Published online Sep 7, 2006. doi: 10.3748/wjg.v12.i33.5401
Revised: May 8, 2006
Accepted: May 22, 2006
Published online: September 7, 2006
Stump appendicitis is an acute inflammation of the residual appendix and one of the rare complications after appendectomy. Paying attention to the possibility of stump appendicitis in patients with right lower abdominal pain after appendectomy can prevent the delay of diagnosis and treatment. In patients with stump appendicitis, CT scan not only assists in making an accurate preoperative diagnosis but also excludes other etiologies. We report a 47-year old man with preoperatively diagnosed stump appendicitis by CT, who underwent an open appendectomy 20 years ago.
- Citation: Uludag M, Isgor A, Basak M. Stump appendicitis is a rare delayed complication of appendectomy: A case report. World J Gastroenterol 2006; 12(33): 5401-5403
- URL: https://www.wjgnet.com/1007-9327/full/v12/i33/5401.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i33.5401
Stump appendicitis is an acute inflammation of the residual appendix and a rare complication after appendectomy[1]. Although the signs and symptoms do not differ from those of acute appendicitis, the diagnosis is often not considered because of prior appendectomy[2]. A small number of stump appendicitis cases have been reported[3]. We report a 47-year old man with preoperatively diagnosed stump appendicitis by CT, who underwent an open appendectomy 20 years ago.
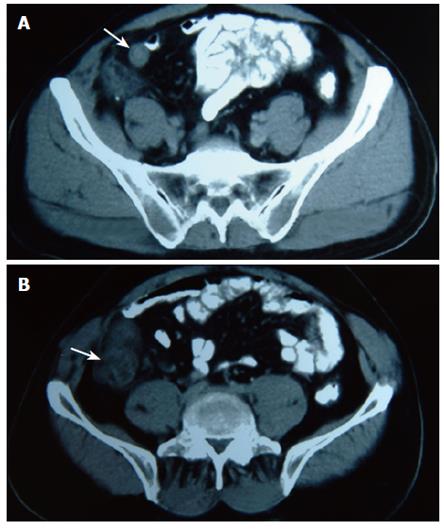
A 47-year-old male patient presented to the emergency department with a chief complaint of abdominal pain for 6 d. The pain was initially localized around the umbilicus, and subsequently localized at the right lower quadrant. The patient complained of anorexia and nausea after the pain started. He had four or five episodes of watery diarrhea daily for 3 d though he had no vomiting. His surgical history included an appendectomy 20 years ago and surgery for peptic ulcer disease 15 years ago. His axillary temperature was 37.1°C, rectal temperature 38.4°C, blood pressure 125/70 mmHg, pulse rate 76 beats/min, and respiratory rate 16 breaths/min. Physical examination of the abdomen revealed healed midline and right lower abdominal (McBurney insicion) surgical scars. A mass without clear borders was found showing tenderness, muscular guarding and rebound in the right lower quadrant during abdominal palpation. Routine laboratory tests included normal electrolyte and blood cell panels except for a white blood cell count of 11700/μL. Urinalysis was unremarkable. Abdominal ultrasonography (USG) showed a heterogene hipoechoic mass at the right lower quadrant. There was no abdominal free fluid. No spesific diagnosis could be made. CT scan of the abdomen and pelvis showed a tubular structure extending from the cecum, with an enhanced wall consistent with an inflamed appendical stump (Figure 1A). Thickened cecum wall, inflammatory change of mesenteric fat and enlarged lymph nodes could also be seen (Figure 1B). Preoperative diagnosis of stump appendicitis was made on the basis of the CT findings.
Abdomen was opened with McBurney incision. Plastron formation in omentum and intestine at the right quadrant and inflammation at the cecum wall were seen. This site was dissected and the purulent material was drained. Stump appendicitis perforated from the appendix radix of 2 cm with necrosis was detected. Appendectomy was performed. The material with necrosis was removed and washed. A drain was placed and the abdomen was closed. Operative findings were confirmed by pathology. The patient was discharged from the hospital three days after operation.
Stump appendicitis is one of the rare delayed compli-cations of appendectomy [4]. Twenty-nine cases have been reported in the worldwide medical literature since the first case reported by Rose in 1945[5,6]. We have detected 7 new cases with our present case, thus 36 cases are available in the worldwide medical literature[2,3,6-10].
The true incidence and prevalence of stump appendicitis are not known, but it is thought to be an underreported entity in the literature[6]. The age of patients with stump appendicitis ranges from 11 to 72 years. The time intervals from initial appendectomy to stump appendicitis range from 2 mo to 51 years[1,3]. A long appendiceal stump is reported to be a risk factor for stump appendicitis. The length of the stump ranges from 0.5 to 6.5 cm[1,3,11,12]. Mangi and Berger[12] reported that leaving an appendiceal stump less than 3 mm in depth with accurate visualisation of the appendiceal base, can minimise the incidence of stump appendicitis.
Whether simple ligation of the appendix or stump inversion into the cecum can reduce the risk of stump appendicitis remains controversial[12]. Rao et al[13] showed that all the cases reported in the literature undergo simple ligation of the appendix without invagination of the stump, suggesting that simple ligation with failure to amputate the appendix close to its origin from the cecum is a prerequisite for developing stump appendicitis. Mangi and Berger[12] reviewed 2185 cases of appendectomy and found that there is no correlation between simple ligation and stump appendicitis. To leave the stump long may cause the inversion difficult. Therefore the length of stump may warn the surgeon.
Laparoscopic appendectomy is now a widely accepted surgical technique in treating appendicitis. The growing use of laparoscopic appendectomy may increase the frequency of stump appendicitis[3,9,11,14] due to the potential limitations of the technique such as smaller field of vision, lack of three-dimensional perspective, absence of tactile feedback, thus leaving a longer stump[14]. In the reported 36 cases of stump appendicitis, only 10 had stump appendicitis after laparoscopic appendectomy[15]. To date, no relationship between laparoscopic appendectomy and stump appendicitis has been demonstrated[12].
A wide spectrum of diseases in the differential diagnosis of right lower quadrant pain of the abdomen and a past appendectomy history delay the diagnosis and treatment of stump appendicitis. It is usually diagnosed perioperatively when stump perforation and/or abscess occurs. In our case, the delay was due to the patient’s late entry to the hospital.
Preoperative screening techniques may help to diagnose the disease[2-4,13,16]. Only 1 case diagnosed by preoperative USG is available in the literature[16]. In our case, although a pathologic lesion was detected at the right lower quadrant by USG, no specific finding of stump appendicitis was detected. Preoperative CT is a more efficient technique. To our knowledge, 4 cases have been diagnosed by CT having stump appendicitis apart from our case to date[2-4,13]. In these studies, beside the appearence of inflamed appendix stump adjacent to the cecum, a cecal arrowhead sign indicating inflammation at the base of the appendix and appendicolith can be seen. CT findings may not be specific for stump appendicits. Nonspecific inflammatory findings such as pericecal inflammatory changes, cecal wall thickening, abscess formation and fluid in the right paracolic gutter can be found in cases of stump appendicitis[2-4,13].
In patients presenting with acute right lower quadrant findings mimicking appendicitis, the history of prior appendectomy does not absolutely rule out the possibility of appendicitis. But this situation usually causes an important delay of their diagnosis and treatment. In patients with stump appendicitis, CT scan not only assists in making an accurate preoperative diagnosis but also excludes other etiologies. Awareness of the possibility of stump appendicitis combined with a high index of suspicion can help to make an early diagnosis.
S- Editor Wang J L- Editor Wang XL E- Editor Ma WH
| 1. | Gupta R, Gernshiemer J, Golden J, Narra N, Haydock T. Abdominal pain secondary to stump appendicitis in a child. J Emerg Med. 2000;18:431-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Aschkenasy MT, Rybicki FJ. Acute appendicitis of the appendiceal stump. J Emerg Med. 2005;28:41-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Shin LK, Halpern D, Weston SR, Meiner EM, Katz DS. Prospective CT diagnosis of stump appendicitis. AJR Am J Roentgenol. 2005;184:S62-S64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Thomas SE, Denning DA, Cummings MH. Delayed pathology of the appendiceal stump: a case report of stump appendicitis and review. Am Surg. 1994;60:842-844. [PubMed] |
| 5. | Rose TF. Recurrent appendiceal abscess. Med J Aust. 1945;32:652-659. |
| 6. | Watkins BP, Kothari SN, Landercasper J. Stump appendicitis: case report and review. Surg Laparosc Endosc Percutan Tech. 2004;14:167-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | De U, De Krishna K. Stump appendicitis. J Indian Med Assoc. 2004;102:329. [PubMed] |
| 8. | Roche-Nagle G, Gallagher C, Kilgallen C, Caldwell M. Stump appendicitis: a rare but important entity. Surgeon. 2005;3:53-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 9. | Nielsen-Breining M, Nordentoft T. [Stump appendicitis after laparoscopic appendectomy]. Ugeskr Laeger. 2005;167:2067-2068. [PubMed] |
| 10. | Burt BM, Javid PJ, Ferzoco SJ. Stump appendicitis in a patient with prior appendectomy. Dig Dis Sci. 2005;50:2163-2164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Erzurum VZ, Kasirajan K, Hashmi M. Stump appendicitis: a case report. J Laparoendosc Adv Surg Tech A. 1997;7:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Rao PM, Sagarin MJ, McCabe CJ. Stump appendicitis diagnosed preoperatively by computed tomography. Am J Emerg Med. 1998;16:309-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Walsh DC, Roediger WE. Stump appendicitis--a potential problem after laparoscopic appendicectomy. Surg Laparosc Endosc. 1997;7:357-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Durgun AV, Baca B, Ersoy Y, Kapan M. Stump appendicitis and generalized peritonitis due to incomplete appendectomy. Tech Coloproctol. 2003;7:102-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Baldisserotto M, Cavazzola S, Cavazzola LT, Lopes MH, Mottin CC. Acute edematous stump appendicitis diagnosed preoperatively on sonography. AJR Am J Roentgenol. 2000;175:503-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |