Published online Sep 28, 2006. doi: 10.3748/wjg.v12.i36.5913
Revised: July 2, 2006
Accepted: July 7, 2006
Published online: September 28, 2006
We experienced a very rare case of ulcerative colitis (UC) accompanied with analogous lesions in the stomach, duodenum, and ileal J -pouch. Ileal J-pouch anal anastomosis was performed on a 29-year old woman in 1996. Six years later, she was admitted again to our hospital because of epigastralgia, nausea, watery diarrhea and low fever. Based on the results of endoscopic examination, we diagnosed it as pouchitis. Moreover, on hypotonic duodenography, expansion of the duodenal bulb and the descending portion were poor. Kerckring folds disappeared with typical lead-pipe appearance. The pathogenesis of the gastric and duodenal lesion in this patient was similar to that of the colonic lesions of UC. For the gastroduodenal lesions in this patient, symptomatic remission was obtained following administration of crushed mesalazine tablets (1500 mg/d) for 14 d with continuous administration of omeprazole. Firstly we used ciprofloxacin to treat pouchitis. On the fifth day, she got a fever because of catheter infection. In the catheter culture, methicillin-resistant Staphylococcus aureus (MRSA) was detected. Therefore we changed ciprofloxacin to vancomycin hydrochloride (Vancomycin®). Vancomycin was very effective, and the stool frequency dramatically improved in three days. Now she continues to take mesalazine, but her condition is stable and there has been no recurrence of pouchitis.
- Citation: Ikeuchi H, Hori K, Nishigami T, Nakano H, Uchino M, Nakamura M, Kaibe N, Noda M, Yanagi H, Yamamura T. Diffuse gastroduodenitis and pouchitis associated with ulcerative colitis. World J Gastroenterol 2006; 12(36): 5913-5915
- URL: https://www.wjgnet.com/1007-9327/full/v12/i36/5913.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i36.5913
Pouchitis after total colectomy with ileal pouch anal anastomosis can sometimes occur in patients with ulcerative colitis (UC). Despite intensive studies the cause of pouchitis remains unknown, but many contributing factors, such as faecal stasis, bacterial invasion, and faecal bile acids have been postulated. Data on the cumulative risk of pouchitis at 5 to 10 years after ileal J-pouch anal anastomosis (IPAA) in UC patients range from 30% to 50% in Western countries[1]. On the other hand, the cumulative risk of pouchitis in Japanese UC patients is lower than that in Western countries[2]. Gastroduodenal lesions in patients with UC are apparently rare, the stomach and duodenum are not generally considered as target organs in UC and there is no consensus regarding their significance or management. When we review the previous case reports, if anything, the number of reported cases of gastroduodenal lesions associated with UC is increasing in Japan. At this time, we experienced a very rare case of UC accompanied with analogous lesions in the stomach, duodenum, and ileal J-pouch. These findings suggest that UC is a generalized disease in which gastroduodenal changes can be regarded as one facet.
A 29-year old woman with a 3-year history of left-side colitis was referred to our hospital for 2 stage total proctocolectomy with mucosectomy, ileal J-pouch anal anastomosis in 1996. The diagnosis of UC was made on the basis of a barium enema and colonoscopic findings and confirmed by the typical histologic features of colorectal biopsies. No evidence of Crohn’s disease (CD) was present at the time of surgery, and the gross and microscopic features of the colectomy specimen were those of UC. The postoperative course was uneventful, and oral prednisolone was gradually tapered off and completely stopped 2 mo after ileostomy closure. In December 2002, this patient was admitted again to our hospital because of epigastralgia, nausea, watery diarrhea and low fever. On admission, the body temperature was 37.2°C and laboratory data were as follows: red blood cell count 467 × 104/μL, hemoglobin 12.3 g/dL, white blood cell count 6000/μL. C-reactive protein (CRP) was slightly increased at 1.3 mg/dL.
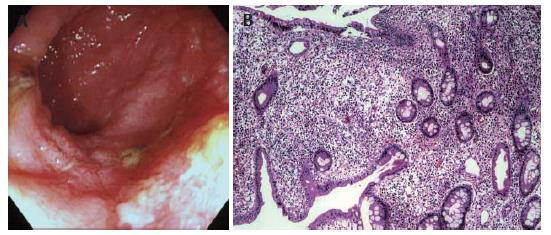
At first we doubted it was pouchitis and performed endoscopy in the ileal J-pouch. The endoscopic features were edema, granularity, loss of vascular pattern, mucus exudates and ulcerations (Figure 1A). Histological examination of the ileal J-pouch biopsied in the active stage demonstrated severe infiltration of inflammatory cells in mucosa (Figure 1B). We used the pouchitis disease activity index (PDAI) as the diagnostic criteria. Her PDAI score was 12 points. We diagnosed her with pouchitis.
