Published online Aug 21, 2006. doi: 10.3748/wjg.v12.i31.5010
Revised: October 21, 2005
Accepted: October 26, 2005
Published online: August 21, 2006
AIM: To investigate the optimal strategy to treat dyspeptic patients in primary care.
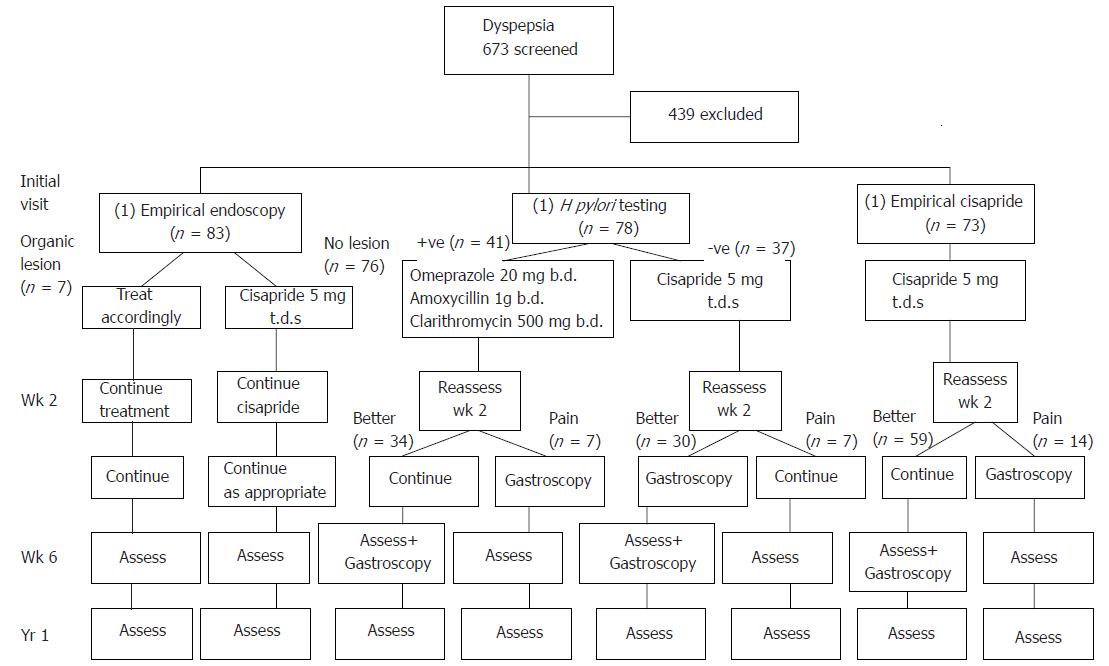
METHODS: Dyspeptic patients presenting to primary care outpatient clinics were randomly assigned to: (1) empirical endoscopy, (2) H pylori test-and-treat, and (3) empirical prokinetic treatment with cisapride. Early endoscopy was arranged if patients remained symptomatic after 2 wk. Symptom severity, quality-of-life (SF-36) as well as patient preference and satisfaction were assessed. All patients underwent endoscopy by wk 6. Patients were followed up for one year.
RESULTS: Two hundred and thirty four patients were recruited (163 female, mean age 49). 46% were H pylori positive. 26% of H pylori tested and 25% of empirical prokinetic patients showed no improvement at wk 2 follow-up and needed early endoscopy. 15% of patients receiving empirical cisapride responded well to treatment but peptic ulcer was the final diagnosis. Symptom resolution and quality-of-life were similar among the groups. Costs for the three strategies were HK$4343, $1771 and $1750 per patient. 66% of the patients preferred to have early endoscopy.
CONCLUSION: The three strategies are equally effective. Empirical prokinetic treatment was the least expensive but peptic ulcers may be missed with this treatment. The H pylori test-and-treat was the most cost-effective option.
- Citation: Hu WH, Lam S, Lam CL, Wong W, Lam K, Lai K, Wong Y, Wong BC, Chan AO, Chan C, Leung GM, Hui W. Comparison between empirical prokinetics, Helicobacter test-and-treat and empirical endoscopy in primary-care patients presenting with dyspepsia: A one-year study. World J Gastroenterol 2006; 12(31): 5010-5016
- URL: https://www.wjgnet.com/1007-9327/full/v12/i31/5010.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i31.5010
Dyspepsia, defined as pain or discomfort centered in the upper abdomen, is a common complaint, affecting 18.5% of the population in our locality[1]. Underlying pathology ranges from functional dyspepsia, peptic ulcer to gastrointestinal cancer. Among the various aetiologies, functional dyspepsia is the most common diagnosis in community-based patients[2]; Up to 79% of dyspeptic patients referred from primary care for open-access endoscopy have normal endoscopic findings[3].
Primary care medicine is the first point of presentation for dyspeptic patients. Studies have suggested that dyspepsia alone accounts for 20%-70% of all gastrointestinal consultations with general practitioners; up to one-third of these patients may eventually be referred to a gastroenterologist[4]. The financial burden for diagnosis and treatment of this common condition is therefore great.
It is unclear how dyspepsia should be investigated and treated in primary care settings, but there are several common approaches. Empirical endoscopy would theoretically be the gold standard in diagnostic accuracy, but it is expensive and invasive. Empirical H2 receptor antagonist therapy has been extensively studied, but has not been shown to have superior cost-benefit over empirical endoscopy[5]. In addition, there may be concerns that antisecretory treatment may mask symptoms of gastric cancer and lead to a delay in diagnosis.
Another possible approach is to test for H pylori. The close association between H pylori and chronic gastritis that accompanies peptic ulcer disease and gastric cancer offers an opportunity to screen for organic disease based on the presence of the bacterium.
An alternate approach is empirical prokinetic treatment. Studies have demonstrated that cisapride and domperidone are beneficial in the treatment of functional dyspepsia over placebo[6-8]. By adopting this approach, the majority of patients with functional dyspepsia could be treated appropriately whereas the smaller number of patients with organic dyspepsia may not benefit from this treatment. Persistence of dyspepsia in this group would then lead to endoscopy and diagnosis. The small delay in diagnosis is not unreasonable since, in real life, many primary care doctors would give antacids to dyspeptic patients without alarm features and monitor symptoms on follow-up. Cisapride has been withdrawn from most markets since this study was carried out though related drugs such as mosapride are still in use in some countries.
In this study, we investigated empirical endoscopy, H pylori test-and-treat, and empirical prokinetic therapy as possible diagnostic and treatment strategies in primary-care patients presenting with dyspepsia.
Patients aged 18 or older presenting with a primary complaint of previously uninvestigated dyspepsia in four government-run primary-care clinics in Hong Kong were recruited for the study. Dyspepsia was defined as pain or discomfort centered in the upper abdomen[9]. History and physical examination were carried out by the primary care physician.
Exclusion criteria for this study were current intake of drugs other than antacids for dyspepsia, previous peptic ulcer disease, history of gastric surgery, presence of malignancy within the previous five years, history of intake of aspirin or non-steroidal anti-inflammatory drugs in the previous four weeks, presence of alarm symptoms, such as weight loss and gastrointestinal haemorrhage, and clinical suspicion of an organic cause of dyspepsia. In addition, those with a family history of sudden death, history of palpitations, co-existing intake of drugs that may interact with cisapride and those with an abnormal electrocardiogram were excluded.
After obtaining written consent for the trial, a locally-validated 13-C urea breath test was administered in the primary care clinic. The details of the breath test have been described elsewhere, and had a sensitivity and specificity of 96.5% and 97.7% respectively[10]. The results were not disclosed to the patients until after the trial unless the patients were randomised into the H pylori test-and-treat group.
The patients were subsequently reassessed by one of the investigators in the gastroenterological unit of Queen Mary Hospital within 24 h of initial presentation. Inclusion and exclusion criteria were checked and a complete physical examination was performed. Electrocardiography was also performed on all recruited patients. A previously validated Chinese (Hong Kong) version of the SF-36 health survey[11], as well as a validated twelve-item dyspepsia symptom severity score[12] were administered. Patients were then randomised using a computer-generated sequence into one of three investigation and treatment groups as detailed below.
This study was approved by the research and ethics committee, faculty of medicine, the University of Hong Kong.
Patients in this group received endoscopy on the initial day attending the gastrointestinal unit. Oesophagogastroduodenoscopy was performed by one of the investigators and an endoscopic diagnosis was made. A rapid urease test was performed if the patient had peptic ulcer disease and biopsies for histology were taken for gastric ulcers and suspicious lesions.
Patients with organic diagnoses were treated accor-dingly. H pylori eradication therapy was given to those with peptic ulcers or erosive gastritis with a positive test for the bacterium.
Dyspeptic patients with normal endoscopy or non-erosive gastritis were considered to have functional dyspepsia and were treated with cisapride 5 mg three times daily for six weeks.
Patients who tested positive for H pylori in the 13C urease breath test received omeprazole 20 mg twice daily, amoxycillin 1 g twice daily, and clarithromycin 500 mg twice daily. The local eradication rate for this regimen is 87.8%[13]. Patients who tested negative for H pylori were treated as functional dyspepsia and given cisapride 5 mg three times daily for six weeks.
All patients in this group were given cisapride 5 mg three times daily for six weeks regardless of H pylori positivity (Figure 1).
Patients were followed-up at two weeks, six weeks and one year after the initial treatment. At follow-up the dyspepsia symptom score and SF-36 survey were administered by an assessor blinded to the purpose of the study. Satisfaction of patients in regard to treatment was assessed at wk 6 using a 4-point Likert scale ranging from dissatisfied to very satisfied. Patients were asked whether they prefered endoscopy or a trial of drug treatment as the initial approach to their dyspspsia.
If the symptoms had not improved after two weeks of treatment, endoscopy was performed on group 2 and 3 patients. Organic pathology discovered at endoscopy was treated appropriately. For patients who had empirical endoscopy, no further investigation was offered unless there was a change in symptoms that raised suspicion of organic disease. At the end of the study, all patients who had not previously received endoscopy received an oesophagoduodenogastroscopy for a definitive diagnosis.
Sample size was determined using NCSS PASS 2002 (NCSS statistical software, Kaysville, Utah, USA). A previous study designed to develop dyspepsia severity scores found a mean of 20.7 and standard deviation of 3.8 in a local population of dyspeptic patients. The difference in mean symptom score between patients who felt better and those who did not was 1.2[12]. Based on this result we estimated that 70 patients in each of the three groups would report a two-point difference in the mean symptom score between one group and the other two with a power of 0.9 and significance level of 0.05.
Cost analysis was performed to examine the economic implications of the three strategies studied. The analysis was carried out from the provider’s perspective, given all three treatment regimens were ambulatory procedures and therefore, assumed to incur similar direct personal, indirect and intangible costs to the patients and society generally. Costs were calculated according to the gazetted list of fees and charges of the Hong Kong Hospital Authority and hospital formulary costs.
The study was analysed according to intention-to-treat. Comparison of baseline dyspepsia scores and quality-of-life domains was made using one-way ANOVA and the Kruskal-Wallis test. Correlation between baseline dyspepsia scores and quality-of-life domains was calculated using Kendall’s tau. Quality-of-life and dyspepsia symptom scores after treatment were compared among the three groups using a repeated measures procedure. The null hypotheses regarding the main effects of time points and three treatment groups, and the interaction between treatment groups and different time points were tested using multivariate analysis. Age and sex were also included as covariables. Statistical analyses were performed using SPSS version 11.0 for windows (SPSS inc., Chicago, Illinois, USA).
Six hundred and seventy three patients were screened for inclusion in the study, of which 234 were recruited (mean age 49, range 18-79, 163 female). Reasons for exclusion included dyspepsia under treatment (257), refusal to participate (49), previous investigations for dyspepsia (51), non-steroidal antiinflammatory agent intake[25], previous gastric surgery or peptic ulcer history[34], alarm symptoms[12] abnormal electrocardiogram[6] and other malignancy[3]. Baseline characteristics of the three groups of patients are as tabulated in Table 1. All patients completed the six-week treatment assessment period. One hundred and eighty one (77.4% overall; 77.1%, 69.2% and 86.3% in the three respective groups) attended one-year follow-up.
| Group | Mean age | Sex (M/F) | Hpylori positive (%) | Mean baseline dyspepsia score |
| Empirical endoscopy (n = 83) | 52.5 ± 13.2 | 25/58 | 37 (44.6%) | 20.4 ± 4.0 |
| H pylori test-and-treat (n = 78) | 46.5 ± 14.2 | 24/54 | 41 (52.6%) | 20.8 ± 3.8 |
| Empirical prokinetics (n = 73) | 48.6 ± 13.0 | 22/51 | 30 (41.1%) | 19.6 ± 3.8 |
| P value | 0.01a | 0.99 | 0.35 | 0.16 |
Group one patients had endoscopy before commencing treatment and provided the most accurate data of the underlying diagnoses of dyspepsia. Among the 83 patients receiving empirical endoscopy 76 (91.5%) had normal findings or non-erosive gastritis, two (2.4%) had gastric erosions, four (4.8%) had peptic ulcer and one (1.2%) had oesophagitis. Endoscopic findings for the three groups are summarised in Table 2. Overall, 46% of patients were H pylori positive.
