Published online Dec 28, 2006. doi: 10.3748/wjg.v12.i48.7844
Revised: July 28, 2006
Accepted: November 27, 2006
Published online: December 28, 2006
AIM: To study the brain-gut interaction and the effect of behavioral or psychiatric conditions on irritable bowel syndrome (IBS) in an African population.
METHODS: IBS was diagnosed using the Rome II diagnostic criteria. The entry of each patient was confirmed following detailed explanations of the questions. Four hundred and eighteen patients were studied. Subjects satisfying the Rome II criteria for IBS were physically examined and stool microscopy was done to identify the presence of “alarm factors”. Depression was diagnosed using the symptom-check list adapted from the Research Diagnostic Criteria (DSM-IV) of the American Psychiatric Association.
RESULTS: Seventy-five (56.8%) of the 132 IBS patients were depressed whereas only 54 (20.1%) of the 268 non-IBS patients were depressed. There was a significant relationship between IBS and depression (χ2 = 54.29, Odds ratio = 5.21, 56.8 ± 8.4 vs 20.1 ± 5.2, P = 0.001). Even though constipation predominant IBS patients were more likely to be depressed, no significant relationship was found between the subtype of IBS and depression (χ2 = 0.02, OR = 0.95, P = 0.68).
CONCLUSION: IBS is significantly associated with major depression but not gender and bowel subtypes of the patients. Patients with IBS need to be evaluated for depression due to the highly significant relationship between the two conditions.
- Citation: Ladep NG, Obindo TJ, Audu MD, Okeke EN, Malu AO. Depression in patients with irritable bowel syndrome in Jos, Nigeria. World J Gastroenterol 2006; 12(48): 7844-7847
- URL: https://www.wjgnet.com/1007-9327/full/v12/i48/7844.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i48.7844
Irritable bowel syndrome (IBS) has been widely studied in the western world and pathophysiologic mechanisms have been available to explain the constellation of symptoms[1]. IBS is a chronic disorder of unknown etiology clinically consisting of altered bowel habits, abdominal pain and the absence of any detectable organic pathologic process[1]. Along with the putative pathophysiologic mechanisms of post-infectious inflammatory disorder, disordered intestinal motility and visceral hypersensitivity, there has been much discussion regarding the brain-gut interaction and the influence of behavioral or psychiatric conditions on these symptoms[2].
IBS is recognized widely as one of the most commonly encountered gastrointestinal disorders[1-4]. Locally, there is paucity of data concerning IBS in Africa. Of the studies available however, IBS was reported in 30 percent of an African population at the University College Hospital, Ibadan[5] and 8% in Kenya[6]. Peak prevalence of IBS was reported in the third decade of life in the study in Kenya. A more recent report from our centre demonstrated a prevalence of 26.1% among a healthy student population[7]. In addition, patients with IBS are at increased risk for other non-gastrointestinal functional disorders such as fibromyalgia[8-11] and interstitial cystitis[12]. IBS is known to co-exist with some psychiatric disorders such as depression, anxiety disorders, somatoform disorders[9,13] and sexual dysfunction (e.g., dyspareunia)[14]. The situation is however, not known in African population. This study aims at determining the prevalence of depression among African IBS patients.
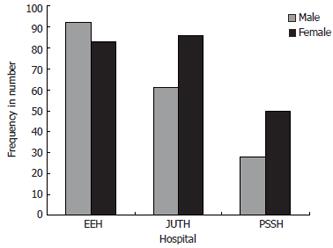
This is a descriptive cross-sectional study. The principal investigator administered the questionnaire after obtaining informed consent to randomly selected subjects attending the General Outpatient (GOP) Clinics of the three hospitals in Jos. These hospitals were: Jos University Teaching Hospital (JUTH), Evangel Hospital (EEH) and Plateau State Specialist Hospital (PSSH). The GOP clinics of these hospitals are where primary care physicians attend to patients prior to referrals for specialist care. On selected days of the week, the investigators went to the various clinics until the proposed study sample size was achieved.
The number of patients visiting each of the GOP clinics in the previous year was used to divide the total sample to be studied proportionately. This was obtained from the records of the hospitals. Individual patients were randomly selected in each GOP clinic. Every fifth patient at EEH, every fourth patient at JUTH and alternate patient at PSSH were selected, subject to satisfying the inclusion criteria.
The study was approved by the Ethics Committee of the three hospitals prior to the commencement of the study. The study at EEH was conducted between July 2003 and September 2003, PSSH between October and November 2003, and JUTH between December 2003 and February 2004. Each patient’s entry was confirmed following detailed explanations of the questions. Subjects satisfying the Rome II criteria for IBS were physically examined to identify the presence of “alarm factors.” Major depression was diagnosed using the symptom-check list adapted from the Research Diagnostic Criteria (DSM-IV) of the American Psychiatric Association[15].