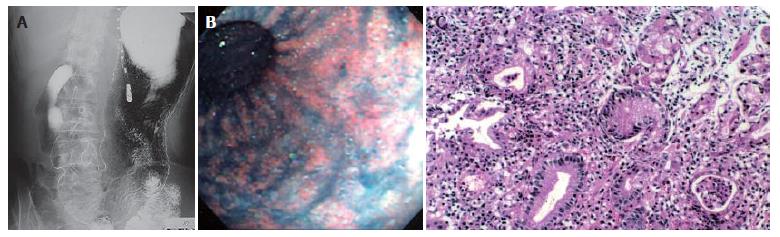
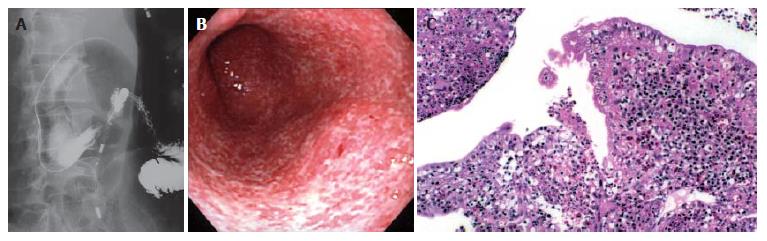
Endoscopy of the upper gastrointestinal tract disclosed multiple erosions and granular changes in the antral greater curvature of the stomach and similar features were noted in the duodenal bulb and the descending portion of the duodenum (Figures 2B and 3B). On hypotonic duodenography, expansion of the duodenal bulb and the descending portion were poor. Kerckring folds disappeared with a typical lead-pipe appearance (Figure 3A). The expansion of the gastric wall was kept but antral mucosa disclosed multiple granular changes (Figure 2A). Histological examination of the stomach biopsied in the active stage demonstrated severe infiltration of inflammatory cells in mucosa and crypt abscess in the mucous glandules (Figure 2C). Histology of the biopsy specimens revealed dense acute and chronic inflammatory infiltrates accompanied with cryptitis in the duodenum (Figure 3C). Neither granuloma nor H pylori was detected in biopsied sections.
After admission, we performed intravenous hyperalimentation, because she exhibited dehydration due to severe watery diarrhea. The gastroduodenal lesions in this patient were not improved by oral omeprazole (20 mg/d) for 7 d, but symptomatic remission was obtained following administration of crushed mesalazine tablets (1 500 mg/d) for 14 d, with continuous administration of omeprazole. Firstly we used ciprofloxacin to treat pouchitis. On the fifth day, she got a fever because of catheter infection. Methicillin-resistant Staphylococcus aureus (MRSA) was detected in the catheter culture. Therefore we changed ciprofloxacin to vancomycin hydrochloride (Vancomycin®). Vancomycin was very effective, and the stool frequency dramatically improved in three days. The patient was discharged on the 44th hospital day. Now she continues to take mesalazine, but her condition is stable and there is no recurrence of pouchitis.
Pouchitis is an idiopathic inflammatory disease of the ileal reservoir in patients who have undergone ileal J-pouch anal anastomosis (IPAA), and is the most common long-term complication of IPAA in UC. The cumulative risk of developing pouchitis in Japanese UC patients is lower than that of western countries[1,2]. On the other hand, reports of gastroduodenal lesions associated with UC are extremely rare in Western countries. In our search we found only 6 cases. Thompson and Bargen[3] reported two cases in 1960 and Valdez et al[4] reported four cases in 2000. In Japan, recently, the number of reports of gastroduodenal lesions associated with UC is increasing. In 2002, Warita et al[5] reported 15 cases in Japan. The instance of both pouchitis and gastroduodenal lesion associated UC exists in only three cases. These cases were reported by Valdez et al[4] in 2000. No patient with complicated pouchitis and gastroduodenal lesion has been reported in Japan.
Crohn’s disease can affect the whole gastrointestinal tract. On the other hand, UC is a chronic inflammatory disease of the colon and includes various extracolonic manifestations. However, the stomach and duodenum are not generally considered target organs in UC. So in this patient, differential diagnosis from CD was important. In our patient, no evidence of CD was present at the time of surgery, and the gross and microscopic features of the colectomy specimen were those of ulcerative left-side colitis. Diffuse ulcerative duodenitis similar in appearance to the ulcerative colitis was found extending from the second to the third portion of the duodenum. Moreover, the pathogenesis of the gastric and duodenal lesions in this patient was similar to that of the colonic lesions of UC and these findings were not induced by H pylori infection. H pylori was negative in our patient, which is consistent with the finding of Warita et al[5] reported who reported that five of 15 cases are negative for H pylori infection. Recent preliminary reports have described a reduced prevalence of H pylori infection in patients with inflammatory bowel disease compared with the general population. Parente et al[6] reported that previous exposure to sulphasalazine is associated with a significantly lower risk of infection, mainly in Crohn’s disease but also in UC patients.
Medical treatment with mesilazine was very effective in our patient. Mitomi et al[7] reported that the symptoms of their patient are resolved one month after treatment with sulfasarazopyrin (3.0 mg/d) and some antacids. Myojo et al[8] reported that while the duodenitis does not respond to a proton-pump inhibitor, it improves obviously after treatment with mesalazine. Moreover, Sasaki et al[9] reported that gastroduodenal lesions are not improved after oral omeprazole, but healing is obtained following intensive intravenous prednisolone therapy for 14 d with continuous administration of omeprazole. Although there is no consensus regarding these types of management, sulfasarazopyrin or mesalazine should be considered as fast-line therapies for gastroduodenal lesions. If these treatment modalities are ineffective, we should use steroids as the second-line therapy for gastroduodenal lesions.
Terashima et al[10] reported that duodenal lesion accompanying UC may be a more common phenomenon, although it occurs infrequently during steroid therapy. In the future, patients with complicated gastroduodenal lesions in a postoperative steroid-free condition may increase. We have to recognize that UC is a generalized disease in which gastroduodenal changes can be regarded as one facet.
S- Editor Liu Y L- Editor Wang XL E- Editor Bi L
| 1. | Heuschen UA, Allemeyer EH, Hinz U, Autschbach F, Uehlein T, Herfarth C, Heuschen G. Diagnosing pouchitis: comparative validation of two scoring systems in routine follow-up. Dis Colon Rectum. 2002;45:776-786; discussion 786-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Ikeuchi H, Nakano H, Uchino M, Nakamura M, Yanagi H, Noda M, Yamamura T. Incidence and therapeutic outcome of pouchitis for ulcerative colitis in Japanese patients. Dig Surg. 2004;21:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | THOMPSON JW, BARGEN JA. Ulcerative duodenitis and chronic ulcerative colitis: report of two cases. Gastroenterology. 1960;38:452-455. [PubMed] |
| 4. | Valdez R, Appelman HD, Bronner MP, Greenson JK. Diffuse duodenitis associated with ulcerative colitis. Am J Surg Pathol. 2000;24:1407-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Warita E, Hiwatashi N, Kumagai Y, Morimoto T, Yamashita K, Shiraki M, Kiuchi Y, Masuda T, Kayama K, Funayama Y. Diffuse duodenitis associated with ulcerative colitis. Stomach and Intestine. 2002;37:781-789. |
| 6. | Parente F, Molteni P, Bollani S, Maconi G, Vago L, Duca PG, Rembacken B, Axon AT, Bianchi Porro G. Prevalence of Helicobacter pylori infection and related upper gastrointestinal lesions in patients with inflammatory bowel diseases. A cross-sectional study with matching. Scand J Gastroenterol. 1997;32:1140-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Mitomi H, Atari E, Uesugi H, Nishiyama Y, Igarashi M, Arai N, Ihara A, Okayasu I. Distinctive diffuse duodenitis associated with ulcerative colitis. Dig Dis Sci. 1997;42:684-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Myojo T. Hirakawa K, Hirota S, Jo Y, Nakamura M, Nubu R, Iwai K, Yao T, Matsumoto S. Progressive duodenitis in a colectomized patient with ulcerative colitis. Stomach and Intestine. 2001;36:567-573. |
| 9. | Sasaki M, Okada K, Koyama S, Yoshioka U, Inoue H, Fujiyama Y, Bamba T. Ulcerative colitis complicated by gastroduodenal lesions. J Gastroenterol. 1996;31:585-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Terashima S, Hoshino Y, Kanzaki N, Kogure M, Gotoh M. Ulcerative duodenitis accompanying ulcerative colitis. J Clin Gastroenterol. 2001;32:172-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.6] [Reference Citation Analysis (0)] |