| Normal | Gastritis/ | Gastric | Gastric | Duodenal | Oesop- | |
| duodenitis | erosions | ulcer | ulcer | hagitis | ||
| Empirical endoscopy (n = 83) | 49 (59) | 27 (32.5) | 2 (2.4) | 3 (3.6) | 1 (1.2) | 1 (1.2) |
| H pylori test-and- treat (n = 78) | 61 (78.2) | 10 (12.8) | 4 (5.1) | 0 | 3 (3.9) | 0 |
| Empirical prokinetics (n = 73) | 46 (63.0) | 17 (23.3) | 4 (5.5) | 3 (4.1) | 3 (4.1) | 0 |
Fourteen patients (18%) randomised to the H pylori test-and-treat group had persistent dyspepsia after two weeks of treatment and needed early endoscopy. None of these patients had organic dyspepsia; two had non-erosive gastritis and 12 had normal endoscopy. At six weeks, three patients with symptom resolution after treatment were found to have duodenal ulcers and three had gastroduodenal erosions. All of these patients were originally tested to be positive for H pylori and had received appropriate eradication therapy, but the ulcer had not completely healed by the time of endoscopy.
Fourteen patients (19%) randomised to empirical prokinetic therapy had persistent dyspepsia at two weeks follow-up and received early endoscopy. Eleven of these patients had normal endoscopy results or non-erosive gastritis, two had gastroduodenal erosions and one had a gastric ulcer. More importantly, at the final diagnostic endoscopy, two patients were found to have erosions, duodenal ulcer and gastric ulcer among those who reported symptomatic improvement after treatment. If endoscopy was not performed, these organic lesions would have likely been missed.
All gastric ulcers detected in this study were benign.
The mean baseline dyspepsia severity score was 20.3 ± 3.9 and was not significantly different among the three groups studied (Table 1). After six weeks of treatment, there was a decrease in mean symptom score to 15.0 ± 2.9 (5.6, 5.6 and 4.4 for empirical endoscopy, H pylori testing and empirical cisapride, respectively). On one year follow-up, the mean dyspepsia score increased to 19.7 ± 7.2. Repeated measures analysis showed no significant effect of treatment group on dyspepsia severity. However, patients with organic causes of dyspepsia were less symptomatic than those with non-ulcer dyspepsia after one year (Table 3).
The SF-36 health-related quality-of-life scores for the various domains are tabulated in Table 4. At baseline, there was no difference in quality-of-life between the three groups of patients. There was a significant correlation between the severity of dyspepsia and the BP, GH, MH, RE, RP, SF and VT domains, but not the PF domain at baseline. At one-year follow-up, there was a general decline in quality-of-life when compared to 6 wk follow-up. Repeated measures analysis again showed no significant effect of treatment group on quality of life.
| BP | GH | MH | PF | RE | RP | SF | VT | |
| All groups | 63/84/51 | 40/47/42 | 72/72/60 | 95/95/85 | 100/100/67 | 50/100/75 | 88/88/75 | 45/50/50 |
| Empirical endoscopy | 62/84/51 | 50/52/50 | 72/72/60 | 95/95/85 | 100/100/67 | 75/100/75 | 75/100/75 | 50/45/50 |
| H pylori test-and-treat | 62/84/51 | 40/45/36 | 68/72/60 | 95/95 80 | 67/100/33 | 50/100/75 | 75/88/63 | 45/45/45 |
| Empirical Prokinetics | 72/84/52 | 39/49/45 | 76/72/64 | 95/95/85 | 100/100/67 | 50/100/75 | 88/88/75 | 45/50/50 |
The calculated six-week investigation and treatment costs for empirical endoscopy, H pylori test-and-treat and empirical prokinetic therapies are HK$4343, $1771 and $1750 per patient, respectively.
Overall, 81% of patients were either satisfied or very satisfied with treatment. There was no significant difference in satisfaction among the three diagnostic paradigms that were tested (Table 5). 66% of patients preferred to have endoscopy before taking medication; the differences in scores were again not significant among groups (Table 5).
| Very | Satisfied | Neutral | Dissatisfied | Prefer initial | |
| satisfied | endoscopy | ||||
| Empirical Endoscopy (n = 83) | 7 (8.4) | 59 (71) | 14 (17) | 3 (3.6) | 63 (75.9) |
| H pylori test-and-treat (n = 78) | 6 (7.7) | 53 (67.9) | 14 (17.9) | 5 (6.4) | 48 (61.5) |
| Empirical Prokinetics (n = 73) | 6 (8.2) | 56 (76.7) | 8 (11.0) | 3 (4.1) | 43 (59.0) |
No patient given cisapride reported significant palpitations or other side effects. All patients were able to complete the six-week course of treatment.
Underlying diagnoses of dyspepsia range from peptic ulcer, gastric cancer to functional dyspepsia, and it may be difficult to determine cause without investigation. Age, symptom assessment and even the presence of alarm symptoms appear to be poor predictors of underlying pathology[14]. However, despite the prevalence and potential high economic cost of this condition, the optimal strategy to manage dyspepsia in primary care practice remains unclear[15].
Community-based studies have generally indicated that peptic ulcer and cancer are uncommon causes of dyspepsia[2], accounting for only 20% of patients referred to open-access endoscopy[3]. Therefore, it is reasonable that any investigative and treatment strategy should be effective in functional dyspepsia, representing the bulk of patients. The optimal approach to investigation and treatment would aim to: (1) provide the most efficacious and cost-effective treatment for functional dyspepsia, (2) allow for prompt treatment of patients with peptic ulcer, with H pylori eradication, if appropriate, (3) correctly diagnose malignant lesions so that definitive treatment can be given and (4) to avoid unnecessary treatment for patients with functional dyspepsia.
Several treatments have generally been shown to be better than placebo in the treatment of functional dyspepsia. Meta-analysis studies have estimated a 20% gain of H2 antagonist treatment against placebo[16], but there may not be global improvement in symptoms[17]. Proton pump inhibitors may benefit dyspeptic patients with co-existing reflux[18]; a study reported 10% therapeutic gain over placebo treatment but efficacy seems to be limited to patients with ulcer-like symptoms[19]. Cisapride has also been extensively evaluated in studies, though many studies had methodological deficiencies[20]. Meta-analyses have generally found a therapeutic gain of 36%-39% when compared to placebo[16,21] but publication bias may have contributed to these results. H pylori eradication is likewise controversial, with some studies showing a long-term benefit[22], and others showing no benefit[23].
Various options have been suggested in the investigation and treatment of patients presenting with dyspepsia. The American Gastroenterological Association has suggested that patients over the age of 45 years or those with alarm features should have empirical endoscopy[24]. For younger patients without alarm symptoms, there may be several options: (1) empirical medical therapy (antisecretory drugs or prokinetics) with investigation for therapeutic failures, (2) immediate diagnosis with endoscopy, (3) testing for H pylori and studying positive subjects, and (4) testing for H pylori and treating positive cases with eradication[24]. An Asian Pacific guideline also suggested a trial of antisecretory drugs or prokinetics for 2-4 wk[25]. Among the alternatives, empirical prokinetic treatment has not been evaluated in previous studies.
Bytzer randomised 414 patients into groups receiving empirical endoscopy or ranitidine[5]. Empirical treatment was associated with higher costs of ulcer drug use and a greater number of sick days. It was also notable that 33% of patients had organic causes of dyspepsia, compared to 8% in the present study. Another study comparing H pylori test-and-treat with endoscopy found greater patient satisfaction with endoscopy but comparable symptoms and sick leave days between the two groups[26]. Comparative costs depend on individual centres. An American study reported similar costs between H pylori testing and empirical endoscopy[27] whereas another claimed lower costs for H pylori eradication[28]. A decision analysis supported a trial of proton pump inhibitor before endoscopy or test-and-treat[29]. Test and endoscopy in primary care has been shown to increase endoscopy rates without benefit in symptom relief or quality of life[30]. It is of note, however, that proton pump inhibitors may not be as efficacious in Asian populations; a paper using the same outcome instruments as the present study failed to show any benefit of four-week lansoperazole treatment over placebo in patients with functional dyspepsia[31].
Most of the studies comparing different diagnostic strategies concentrated on cost. Less data is available concerning symptom resolution and quality of life. Many dyspeptic patients presenting for medical care have a fear of serious disease and malignancy[32]. In addition they are more anxious than non-presenters with similar complaints[1]. It is possible that a completely normal endoscopy may relieve some of the anxiety. Indeed a study on barium meal in dyspeptic patients who were referred from general practice showed that the examination increased management confidence and allayed patients’ anxiety[33]. In this study, however, we failed to show any significant difference in symptom relief among the three groups, indicating that the comforting effect of a negative endoscopy may not be an important factor in the cure of functional dyspepsia.
We have calculated the cost of treatment and empirical endoscopy is most costly, followed by H pylori test-and-treat and the lowest cost was for empirical prokinetics. The high cost for empirical endoscopy in the present study is related to the relatively low rates of endoscopy for patients randomised to the other groups. In the H pylori test-and-treat and empirical cisapride groups, 18% and 19% of patients respectively had persistent dyspepsia after two weeks of treatment and needed early endoscopy. In Bytzer’s study, 136 out of 206 patients randomised to empirical H2 blocker therapy had therapeutic failure and required endoscopy[5]. The difference may be due to differences in length of follow-up and also the lower rate of organic pathology in our study. In our population with dyspepsia, 8.5% had organic causes (empirical endoscopy group), compared with 33% prevalence of organic dyspepsia reported by Bytzer. The overall rate of organic dyspepsia is also lower than the rate in our previous study on open-access endoscopy, where 21% had organic pathology[3]. The difference probably reflects differences in referral patterns, with family physicians referring more severe cases of dyspepsia for immediate endoscopy in the previous study.
We observed a high relapse rate of dyspepsia generally, with the mean dyspepsia severity score returning to the initial level on one-year follow-up. This is due to non-ulcer/functional dyspepsia being the predominant diagnosis in 92% of patients. Functional dyspepsia is a chronic disease that persists in patients; a study reported that 74% of dyspeptic patients are still symptomatic two years after the initial diagnosis[34]. In contrast, the few patients with peptic ulcer in this study tended to remain asymptomatic after the ulcer has healed and these patients in fact have a better prognosis as far as symptom relapse is concerned.
Both empirical endoscopy and H pylori testing appeared to be safe options with similar patient satisfaction. All patients with organic dyspepsia were tested to be positive for H pylori and had appropriate eradication therapy. However, the main drawback in the study was the absence of malignancy; it was not possible to predict whether gastric cancers would have been missed by any approach. Although rare in younger patients, gastric cancers may present without sinister symptoms. A Canadian study reported a prevalence of 1.05 per thousand patients under 45 years presenting with dyspepsia without alarm symptoms[35]. We may expect higher numbers in Asia, with a higher population prevalence of gastric cancer. The possibility of missing or delay in diagnosis of gastric malignancies needs to be considered in empirical treatment approaches.
Since all patients with duodenal or gastric ulcer were positive for H pylori, another approach may be performing endoscopy only on those with a positive 13C urea breath test. Such an approach may prevent 54% of endoscopies. However, 60% of the patients with gastric erosions were negative for H pylori; inappropriate treatment of these patients may potentially lead to progression into ulcer disease.
There is limited data on empirical prokinetic treatment. Because of association with cardial arrhythmia, the drug has been withdrawn in most markets. However, related drugs, such as mosapride, are still used in some countries and this study may throw light on the effectiveness of other prokinetic agents. In the present study we found this strategy to be associated with the lowest cost but with similar outcome regarding symptomatic improvement. However, interestingly, although prokinetic treatment was not targeted for the treatment of peptic ulcers, six patients (2 gastric ulcer, 2 duodenal ulcer, 2 gastric erosions) reported symptomatic improvement after cisapride alone and would not have received definitive therapy. Because of the dangers of misdiagnosing patients with peptic ulcers, empirical cisapride therapy could not be recommended. Despite concerns over potential QT interval prolongation and ventricular arrhythmia, a relatively low dose of 5 mg three times daily was not associated with any adverse event in our sample of patients.
In conclusion, most patients presenting to primary care physicians with dyspepsia appear to have non-ulcer dyspepsia, which is associated with a high one-year relapse rate. Empirical endoscopy, H pylori test-and-treat and empirical prokinetic treatments appear to have similar efficacy in improvement of dyspepsia and quality-of-life. Empirical prokinetics may result in organic lesions being missed in diagnosis. Most patients preferred having endoscopy first, if given the choice, but this is the most expensive option. H pylori test-and-treat is the most cost-effective safe treatment.
We are indebted to the doctors and nurses of the Violet Peel, Sai Ying Pun, Aberdeen and Ap Lei Chau government outpatient clinics for recruitment of patients and Ms. Monique Chong, Ms. Vera Tang, Ms. Wong Ka-Wah, Ms. Diana Chang, Ms. Wing-Ping Yung for their assistance in the endoscopy room.
S- Editor Wang J L- Editor Lutze M E- Editor Bai SH
| 1. | Hu WH, Wong WM, Lam CL, Lam KF, Hui WM, Lai KC, Xia HX, Lam SK, Wong BC. Anxiety but not depression determines health care-seeking behaviour in Chinese patients with dyspepsia and irritable bowel syndrome: a population-based study. Aliment Pharmacol Ther. 2002;16:2081-2088. [PubMed] [DOI] [Full Text] |
| 2. | Bernersen B, Johnsen R, Straume B, Burhol PG, Jenssen TG, Stakkevold PA. Towards a true prevalence of peptic ulcer: the Sørreisa gastrointestinal disorder study. Gut. 1990;31:989-992. [PubMed] [DOI] [Full Text] |
| 3. | Wong BC, Chan CK, Wong KW, Wong WM, Yuen MF, Lai KC, Hu WH, Lau GK, Lai CL, Lam SK. Evaluation of a new referral system for the management of dyspepsia in Hong Kong: role of open-access upper endoscopy. J Gastroenterol Hepatol. 2000;15:1251-1256. [PubMed] |
| 4. | Knill-Jones RP. Geographical differences in the prevalence of dyspepsia. Scand J Gastroenterol Suppl. 1991;182:17-24. [PubMed] [DOI] [Full Text] |
| 5. | Bytzer P, Hansen JM, Schaffalitzky de Muckadell OB. Empirical H2-blocker therapy or prompt endoscopy in management of dyspepsia. Lancet. 1994;343:811-816. [PubMed] [DOI] [Full Text] |
| 6. | Rösch W. Cisapride in non-ulcer dyspepsia. Results of a placebo-controlled trial. Scand J Gastroenterol. 1987;22:161-164. [PubMed] [DOI] [Full Text] |
| 7. | Carvalhinhos A, Fidalgo P, Freire A, Matos L. Cisapride compared with ranitidine in the treatment of functional dyspepsia. Eur J Gastroenterol Hepatol. 1995;7:411-417. [PubMed] |
| 8. | Deruyttere M, Lepoutre L, Heylen H, Samain H, Pennoit H. Cisapride in the management of chronic functional dyspepsia: a multicenter, double-blind, placebo-controlled study. Clin Ther. 1987;10:44-51. [PubMed] |
| 9. | Drossman DA, Corazziari E, Talley NJ. Rome II: the functional gastrointestinal disorders: diagnosis, pathophysiology, and treatment: a multinational consensus. 2nd ed. Mc Lean, Virginia, USA: Degnon Associates 2000; . |
| 10. | Wong WM, Wong BC, Wong KW, Fung FM, Lai KC, Hu WH, Yuen ST, Leung SY, Lau GK, Lai CL. (13)C-urea breath test without a test meal is highly accurate for the detection of Helicobacter pylori infection in Chinese. Aliment Pharmacol Ther. 2000;14:1353-1358. [PubMed] [DOI] [Full Text] |
| 11. | Lam CL, Gandek B, Ren XS, Chan MS. Tests of scaling assumptions and construct validity of the Chinese (HK) version of the SF-36 Health Survey. J Clin Epidemiol. 1998;51:1139-1147. [PubMed] [DOI] [Full Text] |
| 12. | Hu WH, Lam KF, Wong YH, Lam CL, HUIi WM, Lai KC, Wong BC, Lam SK. The Hong Kong index of dyspepsia: a validated symptom severity questionnaire for patients with dyspepsia. J Gastroenterol Hepatol. 2002;17:545-551. [PubMed] [DOI] [Full Text] |
| 13. | Lai KC, Hui WM, Wong BC, Hu WH, Lam SK. Ulcer-healing drugs are required after eradication of Helicobacter pylori in patients with gastric ulcer but not duodenal ulcer haemorrhage. Aliment Pharmacol Ther. 2000;14:1071-1076. [PubMed] [DOI] [Full Text] |
| 14. | Wallace MB, Durkalski VL, Vaughan J, Palesch YY, Libby ED, Jowell PS, Nickl NJ, Schutz SM, Leung JW, Cotton PB. Age and alarm symptoms do not predict endoscopic findings among patients with dyspepsia: a multicentre database study. Gut. 2001;49:29-34. [PubMed] [DOI] [Full Text] |
| 15. | Hu WH, Talley NJ. Functional (non-ulcer) dyspepsia: unexplained but not unmanageable. Med J Aust. 1998;168:507-512. [PubMed] |
| 16. | Dobrilla G, Comberlato M, Steele A, Vallaperta P. Drug treatment of functional dyspepsia. A meta-analysis of randomized controlled clinical trials. J Clin Gastroenterol. 1989;11:169-177. [PubMed] [DOI] [Full Text] |
| 17. | Talley NJ, McNeil D, Hayden A, Piper DW. Randomized, double-blind, placebo-controlled crossover trial of cimetidine and pirenzepine in nonulcer dyspepsia. Gastroenterology. 1986;91:149-156. [PubMed] |
| 18. | Fennerty MB. Use of antisecretory agents as a trial of therapy. Gut. 2002;50 Suppl 4:iv63-iv66. [PubMed] [DOI] [Full Text] |
| 19. | Talley NJ, Meineche-Schmidt V, Paré P, Duckworth M, Räisänen P, Pap A, Kordecki H, Schmid V. Efficacy of omeprazole in functional dyspepsia: double-blind, randomized, placebo-controlled trials (the Bond and Opera studies). Aliment Pharmacol Ther. 1998;12:1055-1065. [PubMed] [DOI] [Full Text] |
| 20. | Bytzer P. H(2) receptor antagonists and prokinetics in dyspepsia: a critical review. Gut. 2002;50 Suppl 4:iv58-iv62. [PubMed] [DOI] [Full Text] |
| 21. | Finney JS, Kinnersley N, Hughes M, O'Bryan-Tear CG, Lothian J. Meta-analysis of antisecretory and gastrokinetic compounds in functional dyspepsia. J Clin Gastroenterol. 1998;26:312-320. [PubMed] [DOI] [Full Text] |
| 22. | McColl K, Murray L, El-Omar E, Dickson A, El-Nujumi A, Wirz A, Kelman A, Penny C, Knill-Jones R, Hilditch T. Symptomatic benefit from eradicating Helicobacter pylori infection in patients with nonulcer dyspepsia. N Engl J Med. 1998;339:1869-1874. [PubMed] [DOI] [Full Text] |
| 23. | Blum AL, Talley NJ, O'Moráin C, van Zanten SV, Labenz J, Stolte M, Louw JA, Stubberöd A, Theodórs A, Sundin M. Lack of effect of treating Helicobacter pylori infection in patients with nonulcer dyspepsia. Omeprazole plus Clarithromycin and Amoxicillin Effect One Year after Treatment (OCAY) Study Group. N Engl J Med. 1998;339:1875-1881. [PubMed] [DOI] [Full Text] |
| 24. | American Gastroenterological Association medical position statement: evaluation of dyspepsia. Gastroenterology. 1998;114:579-581. [PubMed] [DOI] [Full Text] |
| 25. | Talley NJ, Lam SK, Goh KL, Fock KM. Management guidelines for uninvestigated and functional dyspepsia in the Asia-Pacific region: First Asian Pacific Working Party on Functional Dyspepsia. J Gastroenterol Hepatol. 1998;13:335-353. [PubMed] [DOI] [Full Text] |
| 26. | Lassen AT, Pedersen FM, Bytzer P, Schaffalitzky de Muckadell OB. Helicobacter pylori test-and-eradicate versus prompt endoscopy for management of dyspeptic patients: a randomised trial. Lancet. 2000;356:455-460. [PubMed] [DOI] [Full Text] |
| 27. | Silverstein MD, Petterson T, Talley NJ. Initial endoscopy or empirical therapy with or without testing for Helicobacter pylori for dyspepsia: a decision analysis. Gastroenterology. 1996;110:72-83. [PubMed] [DOI] [Full Text] |
| 28. | Ofman JJ, Etchason J, Fullerton S, Kahn KL, Soll AH. Management strategies for Helicobacter pylori-seropositive patients with dyspepsia: clinical and economic consequences. Ann Intern Med. 1997;126:280-291. [PubMed] [DOI] [Full Text] |
| 29. | Spiegel BM, Vakil NB, Ofman JJ. Dyspepsia management in primary care: a decision analysis of competing strategies. Gastroenterology. 2002;122:1270-1285. [PubMed] [DOI] [Full Text] |
| 30. | Delaney BC, Wilson S, Roalfe A, Roberts L, Redman V, Wearn A, Hobbs FD. Randomised controlled trial of Helicobacter pylori testing and endoscopy for dyspepsia in primary care. BMJ. 2001;322:898-901. [PubMed] [DOI] [Full Text] |
| 31. | Wong WM, Wong BC, Hung WK, Yee YK, Yip AW, Szeto ML, Fung FM, Tong TS, Lai KC, Hu WH. Double blind, randomised, placebo controlled study of four weeks of lansoprazole for the treatment of functional dyspepsia in Chinese patients. Gut. 2002;51:502-506. [PubMed] [DOI] [Full Text] |
| 32. | Howell S, Talley NJ. Does fear of serious disease predict consulting behaviour amongst patients with dyspepsia in general practice. Eur J Gastroenterol Hepatol. 1999;11:881-886. [PubMed] [DOI] [Full Text] |
| 33. | Conry BG, McLean AM, Farthing MJ. Diagnostic and therapeutic efficacy of barium meal examination: a prospective evaluation in general practice. BMJ. 1989;299:1443-1445. [PubMed] [DOI] [Full Text] |
| 34. | Jones R, Lydeard S. Dyspepsia in the community: a follow-up study. Br J Clin Pract. 1992;46:95-97. [PubMed] |