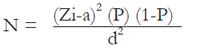
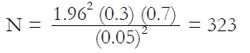
The minimum sample size was determined based on the prevalence reported in the literature using the following formula:
Math 1
N = minimum sample size; P = best estimate of prevalence of IBS from the literature review expressed as a fraction of 100 (in this case, 30% = 0.3)[5]; Zi-a = a constant at 95% confidence interval for a two-tailed descriptive study (= 1.96); d = absolute precision, i.e. value required (in percentage) which in actual terms describes the maximum difference between the population rate and the sample rate that can be tolerated. Five percent (0.05) was adapted for this study. Thus:
Math 2
However, 400 subjects were recruited for the study. Systematically selected adult patients aged 18 to 50 years attending the GOP clinics of the three hospitals were included and the pregnant women and subjects using laxatives for any reason, those with memory problems and the presence of alarm symptoms, including a positive stool test for helminthes were excluded from the study.
The 400 patients who attended the three selected hospitals and who satisfied the inclusion criteria were studied with the questionnaires by the principal investigator. Four hundred and eighteen patients were initially evaluated, but 18 were excluded for various reasons. Six were above 50 years of age, 4 had significant weight loss, 5 could not give a coherent history, 2 declined to participate in the study and 1 had recurrent bloody stools. Of the 400 subjects, 174 were from ECWA Evangel Hospital, 148 from Jos University Teaching Hospital, and 78 from Plateau State Specialist Hospital.
Data were analysed using the Epi Info 2000 Statistical Program[16]. Means and standard deviations were used to describe continuous variables and proportions for categorical data. Two-tailed Student’s t test and analysis of variance (ANOVA), a parametric test for inequality of population means, were used for comparison of group means while the significance of observed differences (proportions) was determined by Chi-square test. P < 0.05 was considered statistically significant.
The mean age of the study population at EEH, JUTH and PSSH were 32.5 ± 9.3, 32.0 ± 10.0 and 31.1 ± 8.8 years, respectively and with an age range of 18-50 years at each hospital. There was no statistically significant difference in the mean age among the three study populations (f = 0.62, P = 0.54). Figure 1 shows the gender distribution of the study population in the three GOP clinics. Eighty-three (47.4%) females and 92 (52.6%) males were recruited at the EEH, while 86 (58.5%) females and 61 (41.5%) males were recruited at JUTH. Fifty (64.1%) females and 28 (35.9%) males were selected at PSSH.
The mean age of this population was 32.0 ± 9.4 years with a range of 18-50 years. The mean age for females was 31.9 ± 9.5 years and males 32.1 ± 9.3 years, showing no statistically significant difference (t = 0.2, P = 0.8). Subjects in the third decade of life predominated over the other age groups, and the number of females was higher than their male counterparts.
Table 1 gives a summary of this relationship. Seventy-five (56.8%) of the 132 IBS patients were depressed whereas only 54 (20.1%) of the 268 non-IBS patients were depressed. There was a significant relationship between IBS and depression (Odds ratio = 5.21, χ2 = 54.29, P = 0.001). There was no significant relationship between the gender of the IBS patients and depression (Odds ratio = 0.95, χ2 = 0.02, P = 0.89) (Table 2). Even though constipation predominant IBS patients were more likely to be depressed, Table 3 shows that no significant relationship exists between the subtype of IBS and depression (χ2 = 0.77, P = 0.68). No significant difference was observed between the gender of the population and the subtypes of IBS.
| IBS | Depressed n (%) | Not depressed n (%) | Total (n) |
| Yes | 75 (56.8) | 57 (43.2) | 132 |
| No | 54 (20.1) | 214 (79.9) | 268 |
| Total | 129 (32.3) | 271 (67.7) | 400 |
| Depression | Male n (%) | Female n (%) | Total (n) |
| Yes | 32 (42.7) | 43 (57.3) | 75 |
| No | 25 (43.9) | 32 (56.1) | 57 |
| Total | 57 (43.2) | 75 (56.8) | 132 |
| Subtype | Depression n (%) | No depression n (%) | Total (n) |
| Constipation | 36 (61.0) | 23 (39.0) | 59 |
| Diarrhoea | 31 (53.4) | 27 (46.6) | 58 |
| Alternator | 8 (53.3) | 7 (46.7) | 15 |
| Total | 75 (56.8) | 57 (43.2) | 132 |
Seventy-five (56.8%) IBS patients were depressed compared with 54 (20.1%) of the 268 non-IBS patients fulfilled the DSM IV criteria for depression. There was a highly significant relationship between IBS and depression (χ2 = 54.29, Odds ratio = 5.21, P < 0.001). This compares well with western studies that reported 60% psychiatric co-morbidity among their IBS patients who have sought healthcare[17,18]. Abnormal psychologic features have been recorded in a large percentage of patients with IBS. In a study by McDonald and others[19] involving 35 patients with IBS and 32 patients with non-IBS disease, 20% of the non-IBS group had diagnosable psychiatric disorders when compared with 53% of the IBS group. This high prevalence of depression among our cohort is most likely due to the fact that it was a study among a patient population. Most western community-based studies and a recent study done by us among stable students showed that the rate of depression was comparable to that among the non-IBS group[7,17]. Indeed, co-morbidities such as psychological symptoms are recognized factors that affect healthcare seeking of IBS patients[20].
Most investigators have found that psychiatric features predate the onset of bowel symptoms or occur concurrently, suggesting that it is not the bowel symptoms of IBS that induce psychiatric diseases[4]. Many theories have implicated the role of depression in IBS[9,14]. In addition, serotonin and catecholeamines (neurotransmitters that play some role in depression), have been shown to be in excess in patients with IBS[21-23]. Emotional stress can trigger bowel hypermotility both in normal subjects and in patients with IBS[24]. These events are associated with development of both organic and functional abdominal illness[25]. Moreover, the existing evidence suggests that treating depression and anxiety can improve the patient’s gastrointestinal distress.
There was no significant difference between the gender of the IBS patients and depression, implying that both men and women are equally prone to depression. Even though, a trend was observed in constipation-predominant IBS and depression, there was no statistically significant relationship (P = 0.68). This finding agrees with that by Whitehead et al[26].
IBS is significantly associated with major depression, but not with gender and bowel subtypes of the patients. Patients with IBS need to be evaluated for depression due to the highly significant relationship that exists between the two conditions.
The RomeIIcriteria has been widely validated in the western world and found to have a positive predictive value of 98%[27]. In our setting however, where a lot of helminthic and protozoa infestations exist, it is unclear whether the subjects fulfilling these criteria truly have IBS or not. A subset of the patients who had their stools evaluated for these infestations did not change the pre-examination diagnosis of IBS. This is a subject for further evaluations.
We are grateful to the chief executives of the three hospitals, heads of departments of the GOP clinics of the three hospitals for using their patients.
Irritable bowel syndrome (IBS) has been widely studied in the western world and many pathophysiologic mechanisms have been provided to explain the constellation of symptoms. Along with the putative pathophysiologic mechanisms of post-infectious inflammatory disorder, disordered intestinal motility and visceral hypersensitivity, there has been much discussion regarding the brain-gut interaction and the influence of behavioral or psychiatric conditions on these symptoms.
IBS is known to co-exist with some psychiatric disorders such as depression, anxiety disorders, somatoform disorders and sexual dysfunction (e.g., dyspareunia). The situation is however, not known in African populations. This study aimed at determining the prevalence of depression among African IBS patients.
IBS is significantly associated with major depression. Patients with IBS need to be evaluated for depression due to the highly significant relationship between the two conditions. The Rome criteria has been widely validated in the Western world and found to have positive predictive value of 98%. It is necessary to validate this criteria in the African setting, where a lot of helminthic and protozoa infestations exist that may be confused with IBS.
IBS is a chronic disorder of unknown etiology clinically consisting of altered bowel habits, abdominal pain and the absence of any detectable organic pathologic process. Depression is a state of low mood, loss of interest and energy that may result in suicidal ideation or act.
This is a well-done and interesting study on co-expression of depression and IBS in an African population.
S- Editor Wang GP L- Editor Ma JY E- Editor Bi L
| 1. | Horwitz BJ, Fisher RS. The irritable bowel syndrome. N Engl J Med. 2001;344:1846-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 132] [Article Influence: 5.5] [Reference Citation Analysis (2)] |
| 2. | Dunphy RC, Verne GN. Drug treatment options for irritable bowel syndrome: managing for success. Drugs Aging. 2001;18:201-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1502] [Cited by in RCA: 1427] [Article Influence: 44.6] [Reference Citation Analysis (1)] |
| 4. | Hasler WL, Owyang C. Irritable Bowel Syndrome. Textbook of Gastroenterology. Philadelphia: JB Lippincott Company 1991; 1696-1714. |
| 5. | Olubuyide IO, Olawuyi F, Fasanmade AA. A study of irritable bowel syndrome diagnosed by Manning criteria in an African population. Dig Dis Sci. 1995;40:983-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Lule GN, Amayo EO. Irritable bowel syndrome in Kenyans. East Afr Med J. 2002;79:360-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Okeke EN, Agaba EI, Gwamzhi L, Achinge GI, Angbazo D, Malu AO. Prevalence of irritable bowel syndrome in a Nigerian student population. Afr J Med Med Sci. 2005;34:33-36. [PubMed] |
| 8. | Azpiroz F, Dapoigny M, Pace F, Müller-Lissner S, Coremans G, Whorwell P, Stockbrügger RW, Smout A. Nongastrointestinal disorders in the irritable bowel syndrome. Digestion. 2000;62:66-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications. Gastroenterology. 2002;122:1140-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 775] [Cited by in RCA: 774] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 10. | Sperber AD, Atzmon Y, Neumann L, Weisberg I, Shalit Y, Abu-Shakrah M, Fich A, Buskila D. Fibromyalgia in the irritable bowel syndrome: studies of prevalence and clinical implications. Am J Gastroenterol. 1999;94:3541-3546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 152] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Veale D, Kavanagh G, Fielding JF, Fitzgerald O. Primary fibromyalgia and the irritable bowel syndrome: different expressions of a common pathogenetic process. Br J Rheumatol. 1991;30:220-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 133] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Terruzzi V, Magatti F, Quadri G, Tenore C, Minoli G, Belloni C. Bladder dysfunction and irritable bowel syndrome. Am J Gastroenterol. 1992;87:1231-1232. [PubMed] |
| 13. | Osterberg E, Blomquist L, Krakau I, Weinryb RM, Asberg M, Hultcrantz R. A population study on irritable bowel syndrome and mental health. Scand J Gastroenterol. 2000;35:264-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Walker EA, Katon WJ, Roy-Byrne PP, Jemelka RP, Russo J. Histories of sexual victimization in patients with irritable bowel syndrome or inflammatory bowel disease. Am J Psychiatry. 1993;150:1502-1506. [PubMed] |
| 15. | American Psychiatric Association. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington DC: American Psychiatric Association 1994; 320-327. |
| 16. | Epi Info 2000 (version 1.1.2a) statistical program. Epi-demiology Program office, Centers for Disease Control. Atlanta Georgia. Accessed March 25. Washington DC: American Psychiatric Association 2002; Available from: http://www.cdc.gov/epo/epiinfo.htm.. |
| 17. | Whitehead WE, Bosmajian L, Zonderman AB, Costa PT Jr, Schuster MM. Symptoms of psychologic distress associated with irritable bowel syndrome. Comparison of community and medical clinic samples. Gastroenterology. 1988;95:709-714. [PubMed] |
| 18. | Almy TP, Abbot FK, Hinkle LE Jr. Alterations in colonic function in man under stress; hypomotility of the sigmoid colon, and its relationship to the mechanism of functional diarrhea. Gastroenterology. 1950;15:95-103. [PubMed] |
| 19. | MacDonald AJ, Bouchier IA. Non-organic gastrointestinal illness: a medical and psychiatric study. Br J Psychiatry. 1980;136:276-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 76] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Drossman DA, McKee DC, Sandler RS, Mitchell CM, Cramer EM, Lowman BC, Burger AL. Psychosocial factors in the irritable bowel syndrome. A multivariate study of patients and nonpatients with irritable bowel syndrome. Gastroenterology. 1988;95:701-708. [PubMed] |
| 21. | Talley NJ. Review article: 5-hydroxytryptamine agonists and antagonists in the modulation of gastrointestinal motility and sensation: clinical implications. Aliment Pharmacol Ther. 1992;6:273-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 119] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Drossman DA. Sexual and physical abuse and gastrointestinal illness. Scand J Gastroenterol Suppl. 1995;208:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Stewart GT. Post-dysenteric colitis. Br Med J. 1950;1:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Almy TP, Tulin M. Alterations in colonic function in man under stress; experimental production of changes- simulating the irritable colon. Gastroenterology. 1947;8:616-626. [PubMed] |
| 25. | Creed F, Craig T, Farmer R. Functional abdominal pain, psychiatric illness, and life events. Gut. 1988;29:235-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 115] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Whitehead WE, Crowell MD, Robinson JC, Heller BR, Schuster MM. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 291] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | Vanner SJ, Depew WT, Paterson WG, DaCosta LR, Groll AG, Simon JB, Djurfeldt M. Predictive value of the Rome criteria for diagnosing the irritable bowel syndrome. Am J Gastroenterol. 1999;94:2912-2917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 162] [Article Influence: 6.2] [Reference Citation Analysis (0)] |