Published online Oct 21, 2006. doi: 10.3748/wjg.v12.i39.6382
Revised: June 28, 2006
Accepted: July 18, 2006
Published online: October 21, 2006
AIM: To explore some operative techniques to prevent the occurrence of delayed gastric emptying (DGE) after pylorus-preserving pancreaticoduodenectomy (PPPD).
METHODS: One hundred and eighty-six patients in a single medical center who accepted PPPD were retrospectively studied. The incidence of DGE was investigated and the influence of some operative techniques on the prevention of DGE was analyzed.
RESULTS: During the operative process of PPPD, the methods of detached drainage of pancreatic fluid and bile and gastric fistulization were used. Postoperatively, six patients suffered DGE among the 186 cases; the incidence was 3.23% (6/186). One of them was complicated with intraabdominal infection at the same time, and two with pancreatic leakage.
CONCLUSION: Appropriate maneuvers during operation are essential to avoid postoperative DGE in PPPD. The occurrence of DGE is avoidable. It should not be used as an argument to advocate hemigastrectomy in PPPD.
- Citation: Bu XM, Xu J, Dai XW, Ma K, Yang FQ, Hu J, Wang NF. Is delayed gastric emptying so terrible after pylorus-preserving pancreaticoduodenectomy? Prevention and management. World J Gastroenterol 2006; 12(39): 6382-6385
- URL: https://www.wjgnet.com/1007-9327/full/v12/i39/6382.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i39.6382
Pylorus-preserving pancreaticoduodenectomy (PPPD) was first reported by Watson in 1944[1] and reintroduced by Traverso and Longmire in 1978[2]. For the sake of functional preservation of the stomach and improvement of life quality, it has been accepted and adopted by more and more surgeons. With the wide use of PPPD, delayed gastric emptying (DGE) becomes the most common complication in the early postoperative course. Although there is no generally accepted definition of DGE, it may be described as the need for gastric suction during postoperative 7-10 d. Despite the self-limited characteristics of DGE, it prolongs the hospitalization days and increases the sufferings of patients. Meanwhile, it also affects the confidence of surgeons in further use of PPPD. In order to reduce the risk of DGE, we have adopted some effective approaches during operative process, as well as some postoperative managements and gained satisfactory results.
From March 1992 to December 2003, 186 consecutive patients from the Department of Hepatobiliary Pancreatic Surgery of our hospital underwent PPPD performed by the same surgical group. Of these patients, 110 were male (59.1%) and 76 were female (40.9%), with a median age of 55.3 years (range, 32 to 83). The most frequent indication was peri-ampullary carcinomas (184 patients) (Table 1).
| Type of disease | Cases (n) | % |
| Ampulla carcinoma | 78 | 41.9 |
| Distal carcinoma of common bile duct | 61 | 32.8 |
| Duodenal carcinoma | 4 | 2.1 |
| Pancreatic head carcinoma | 39 | 21.0 |
| Cyst adenocarcinoma | 2 | 1.1 |
| Chronic pancreatitis | 2 | 1.1 |
Blood supply of duodenal residue should be well preserved: When the hepatogastric ligament and right part of gastrocolic ligament were resected, the vessel arch around the stomach should be preserved. The right gastric artery and gastroduodenal artery were divided and ligated at their origins to keep the distal arcade. The duodenum was transected 2 to 3 cm below the pylorus. The stomach was packed with wet gauze to protect it from loss of fluid. If the blood supply of residual duodenum was poor, PPPDs were substituted by standard pancreaticoduodenectomy (PD).
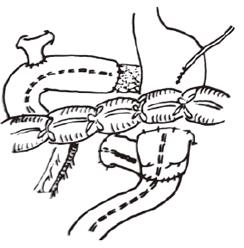
The detached drainage of pancreatic fluid and bile was performed: After the neck of pancreas was transected, a thin drainage tube (about 3 mm in diameter and 40 cm in length) was inserted into the distal pancreatic duct (Figure 1). The tube could drain the pancreatic fluid out of peritoneal cavity before pancreaticojejunostomy. When the posterior wall of pancreaticojejunostomy was completed, the thin tube was put into the jejunum to drain the pancreatic fluid away from the pancreaticojejunostomy and cholangiojejunostomy. Several small steel balls were put into the distal end of the tube, and their gravity may keep the tube from bending in the jejunum. We named the drain method detached drainage of pancreatic fluid and bile. Regarding the alimentary reconstructive procedures, Child’s method was adopted.
Gastric fistulization tube was put into the intestine through the duodejejunal anastomosis: After the posterior wall of duodejejunectomy was sutured, gastric fistulization was made routinely. A small hole was made in the anterior wall of the stomach, and a thin tube (about 40 cm in length and 4 mm in diameter) was inserted through the hole and pylorus to the proximal jejunum. The other end of the tube passed through the abdominal wall and was fixed to the skin. Two abdominal drainage tubes were essential for the operation, one was placed behind the pancreaticojejunostomy and choledochojejunostomy, and the other was placed in front of the pancreaticojejunostomy.
In order to help the patients recover well, relatively stable internal environment and good nutritional condition of the patients should be maintained. In the preoperative and early postoperative stages, correction of imbalance of water and electrolytes and appropriate nutritional support should be undertaken. In most cases, total parenteral nutrition was needed.
The drainage tubes must be carefully watched to keep fluent in postoperative stage, because sometimes blood clots and necrotic tissues may obstruct them. If postoperative abdominal infection was suspected or proved, effective therapies such as drainage of the infectious focus and prescription of antibiotics should be taken promptly. Gastric suction may be stopped within postoperative 2 to 3 d; meanwhile, gastrointestinal motility drugs may be taken orally. After the recovery of alimentary function, the patients may have liquid diet, and the amount of the intravenous fluid may be reduced. The use of antacid drugs was routine.
If the DGE was suspected, some examinations were helpful. The first was X-ray examination of the stomach; 76% of meglucamine diatrizoate was injected into the stomach by gastric suction tube. The typical manifestation of DGE was the decrease or diminish of gastric peristalsis; the contrast media retained in the stomach and could not go into the jejunum. A further choice was gastroscopic examination; the obstruction of gastrojejunostomy might be excluded. To improve the DGE, nutritional support was essential. Because of the thin tube in the stomach and jejunum; enteral nutrition was available and convenient. Small doses of erythromycin (0.6-0.9 g/d) might be administered intravenously. Some other drugs might also be used to stimulate the peristalsis of gastrointestinal tract, such as cisapride. For some patients, the change of body position was helpful, such as lying on the right side.
The complications of PPPD are listed in Table 2. Six patients suffered DGE among the 186 cases; the incidence was 3.23% (6/186). Among them, one was also complicated with intraabdominal infection simultaneously, and two with pancreatic leakage. The median recovery time was 36 (range: 15-81) d. One patient recovered after the gastroscopic examination. Three patients became normal after the use of small doses of erythromycin and cisapride. One patient did not show remission though all of the above methods were tried. However, at the 81st day postoperation, the uncomfortable symptoms of the patient disappeared spontaneously.
| Complication | Cases (n) |
| Delayed gastric emptying | 6 |
| Pancreatic leakage | 4 |
| Intraabdominal infection | 2 |
| Intraabdominal hemorrhage | 2 |
| Liver function failure | 2 |
| Bile leakage | 1 |
As the main complication of PPPD, DGE may occur in 20%-60% of patients[3-8]. The pathogenesis of DGE is still unknown. Thor and his coworkers[9] found that the operation might damage the enteric nervous system, which induced the profound changes in gastric motility and emptying. Some authors[9,10] stressed that the ischemic injury of antrum and pylorus plays an important role in the occurrence of DGE. Others emphasized the central role of the change of motilin concentration in plasma in DGE occurrence. All these above factors may partially participate in occurrence of DGE. In clinics, DGE is characterized with gastric dysfunction. The gastrointestinal radiography indicates the stomach is dilated; the gastric peristalsis is decreased or diminished. By the examination of gastroscopy, we may see the duodenojejunostomy anastomosis and gastric mucosa is congested and edematous, but the anastomosis is unobstructed, and the top end of gastroscopy may go through the anastomosis smoothly.
In our series, gastric fistulization was a routine maneuver. We assumed that the thin tube played an important role in prevention of DGE. In the early postoperative period, even if the existence of gastric atony, the gastric juice and liquid food may flow into jejunum along the wall of the tube, similar to the situation of flow of the bile into the duodenum in the patient with endoscopic nasobiliary drainage. Therefore, the gastric retention can be decreased. The corresponding symptoms such as nausea and vomiting may be avoided. Because the tube had many orifices in the walls at its forepart, if the gastric retention was very serious, negative pressure suction was convenient through the tube. If the abnormal gastric function lasted for a period of time and led to delayed food ingestion, enteral nutrition was available through the jejunal tube, thus avoiding some complications arising from long-term parenteral nutrition.
Besides the above-mentioned factors that may lead to DGE, postoperative intra-abdominal complications are also an important cause. Riediger[11] studied 204 patients undergoing PPPD. By multivariate analysis, it was revealed that the postoperative complications were the most important factor associated with the occurrence of DGE. Park[12] studied 150 consecutive patients who underwent PPPD performed by one surgeon. The incidence of DGE was 41.7% (15 of 36) in the group with complications, yet only 8.8% (10 of 114) in the other group (P = 0.0001). Among the postoperative intraabdominal complications, pancreatic leakage was most often seen. In our series, two of the six patients with DGE were complicated with pancreatic leakage. Therefore, it is important to prevent the pancreatic leakage during postoperative period.
Pancreatic leakage is also a primary complication after PPPD. It is far more disastrous than DGE. It is not only related to delayed gastric emptying, but can lead to some fatal consequences such as intra-abdominal bleeding and infection. How to prevent its occurrence is always a compelling problem for surgeons. In our experience, detached drainage of pancreatic fluid and bile is an effective method[13] for the prevention of pancreatic leakage. The tube in pancreatic duct can drain pancreatic fluid into the jejunum away from the pancresticojejunostomy. No pancreatic fluid detains in the intestinal lumen near the pancreaticojejunostomy, the enteral pressure is decreased and pancreaticojejunostomy is free of the soaking and corrosion resulting from pancreatic fluid. Along the outer wall of the tube, the bile is also drained to the distal jejunum away from cholangiojejunostomy where it mixes with pancreatic fluid and activates the digestive proenzyme in pancreatic fluid. Due to adoption of these methods, the incidence of pancreatic leakage was rather low in our series. We believe that it is helpful for the prevention of the DGE. Compared with the traditional method, in which the pancreatic fluid is drained outside body, our technique may decrease the loss of body fluid, thus helpful for maintaining stable internal environment and balancing the water and electrolytes of the patients.
As a postoperative complication characterized by gastrointestinal dysfunction, DGE is not specific for PPPD. It may occur after other abdominal operations, including the standard pancreaticoduodenectomy. Tran studied[14] a nonselected series of 170 consecutive patients and found DGE occurred equally in the 2 groups. Horstmann[15] also proposed that pylorus preservation did not increase the frequency of DGE. DGE almost exclusively occurs as a consequence of other postoperative complications. As we know, the best way to avoid postoperative complications is appropriate maneuvers during operation. In our series, besides elaborate surgical techniques, we used the thin tube twice, and the small tubes really play big roles in preventing DGE. Since the occurrence of DGE is avoidable in most cases, DGE should not be used as an argument to advocate hemigastrectomy in PPPD.
S- Editor Liu Y L- Editor Zhu LH E- Editor Bai SH
| 1. | Watson K. Carcinoma of ampulla of Vater. Successful radical resection. Br J Surg. 1944;31:368-373. [RCA] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Traverso LW, Longmire WP Jr. Preservation of the pylorus in pancreaticoduodenectomy. Surg Gynecol Obstet. 1978;146:959-962. [PubMed] |
| 3. | Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, Coleman J. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993;217:430-45; discussion 430-45;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 565] [Article Influence: 17.7] [Reference Citation Analysis (33)] |
| 4. | Hishinuma S, Ogata Y, Matsui J, Ozawa I. Complications after pylorus-preserving pancreatoduodenectomy with gastrointestinal reconstruction by the Imanaga method. J Am Coll Surg. 1998;186:10-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992;127:945-99; discussion 945-99;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 274] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 6. | Patel AG, Toyama MT, Kusske AM, Alexander P, Ashley SW, Reber HA. Pylorus-preserving Whipple resection for pancreatic cancer. Is it any better. Arch Surg. 1995;130:838-42; discussion 842-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 84] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Heise JW, Becker H, Borchard F, Röher HD. [Risks of radical treatment in pylorus preserving duodenopancreatectomy in ductal carcinoma]. Chirurg. 1994;65:780-784. [PubMed] |
| 8. | Talamini MA, Moesinger RC, Pitt HA, Sohn TA, Hruban RH, Lillemoe KD, Yeo CJ, Cameron JL. Adenocarcinoma of the ampulla of Vater. A 28-year experience. Ann Surg. 1997;225:590-599; discussion 590-599;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 197] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Braasch JW, Deziel DJ, Rossi RL, Watkins E Jr, Winter PF. Pyloric and gastric preserving pancreatic resection. Experience with 87 patients. Ann Surg. 1986;204:411-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 191] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Liberski SM, Koch KL, Atnip RG, Stern RM. Ischemic gastroparesis: resolution after revascularization. Gastroenterology. 1990;99:252-257. [PubMed] |
| 11. | Riediger H, Makowiec F, Schareck WD, Hopt UT, Adam U. Delayed gastric emptying after pylorus-preserving pancreatoduodenectomy is strongly related to other postoperative complications. J Gastrointest Surg. 2003;7:758-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Park YC, Kim SW, Jang JY, Ahn YJ, Park YH. Factors influencing delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Am Coll Surg. 2003;196:859-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 115] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Dai XW, Ma K, Wang FX, Yang FQ, Wang BS, Zhao HY, Sun W, Liu BL, Qiu F, Pu XM. Prevention of pancreaticojejunal anastomotic leakage after pancreaticoduodenectomy with separate internal drainage of bile and pancreatic fluid. Hepatobiliary Pancreat Dis Int. 2003;2:131-134. [PubMed] |
| 14. | Tran KT, Smeenk HG, van Eijck CH, Kazemier G, Hop WC, Greve JW, Terpstra OT, Zijlstra JA, Klinkert P, Jeekel H. Pylorus preserving pancreaticoduodenectomy versus standard Whipple procedure: a prospective, randomized, multicenter analysis of 170 patients with pancreatic and periampullary tumors. Ann Surg. 2004;240:738-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 286] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 15. | Horstmann O, Markus PM, Ghadimi MB, Becker H. Pylorus preservation has no impact on delayed gastric emptying after pancreatic head resection. Pancreas. 2004;28:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 86] [Article Influence: 4.1] [Reference Citation Analysis (0)] |