Published online Nov 14, 2006. doi: 10.3748/wjg.v12.i42.6889
Revised: October 1, 2006
Accepted: October 6, 2006
Published online: November 14, 2006
AIM: To detect the hemodynamic alterations in collateral circulation before and after combined endoscopic variceal ligation (EVL) and splenectomy with pericardial devascularization by ultrasonography, and to evaluate their effect using hemodynamic parameters.
METHODS: Forty-three patients with esophageal varices received combined EVL and splenectomy with pericardial devascularization for variceal eradication. The esophageal vein structures and azygos blood flow (AZBF) were detected by endoscopic ultrasonography and color Doppler ultrasound. The recurrence and rebleeding of esophageal varices were followed up.
RESULTS: Patients with moderate or severe varices in the esophageal wall and those with severe peri-esophageal collateral vein varices had improvements after treatment, while the percentage of patients with severe para-esophageal collateral vein varices decreased from 54.49% to 2.33%, and the percentage of patients with detectable perforating veins decreased from 79.07% to 4.65% (P < 0.01). Color Doppler flowmetry showed a significant decrease both in AZBF (43.00%, P < 0.05) and in diameter of the azygos vein (28.85%, P < 0.05), while the blood flow rate was unchanged. The recurrence rate of esophageal varices was 2.5% (1/40, mild), while no re-bleeding cases were recorded.
CONCLUSION: EVL in combination with splenectomy with pericardial devascularization can block the collateral veins both inside and outside of the esophageal wall, and is more advantagious over splenectomy in combination with pericardial devascularization or EVL in preventing recurrence and re-bleeding of varices.
- Citation: Liu B, Deng MH, Lin N, Pan WD, Ling YB, Xu RY. Evaluation of the effects of combined endoscopic variceal ligation and splenectomy with pericardial devascularization on esophageal varices. World J Gastroenterol 2006; 12(42): 6889-6892
- URL: https://www.wjgnet.com/1007-9327/full/v12/i42/6889.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i42.6889
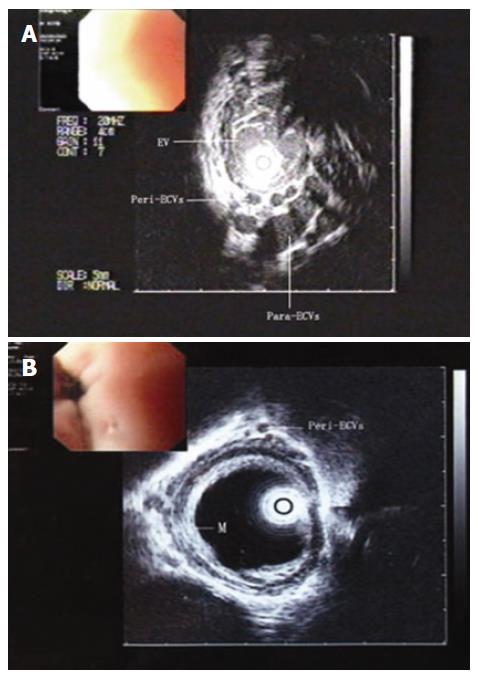
In patients with portal hypertension, collaterals should be established to reduce the high portal pressure, and the hemodynamic indicators of such collaterals have been used for the evaluation of therapeutic effects. According to the location of veins, they can be divided into collateral veins inside and outside of the esophageal wall[1]. The collateral veins inside of the esophageal wall may form varices which can be evaluated by routine endoscopy, and are the major source of recurrent bleeding. The collateral veins outside of the esophageal wall, where hypoechic round spaces can be shown by endoscopic ultrasound (EUS), include peri-esophageal collateral veins (peri-ECVs), para-esophageal collateral veins (para-ECVs) and perforating veins. Peri-ECVs are adjacent to the esophageal wall while para-ECVs are distal to the esophageal wall, the perforating veins penetrate the esophageal wall connecting peri- or para-ECVs[2-5].
Irisawa et al[2-5] demonstrated that both the prevalences of perforating veins and severe peri-ECVs are positively correlated with the form of varices. The incidence of severe peri-ECVs, para-ECVs, and perforating veins in variceal recurrent cases is significantly higher than that in non- variceal recurrent cases (70%, 50% and 90% vs 3.6%, 32.1% and 21.4%, respectively)[6].
On the other hand, endoscopic Doppler ultrasound for measurement of azygos blood flow (AZBF) volume has been used widely in evaluation of the porto-systemic collateral circulation[7], and is a safe and useful method for monitoring portal venous flow in patients with portal hypertension.
It is reported that more than 70% of portal hypert-ension patients with variceal bleeding history may suffer from recurrent bleeding[8,9]. Splenectomy with pericardial devascularization, sclerotherapy, endoscopic variceal ligation (EVL) or other combined therapies have been recommended for those patients. We have previously reported that splenectomy with EVL is superior to splenectomy with pericardial devascularization in the treatment of portal hypertension[10-12]. However, whether combined EVL and splenectomy with pericardial devascularization is effective and the hemodynamic alterations in this process remain unknown.
In this study, we used EUS and color Doppler ultrasound to detect the hemodynamic alterations in collateral circulation before and after EVL in combination with splenectomy with pericardial devascularization. The hemodynamic parameters were used to evaluate its effect. An ultrasound microprobe (UMP) was adopted for the detection of collateral veins, which could provide better images of vascular structures than conventional EUS due to its higher frequency and resolution[3,13,14].
From March 2001 to May 2004, consecutive patients with untreated esophageal varices caused by portal hypertension were admitted to the Third Affiliated Hospital of Sun Yat-Sen University. Patients who did not want to participate in the study, those with severe diseases in major organs other than in liver and/or older than 70 years, and those with different Child-Pugh’s scores before and after all EVL sessions were excluded to avoid the influence of alterations of Child-Pugh’s grade on the portal blood flow rate[5]. Finally, 43 patients who were clinically diagnosed as portal hypertension with endoscopically confirmed esophageal varices were included in this study. The clinical data of the enrolled patients are shown in Table 1.
| Sex | |
| M:F | 28:15 |
| Mean age ± SD (range) (yr) | 50.8 ± 11.2 (20-66) |
| Etiology of liver cirrhosis | |
| Posthepatic | 41 |
| Schistosomiasis | 1 |
| Alcoholic | 1 |
| Liver function, Child-Pugh classification | |
| A | 16 |
| B | 18 |
| C | 9 |
| History of upper gastrointestinal bleeding | 30 |
Written informed consent was obtained from all the patients, and the study was approved by the Ethics Committee of Sun Yat-Sen University.
Patients underwent EVL first. After local application of lidocaine, an endoscope (GIF 240 or 260, Olympus Optical, Tokyo) was introduced, and ligation was carried out 6-12 times by placing a single rubber band (Bard Interventional Products, Tewksbury, Mass.) over a varix. The ligation was repeated every 2 wk till the complete disappearance of varices under endoscope.
Patients underwent splenectomy with pericardial devascularization (Hassab’s operation) 4-10 wk after the first EVL session as previously described by Yang and Qiu[15]. In brief, extended left subcostal incision or L incision of the left upper abdomen was used for extreme splenomegaly. After routine splenectomy, the gastric branch and 5-8 small branches of the gastric coronary veins were disconnected. The esophageal branch was disconnected and suture-ligated. The gastric posterior vein was ligated by suturing, and then the left subphrenic vein was ligated as well[16]. In addition, the arteries accompanying the veins including the left gastric, left gastroepiploic, gastric posterior and left subphrenic arteries, were disconnected.
Color Doppler ultrasound detection was performed before the treatment and 1 wk prior to discharge. AZBF was measured with EUS duplex Doppler technique with a Pentax FG-32UA echo-endoscope (Tokyo, Japan) and a Hitachi EUB-515A ulterasound scanner (Tokyo, Japan) with a frequency of 7.5 MHz[17]. The diameter of the vessel and the blood velocity were measured, the mean value of 3 repeated measures performed at the same position was used. AZBF was calculated with the following formula: AZBF = (radius)2 × blood velocity.
The structure of vessels inside and outside of the esophageal wall was examined before the treatment and 1 wk prior to discharge with an Olympus UM-3R 20MHz UMP (Tokyo, Japan ) passed through the accessory channel of a GIF 250 Olympus endoscope (Tokyo, Japan). Before examination, the esophagus was filled with deaerated water through a water supply tube attached to the endoscope. The veins around the esophagus were scanned from the esophago-gastric junction (GEJ) to a point 5 cm proximal to the EGJ. Varices inside of the esophageal wall (EV) were evaluated as mild (< 5 mm in diameter), moderate (5-7 mm in diameter), and severe (> 7 mm in diameter).
According to the definition of location[3], esophageal collateral veins outside of the esophageal wall could be divided into peri-ECVs and para-ECVs. There were less than 4 mild peri-ECVs (< 2 mm in diameter) and more than 5 severe peri-ECVs (≥ 2 mm in diameter) adjacent to the muscularis externa of the esophagus, a few mild para-ECVs (< 5 mm in diameter) and severe para-ECV (≥ 5 mm in diameter) distal to the esophageal wall without contact with the muscular externa. The presentations of perforating veins penetrating the esophageal wall which were connected either to peri-ECV or to para-ECV, were recorded.
Endoscopic follow-up was performed every 12 wk after discharge of the patients. The degree of varices was evaluated at each follow-up.
Values were expressed as mean ± SD. Statistical analysis was performed using the statistical SPSS version 10.0. Differences in numerical variables between groups were analyzed with paired t test. Mann-Whitney test was used for the analysis of ranked data. Comparison of categorical data was performed by the chi square test. P < 0.05 (two-tailed test) was considered statistically significant.
Compared to pre-treatment, EV, peri- and para-ECV in varices as well as perforating veins were all improved after treatment. Patients with moderate or severe EV or severe peri-ECVs had improvement after treatment, while the percentage of patients with severe para-ECVs decreased from 54.49% to 2.33%, and the percentage of patients with detectable perforating veins decreased from 79.07% to 4.65% (P < 0.01, Table 2).
| Pre-treatment | Post-treatment | |
| n (%) | n (%) | |
| EV | ||
| Mild | 0 (0) | 43 (100) |
| Moderate | 26 (60.47) | 0 (0) |
| Severe | 17 (39.53) | 0 (0) |
| Peri-ECVs | ||
| Mild | 13 (30.23) | 43 (100) |
| Severe | 30 (69.77) | 0 (0) |
| Para-ECVs | ||
| Mild | 20 (46.51) | 42 (97.67) |
| Severe | 23 (53.49) | 1 (2.33) |
| Perforating veins | ||
| Detectable | 34 (79.07) | 2 (4.65) |
| Undetectable | 9 (20.93) | 41 (95.35) |
In the UMP images before treatment, enlarged tortuous varices were found inside of the esophageal wall, while many small vessels adjacent to the muscularis externa formed a venous plexus. After treatment, the anechoic areas inside and outside of the esophageal wall disappeared or remained only tiny, while the echo of mucosa and submucosa of the esophagus enhanced. The alteration in appearance of UMP images intuitively implied the improvement in varices after treatment (Figure 1).
Color Doppler flowmetry showed a significant decrease both in AZBF (43.00%, P < 0.05) and in diameter of the azygos vein (28.85%, P < 0.05), while the blood flow rate was uncharged (Table 3).
A total of 40 patients were followed up for 6 mo to 1 year, with a follow-up rate of 93.0%. Three patients were not followed up due to death (1 died of liver cancer, 2 died of other diseases). The recurrence rate of esophageal varices was 2.5% (1/40, mild), while no re-bleeding cases were recorded.
Although splenectomy with pericardial devascularization has been commonly used for portal hypertension and can control bleeding[15], re-bleeding is likely to occur because of the existing portal hyperdynamic pressure[18]. Varices cannot be eliminated by splenectomy with pericardial devascularization, and the unblocked blood flow in reverse direction in esophageal submucosa and muscular layer may increase the venous pressure at the distal part of stomach, which increases the risk of variceal bleeding.
EVL is a more effective method for portal hypertension with less side effects than surgery[19,20]. However, it causes fibrosis in mucous layer where the esophageal varices locate and has no effect on the formation of collateral circulations in the muscular layer or outside of the esophageal wall.
Nagamine et al[13] showed that after repeated EVL, almost all varices are undetectable in UMP imaging. However, neither collateral nor the azygous vein significantly changes its size. Similar results have been repeated by Seno et al[21].
In our study, not only varices were relieved, but also the sizes of collaterals and azygous vein were reduced after combined EVL and splenectomy with pericardial devascularization, suggesting that this combined therapy can almost completely relieve collateral vein varices both inside and outside of the esophageal wall.
In addition, more obvious improvement in collateral vein varices outside of the esophageal wall was found in peri-ECVs (the percentage of severe cases reduced from 69.77% to 0%) and perforating veins (the percentage of detectable cases reduced from 79.07% to 4.65%), suggesting that peri-ECVs play a more important role in the formation of esophageal varices than para-ECVs[3].
The incidence of varix and its recurrence observed in a short-term follow-up were low. However, the long-term results of the treatment in this study may be influenced by many factors, such as liver function, infection and food consumption. Therefore, the long-term effect of combined EVL and splenectomy with pericardial devascularization should be further studied.
In conclusion, combined EVL and splenectomy with pericardial devascularization can block the collateral veins both inside and outside of the esophageal wall and is more advantagious over splenectomy with pericardial devascularization or EVL in preventing recurrence and rebleeding of varices.
S- Editor Wang GP L- Editor Wang XL E- Editor Ma WH
| 1. | BUTLER H. The veins of the oesophagus. Thorax. 1951;6:276-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 67] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Irisawa A, Saito A, Obara K, Shibukawa G, Takagi T, Yamamoto G, Sakamoto H, Takiguchi F, Shishido H, Hikichi T. Usefulness of endoscopic ultrasonographic analysis of variceal hemodynamics for the treatment of esophageal varices. Fukushima J Med Sci. 2001;47:39-50. [PubMed] |
| 3. | Irisawa A, Obara K, Sato Y, Saito A, Takiguchi F, Shishido H, Sakamoto H, Kasukawa R. EUS analysis of collateral veins inside and outside the esophageal wall in portal hypertension. Gastrointest Endosc. 1999;50:374-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 69] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Irisawa A, Saito A, Obara K, Shibukawa G, Takagi T, Shishido H, Sakamoto H, Sato Y, Kasukawa R. Endoscopic recurrence of esophageal varices is associated with the specific EUS abnormalities: severe periesophageal collateral veins and large perforating veins. Gastrointest Endosc. 2001;53:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Irisawa A, Obara K, Bhutani MS, Saito A, Shishido H, Shibukawa G, Takagi T, Yamamoto G, Seino O, Shishido F. Role of para-esophageal collateral veins in patients with portal hypertension based on the results of endoscopic ultrasonography and liver scintigraphy analysis. J Gastroenterol Hepatol. 2003;18:309-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Obara K. Hemodynamic mechanism of esophageal varices. Zhonghua Xiaohua Neijing Zazhi. 2006;18:6-9. |
| 7. | Lebrec D, Sogni P, Vilgrain V. Evaluation of patients with portal hypertension. Baillieres Clin Gastroenterol. 1997;11:221-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Grace ND, Groszmann RJ, Garcia-Tsao G, Burroughs AK, Pagliaro L, Makuch RW, Bosch J, Stiegmann GV, Henderson JM, de Franchis R. Portal hypertension and variceal bleeding: an AASLD single topic symposium. Hepatology. 1998;28:868-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 259] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Gotoh Y, Iwakiri R, Sakata Y, Koyama T, Noda T, Matsunaga C, Ogata SI, Ishibashi S, Sakata H, Tsunada S. Evaluation of endoscopic variceal ligation in prophylactic therapy for bleeding of oesophageal varices: a prospective, controlled trial compared with endoscopic injection sclerotherapy. J Gastroenterol Hepatol. 1999;14:241-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Liu B, Xu RY, Qiu WS, Lin N, Chen TF, Huang FZ, Liu XY. [Treatment of portal hypertension by endoscopic esophageal ligation of varicose veins combined with partial splenic embolization]. Zhonghua Waike Zazhi. 2003;41:721-723. [PubMed] |
| 11. | Xu RY, Liu B, Lin N. Therapeutic effects of endoscopic variceal ligation combined with partial splenic embolization for portal hypertension. World J Gastroenterol. 2004;10:1072-1074. [PubMed] |
| 12. | Liu B, Lin N, Xu RY. [Splenectomy combined with endoscopic variceal ligation in treating portal hypertension]. Zhongnan Daxue Xuebao Yixueban. 2004;29:87-89. [PubMed] |
| 13. | Nagamine N, Ido K, Ueno N, Kimura K, Kawamata T, Kawada H, Hirasawa T, Suzuki T, Kubo H, Tokumaru K. The usefulness of ultrasonic microprobe imaging for endoscopic variceal ligation. Am J Gastroenterol. 1996;91:523-529. [PubMed] |
| 14. | Nishizono M, Haraguchi Y, Eto T, Kamikawa H, Bekki F, Nagasaki Y, Koga N, Koga T, Yamashita Y. Endoscopic ultrasonography using a 15/20 MHz probe in a direct contact technique: evaluation and application in esophageal and gastric varices. Fukuoka Igaku Zasshi. 1994;85:251-255. [PubMed] |
| 15. | Yang Z, Qiu F. [Pericardial devascularization with splenectomy for the treatment of portal hypertension]. Zhonghua Waike Zazhi. 2000;38:645-648. [PubMed] |
| 16. | Justo CR, Brandt CT, Lucena MT, Jales M. Effect of splenectomy and ligature of the left gastric vein on portal hypertensive colopathy in carriers of surgical hepatosplenic schistosomiasis mansoni. Acta Cir Bras. 2005;20:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Nishida H, Giostra E, Spahr L, Mentha G, Mitamura K, Hadengue A. Validation of color Doppler EUS for azygos blood flow measurement in patients with cirrhosis: application to the acute hemodynamic effects of somatostatin, octreotide, or placebo. Gastrointest Endosc. 2001;54:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Huang Y, Wang W, Wang J, Bai C. Surgical treatment of portal hypertension: 45 year experience. Zhonghua Waike Zazhi. 2000;38:85-88. [PubMed] |
| 19. | Garcia-Pagán JC, Bosch J. Endoscopic band ligation in the treatment of portal hypertension. Nat Clin Pract Gastroenterol Hepatol. 2005;2:526-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 87] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 20. | Biecker E, Schepke M, Sauerbruch T. The role of endoscopy in portal hypertension. Dig Dis. 2005;23:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Seno H, Konishi Y, Wada M, Fukui H, Okazaki K, Chiba T. Endoscopic ultrasonograph evaluation of vascular structures in the gastric cardia predicts esophageal variceal recurrence following endoscopic treatment. J Gastroenterol Hepatol. 2006;21:227-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |