Published online Aug 21, 2006. doi: 10.3748/wjg.v12.i31.5084
Revised: June 10, 2006
Accepted: June 15, 2006
Published online: August 21, 2006
Cytomegalovirus enteritis is most usually associated with patients positive for human immunodeficiency virus or immunosuppressed transplant patients. The gastrointestinal tract may be affected anywhere from the esophagus to the colon, but the small bowel involvement is rare. We report a case of cytomegalovirus ileitis in an immunocompetent adult, which was confirmed by histopathologic findings through colonoscopic biopsy.
- Citation: Ryu KH, Yi SY. Cytomegalovirus ileitis in an immunocompetent elderly adult. World J Gastroenterol 2006; 12(31): 5084-5086
- URL: https://www.wjgnet.com/1007-9327/full/v12/i31/5084.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i31.5084
Cytomegalovirus (CMV) is a β-group herpes virus and produces latent infection like other herpes viruses. Clinically significant CMV infection usually occurs in patients with immunosuppression, transplantations and acquired immune deficiency syndrome[1]. In immunocompetent subjects, active infection is apparently rare, and the virus exhibits relatively low pathogenicity[2]. We here describe a case of CMV ileitis without colon involvement in an immunocompetent subject.
A 63-year-old woman, with a one-day history of epigastric pain, was hospitalized at Ewha Womans University Hospital on Feb 16, 2006. She is a non-smoker and denied any medication or drug abuse.
On physical examination, the patient appeared to be acutely ill, with a blood pressure of 130/80 mmHg, heart rate of 70 beats/min, respiratory rate of 20 breaths/min, and temperature of 37°C. The abdominal examination was notable for the presence of pain on the epigastric and the right lower quadrant areas with mild guarding but bowel sounds were normal. Laboratory values on admission were in normal range except elevated C-reactive protein.
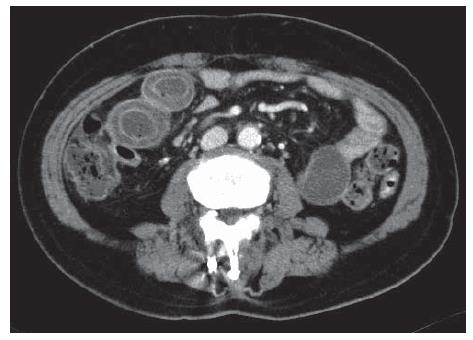
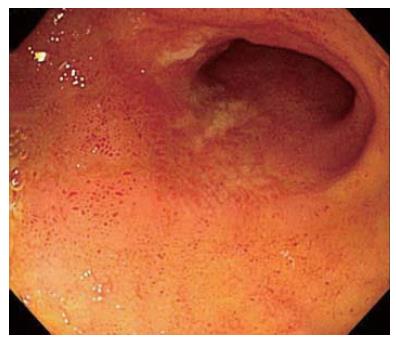
The chest X-ray was normal. Abdominal computed tomography showed layering appearance of bowel wall and luminal dilatation from the distal jejunum to the pelvic ileal loop (Figure 1). The colonoscopy revealed scattered regions of geographic deep ulcerations and hyperemic edematous mucosa upon a background of normal mucosa in terminal ileum (Figure 2). We made differential diagnosis including nonspecific ileitis, Crohn’s disease, tuberculosis induced ileitis and ischemic ileitis. Histological examination showed mild inflammation with lymphocytic infiltration without specific feature.
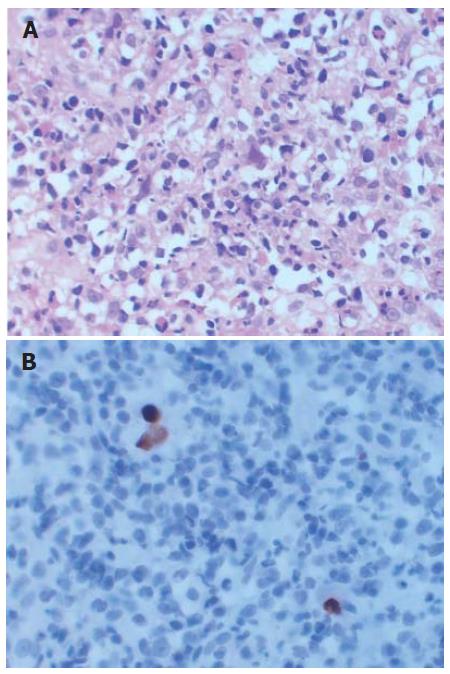
After the initial clinical and laboratory evaluation, the patient began therapy with intravenous antibiotics and fluids for the most probable diagnosis of nonspecific ileitis. During the admission, her clinical condition improved, and abdominal pain disappeared. Two weeks later, the follow up colonoscopy was performed. The ulcerations and hyperemic edematous lesions, which were previously noted on the terminal ileum, were much improved (Figure 3). The histological findings showed intranuclear and intracytoplasmic inclusions. Immunohistochemical stain for CMV showed scattered positive cells at the ulcer base (Figure 4). She was discharged without medication on March 7, 2006.
CMV is a member of the herpes virus family and is a prevalent pathogen, with 40 to 90 percent of the general population showing prior exposure by serology[3]. Human CMV infection can be seen at all stages of life but most often affects those who are immunosuppressed and can commonly cause retinitis, pneumonitis or enteritis[4]. Most primary CMV infections in immunologically healthy adults do not cause symptoms or are associated with a mild mononucleosis like syndrome[5].
Gastrointestinal involvement in CMV infection is well known among immunocompromised patients. It is usually seen in advanced acquired immune deficiency syndrome with CD4 lymphocyte count less than 50 cells/mm3 and among transplant recipients as a reactivation of latent infection or rarely during primary infection[6]. CMV colitis in immunocompetent individuals has been reported mainly in older patients, particularly those with other comorbidities, and is mostly community-acquired. This is likely a reflection of a weakened immune system, as a consequence of aging. Age-related dysfunctions of B and T cell lymphocytes, impaired cytokine, and perturbation of mucosal immunity are thought to contribute to a relative immunodeficiency in the elderly, predisposing them to various infectious and inflammatory diseases[7].
Gastrointestinal tract may be affected anywhere from the mouth to the anus with the esophagus and colon being most common and small bowel relatively rare. The clinical manifestations of gastrointestinal CMV infection include gastrointestinal bleeding, abdominal pain, vomiting and diarrhea[1,8]. Endoscopic findings of gastrointestinal CMV disease include erosions, ulceration and mucosal hemorrhage. The prototypical ulceration has a well-defined punched out appearance. The pathogenesis of CMV-induced ulceration is thought to involve ischemic mucosal injury secondary to infection of the vascular endothelial cells[8,9].
CMV enteritis is remarkable for its ability to mimic many diseases, such as colitis caused by C. diffile, ischemia, malignant diseases of the colon and inflammatory bowel diseases. The diagnosis is made by the demonstration of the presence of CMV by routine histologic examination, culture or staining for CMV antigen or DNA[10,11].
The primary therapy for clinically significant CMV infection is use of the antiviral drugs such as ganciclovir and foscarnet[6,12]. Galiastsatos et al[7] reported that spontaneous resolution occurred mainly in patients younger than 55 years of age, with no other comorbidities. They suggested that young, otherwise healthy, well-selected patients can improve without the need for antiviral therapy but immunocompromised patients and patients older than 55 years of age with comorbidities need antiviral therapy. Sakamoto et al[13] thought that the administration of the antiviral agents is not always necessary for immunocompetent individuals.
In conclusion, we report a case of CMV ilieitis not involving colon in an immunocompetent elderly adult who recovered without antiviral therapy.
S- Editor Wang J L- Editor Zhu LH E- Editor Bi L
| 1. | Cheung AN, Ng IO. Cytomegalovirus infection of the gastrointestinal tract in non-AIDS patients. Am J Gastroenterol. 1993;88:1882-1886. [PubMed] |
| 2. | Oku T, Maeda M, Waga E, Wada Y, Nagamachi Y, Fujita M, Suzuki Y, Nagashima K, Niitsu Y. Cytomegalovirus cholangitis and pancreatitis in an immunocompetent patient. J Gastroenterol. 2005;40:987-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Emery VC. Cytomegalovirus and the aging population. Drugs Aging. 2001;18:927-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Page MJ, Dreese JC, Poritz LS, Koltun WA. Cytomegalovirus enteritis: a highly lethal condition requiring early detection and intervention. Dis Colon Rectum. 1998;41:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Taylor GH. Cytomegalovirus. Am Fam Physician. 2003;67:519-524. [PubMed] |
| 6. | Klauber E, Briski LE, Khatib R. Cytomegalovirus colitis in the immunocompetent host: an overview. Scand J Infect Dis. 1998;30:559-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 76] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Galiatsatos P, Shrier I, Lamoureux E, Szilagyi A. Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts. Dig Dis Sci. 2005;50:609-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 150] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 8. | Taniwaki S, Kataoka M, Tanaka H, Mizuno Y, Hirose M. Multiple ulcers of the ileum due to Cytomegalovirus infection in a patient who showed no evidence of an immunocompromised state. J Gastroenterol. 1997;32:548-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Keates J, Lagahee S, Crilley P, Haber M, Kowalski T. CMV enteritis causing segmental ischemia and massive intestinal hemorrhage. Gastrointest Endosc. 2001;53:355-359. [PubMed] |
| 10. | Siegal DS, Hamid N, Cunha BA. Cytomegalovirus colitis mimicking ischemic colitis in an immunocompetent host. Heart Lung. 2005;34:291-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Caroline DF, Hilpert PL, Russin VL. CMV colitis mimicking Crohn's disease in a patient with acquired immune deficiency syndrome (AIDS). Can Assoc Radiol J. 1987;38:227-228. [PubMed] |
| 12. | Karakozis S, Gongora E, Caceres M, Brun E, Cook JW. Life-threatening cytomegalovirus colitis in the immunocompetent patient: report of a case and review of the literature. Dis Colon Rectum. 2001;44:1716-1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Sakamoto I, Shirai T, Kamide T, Igarashi M, Koike J, Ito A, Takagi A, Miwa T, Kajiwara H. Cytomegalovirus enterocolitis in an immunocompetent individual. J Clin Gastroenterol. 2002;34:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |