 11 cm × 13 cm in size, with multiple septa (Figure 2). Microscopically, the tumor showed the picture of a myxoid liposarcoma (Figure 3). Postoperative course was uneventful and she was discharged on the tenth postoperative day. She was followed up at our out patient clinics and liver ultrasonography was performed every 2 or 3 mo.
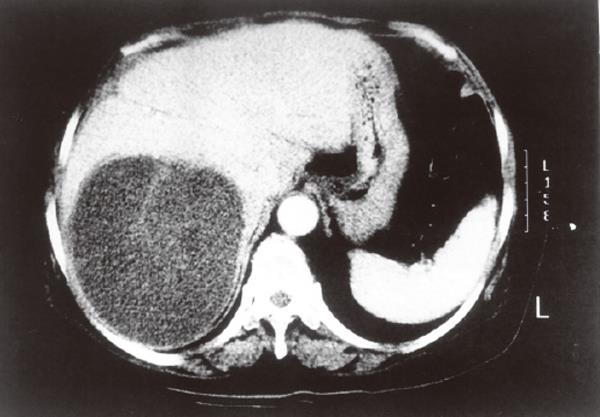
A big tumor, 9.5 cm × 10 cm × 12.4 cm in size, recurred in the right lobe of the liver 10 mo after the first surgery although liver sonography was performed regularly and no tumor was found in previous examinations (Figure 4). Hepatectomy was performed again to excise the tumor. Pathologic pictures showed that the tumor was a recurrent myxoid liposarcoma. The patient was then discharged and was followed up at our outpatient clinics. Nevertheless, a tumor, 7 cm × 9 cm × 12 cm in size, occurred again in the liver 11 months after the second surgery. Whole body bone scan with Tc-99m MDP was performed and showed negative for bony metastasis. Thereafter, hepatectomy was performed again to excise the tumor. The pathologic pictures showed undifferentiated sarcoma of the liver (Figure 5). However, the patient complained about neck pain 2 wk after the third hepatectomy. A cervical spine metastasis (C3-C4) was noted. Laminectomy was performed to remove the spinal tumor and release the spinal cord compression.
Although aggressive surgical treatments were employed to treat this liposarcoma, tumor recurred in the liver 2 mo after the last surgery. Since the patient could not tolerate further surgical interventions, radiotherapy was performed. But the tumor did not respond to radiotherapy, and her condition deteriorated. The patient died of liver failure and aspiration pneumonia five months after the last hepatic resection surgery.
Primary liver liposarcoma is rare. The experience for a surgeon or a gastroenterologist is also limited. In this case study, the patient survived for 26 mo after an aggressive treatment. Wolloch et al[3] described the first liver myxoid liposarcoma patient. The patient underwent a right hemihepatectomy and survived for 46 d only after the surgery. Subsequently, only few cases have been described[2]. Moreover, the clinical course and management of primary liver liposarcoma are rarely mentioned in these reports (Table 1). Therefore, the knowledge of primary liver liposarcoma is still limited. The results of surgical resections are unknown. The long-term prognosis for liver liposarcoma is unknown either.
| Case source | Age (yrs) | Sex | Location | Management | Results |
| Wolloch et al[3] | 22 | F | Right lobe | Right lobe hepatectomy | Survival 46 d |
| Kim and Reyes[6] | 86 | M | Capsule | Supportive treatment | NM |
| Kim et al[7] | 30 | F | Right lobe | Right lobe hepatectomy | Tumor free for 10 mo |
| Aribal et al[8] | 48 | F | Hilum | Chemotherapy | NM |
| Nelson et al[2] | 54 | F | Left lobe right lobe | Exploratory laparotomy with biopsy | Post-operative bleeding and death |
| Current study | 61 | F | Right lobe | Right lobe hepatectomy | Survival 27 mo |
Clinical course and management of primary liver liposarcoma are scarcely mentioned in previous reports because the patients were too old or had serious underlying diseases to receive a surgery, or the tumor was big-sized or located in a position difficult for complete resection. In this case, curative hepatectomy was performed although the tumor was huge. According to the clinical course, liver liposarcoma has a high rate of recurrence, which is similar to those at other sites[1,4]. Aggressive surgery can prolong the life of patients. Thus, this case provides a good experience about the clinical course of primary liver liposarcoma.
Early diagnosis of liver liposarcoma is not easy. Liver is the largest organ in the abdomen, and symptoms and signs of a tumor in the liver are usually trivial unless the tumors are large. The usual symptoms and signs of primary liver liposarcoma include jaundice, fever, nausea, vomiting, abdominal fullness, right upper quadrant pain, and body weight loss[2]. Most of the symptoms are caused either by displacement or compression of nerves, vessels, biliary tract, and intestinal structure. Our case had similar clinical presentations because of the massive effect of tumor and central location of the tumor to compress biliary tracts. Abdominal ultrasonography usually is a good tool to do preoperative screening and postoperative follow-up. In this case, abdominal ultrasonography was performed regularly at an interval of 12 wk. However, the recurrent tumor was always large when the tumor was found by ultrasonography. This implies that recurrent tumor grows rapidly between two ultrasonography examinations. Computed tomography is still the best tool to evaluate the resectability of liver liposarcoma before surgery.
Five major histologic categories of liposarcoma are mentioned[5] and patients with myxoid or well-differentiated type have a lower local recurrence rate than other types[1]. In our case, surgical specimens showed myxoid liposarcoma in the first and second time. However, the tumor exhibited high grade of undifferentiated sarcoma in the third time. The interval to recurrence in the first and second time was 10 mo and 11 mo, respectively, but recurrence interval in the third time reduced to 2 mo. The tumor pathology became aggravating after repeated surgery.
In conclusion, primary liposarcoma of the liver is rare. The experience in dealing with this malignant neoplasm is limited. In our experience, the tumor becomes aggravating with the time course or after repeated surgeries, and resists to radiotherapy. Curative and aggressive hepatectomies are still the best policy to achieve a long-term survival of the patients.
S- Editor Guo SY L- Editor Wang XL E- Editor Cao L
| 1. | Enzinger FM, Winslow DJ. Liposarcoma. A study of 103 cases. Virchows Arch Pathol Anat Physiol Klin Med. 1962;335:367-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 278] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 2. | Nelson V, Fernandes NF, Woolf GM, Geller SA, Petrovic LM. Primary liposarcoma of the liver: a case report and review of literature. Arch Pathol Lab Med. 2001;125:410-412. [PubMed] |
| 3. | Wolloch Y, Dintsman M, Garti I. Primary malignant tumors of the liver. Isr J Med Sci. 1973;9:6-11. [PubMed] |
| 4. | Enterlaine HT, Culberson JD, Rochlin DB, Brady LW. Liposarcoma. A clinical and pathological study of 53 cases. Cancer. 1960;13:932-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Enzinger FM, Weiss SW. Soft Tissue Tumors. 3rd ed. St Louis, Mo: Mosby 1995; 431-465. |
| 6. | Kim TW, Reyes CV. Myxoid liposarcoma mimicking fluid density. J Surg Oncol. 1985;30:80-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Kim YI, Yu ES, Lee KW, Park EU, Song HG. Dedifferentiated liposarcoma of the liver. Cancer. 1987;60:2785-2790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Aribal E, Berberoglu L. Primary liposarcoma of the liver. AJR Am J Roentgenol. 1993;161:1331-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |