Published online Sep 14, 2006. doi: 10.3748/wjg.v12.i34.5562
Revised: May 28, 2006
Accepted: June 14, 2006
Published online: September 14, 2006
Arteroportal fistula is a rare cause of prehepatic portal hypertension. A 44-year-old male with hepatitis virus C infection was admitted for acute variceal bleeding. Endoscopy showed the presence of large esophageal varices. The ultrasound revealed a mass near the head of pancreas, which was characterized at the color-Doppler by a turbulent flow, and arterialization of portal vein flow. CT scan of abdomen showed a large aneurysm of the gastroduodenal artery communicating into the superior mesenteric vein. The sinusoidal portal pressure measured as hepatic vein pressure gradient was normal, confirming the pre-hepatic origin of portal hypertension. The diagnosis of extrahepatic portal hypertension secondary to arteroportal fistula was established, and the percutaneous embolization was performed. Three months later, the endoscopy showed absence of esophageal varices and ascites. At the moment, the patient is in good clinical condition, without signs of portal hypertension.
- Citation: Marrone G, Caruso S, Miraglia R, Tarantino I, Volpes R, Luca A. Percutaneous transarterial embolization of extrahepatic arteroportal fistula. World J Gastroenterol 2006; 12(34): 5562-5564
- URL: https://www.wjgnet.com/1007-9327/full/v12/i34/5562.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i34.5562
Extrahepatic arteroportal fistula is a rare disorder of hepatic vasculature characterized by anomalous communication between arteries and portal vein system most commonly caused by abdominal trauma, and iatrogenic damage induced by procedures such as liver biopsies, tumors and congenital vascular malformations[1]. Arteroportal fistula may cause severe portal hypertension which leads to gastroesophageal variceal bleeding, refractory ascites, diarrhea, and hepatic encephalopathy. The recent progress in computed tomography and magnetic resonance technology with no invasive angiography imaging , makes it possible to confirm the suspicious arteroportal fistula at the Doppler ultrasonography and guide the choice of the treatment. The hepatic vein portal pressure gradient (HVPG) measurement may verify the diagnosis of extrahepatic portal hypertension.
A 44-year-old male was admitted to our Institution because of acute variceal bleeding and a clinical diagnosis of cirrhosis. The patient underwent a total gastrectomy in 1984 for gastroduodenal ulcer. In December 2000, there was a biopsy-proven chronic active hepatitis secondary to hepatitis virus C infection; and a long-term biochemical and virological response was obtained with a 12-mo course of combined antiviral treatment with PEG-IFN plus Ribavirine. Upon admission, the liver function tests were made and the results were: AST 34 U/L, ALT 61 U/L, INR 1.2, PT 63%, serum albumin 33 g/L, serum bilirubin 1.1 mg/dL, and platelets count 15 × 10³ μL.
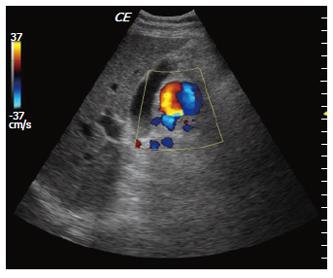
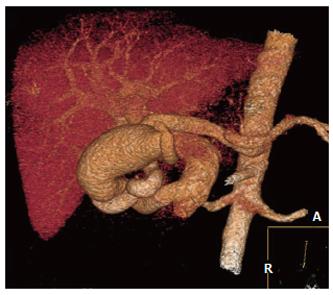
The endoscopy showed the presence of large esophageal varices with cherry red spots, localized in the medial and lower third of the esophagus and extended into the subcardial tract; the varix actively bleeding was treated with banding legations. Two days later, the ultrasonography showed homogeneous liver texture, enlarged spleen (a longitudinal diameter of 16.3 cm) and absence of ascites. However, an anechoic mass 2.5 cm in diameter was detected next to the head of the pancreas. The color-Doppler demonstrated turbulent flow, and arterialization of portal vein flow, with an increased peak velocity (83 cm/sec) (Figure 1). All these findings were suggestive for extrahepatic arteroportal fistula. A 16 slices-MDCT scan of the abdomen was performed, using 150 mL of isosmolate iodate contrast media (1.8 mL/kg), injection-velocity of 5 mL/sec, pitch 1, thickness of 2.5 mm, interval reconstruction of 0.6 mm, and triple-phase acquisition. Maximum Intensity Projection (MIP) and Volume Rendering (VR) 3D angiography reconstructions clearly confirmed the presence of a large aneurysm filled by a dilated gastroduodenal artery, draining into the superior mesenteric vein (Figure 2). Other CT findings were normal liver, presence of esophageal varices and splenomegaly (volume of 910 mL). The HVPG was normal (5 mmHg), confirming the extrahepatic origin of portal hypertension. The diagnosis of extrahepatic portal hypertension secondary to arteroportal fistula was established. However, the patient refused the percutaneous arterial embolization of the fistula.
Seven months later a clinical examination revealed the presence of ascites. The MRI confirmed the presence of free fluid into the abdomen, bilateral pleural effusion and no changes in the aneurysm. The percutaneous embolization was then accepted. The initial angiogram of the celiac axis confirmed the large aneurysm of the gastro-duodenal artery and a fistulous communication with the main portal vein (Figure 3). After selective catheterization of the aneurysm, several metallic coils (8 mm in diameter) were placed in both the aneurysm and the fistula. The post-procedure arteriogram showed the complete occlusion of the fistula (Figure 4).
One month later, the endoscopy demonstrated the absence of esophageal varices. Three months later, a CT scan showed a complete thrombosis of the arteroportal fistula, the absence of ascites and pleural effusion, and a significant reduction of the spleen volume (689 mL). Now, the patient is free of symptoms with normal liver function tests: AST 34 U/L, ALT 32 U/L, serum bilirubin 0.8 mg/dL, albumin 3.9 g/dL, PT 98%, INR 0.8, and platelets count 22 × 10³ μL.
The arteroportal fistula is a rare disorder of hepatic vasculature characterized by anomalous communication between the arteries and portal venous system. Extrahepatic arteroportal fistulas are less common than the intrahepatic ones. The most common causes of arteroportal venous fistula are traumas, iatrogenic damage and congenital vascular malformations[1]. In our patient there was no history of traumas or other vascular malformations, suggesting that the previous gastrectomy might be the most likely cause of arterioportal fistula. It is known that this vascular disorder may cause portal hypertension in non-cirrhotic liver[2,3], due to an increased arterial blood flow. In addition, the nodular regenerative hyperplasia and hepatoportal sclerosis with fibrosis may develop during the follow-up period and worsen portal hypertension[3].
In our case, the arteroportal venous fistula was well detected by Doppler ultrasonography, and confirmed by computed tomography and magnetic resonance angiography.
Severe portal hypertension with large esophageal varices, ascites and pleural effusion was maintained by the increased portal venous inflow. This is confirmed by a normal value of HVPG that rules out the hepatic origin of portal hypertension. The arteroportal venous fistula can be treated with percutaneous arterial occlusion[4]. Notably, esophageal varices and ascites disappeared after the embolization, which further confirmed the role of increased portal blood inflow.
In conclusion, arteroportal fistula is a rare cause of portal hypertension in non-cirrhotic liver and may cause variceal bleeding and ascites. Imaging studies are useful to detect it and the HVPG measurement is useful in confirming the extrahepatic origin of portal hypertension. The percutaneous arterial embolization is an effective therapy for these patients.
S- Editor Wang J L- Editor Ma JY E- Editor Bai SH
| 1. | Tomczak R, Helmberger T, Görich J, Schütz A, Merkle E, Brambs HJ, Rieber A. [Abdominal arteriovenous and arterio-portal fistulas: etiology, diagnosis, therapeutic possibilities]. Z Gastroenterol. 1997;35:555-562. [PubMed] |
| 2. | Kang TC, Lee HC, Yang FS, Wang NL. Idiopathic hepatic arterio-portal fistula: report of one case. Acta Paediatr Taiwan. 2002;43:102-105. [PubMed] |
| 3. | Aithal GP, Alabdi BJ, Rose JD, James OF, Hudson M. Portal hypertension secondary to arterio-portal fistulae: two unusual cases. Liver. 1999;19:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Baumann UA, Tillmann U, Frei J, Fehr HF. [Arterial aneurysm of the liver with arterio-portal fistula: treatment using embolization]. Schweiz Med Wochenschr. 1984;114:451-453. [PubMed] |