Published online Aug 7, 2006. doi: 10.3748/wjg.v12.i29.4736
Revised: November 28, 2005
Accepted: February 18, 2006
Published online: August 7, 2006
AIM: To design a hand-assisted laparoscopic approach in an attempt to provide an option for laparoscopic resection of abdominal large viscera.
METHODS: A 5-6 cm incision (for HandPort) and 2 trocars were employed. The main vessel of the target organ was taken as a “core”, and all tissues around the core were taken as peripheral structures. The peripheral structures were dissected first, and the core vessels were treated last. Twenty-six patients underwent laparoscopic deroofing of the hepatic huge cysts, resection of the segments lying at the outer edge of the liver (segments 2 to 6), splenectomy, hemicolectomy, ileocecectomy and subtotal gastrectomy with HandPort device, harmonic scalpel, or Ligasure.
RESULTS: The duration of the procedure was within 2 hours. Blood loss amounted to 8-120 mL. The conversion rate was 3.8% (1/26). All patients had uneventful postoperative courses with less pain, earlier oral intake, and faster recovery, compared with conventional surgery.
CONCLUSION: This method combines the advantages of both open and laparoscopic techniques, achieving better hemostasis effect, shortening the operative time, and is beneficial to the patients.
- Citation: Dai LH, Xu B, Zhu GH. Hand-assisted laparoscopic surgery of abdominal large visceral organs. World J Gastroenterol 2006; 12(29): 4736-4740
- URL: https://www.wjgnet.com/1007-9327/full/v12/i29/4736.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i29.4736
Since Mouret performed the successful laparoscopic cholecystectomy in 1987, new frontiers have opened for minimally invasive surgery[1], and has been expanded to more extensive procedures such as resection of the abdominal large viscera[2-4]. The minimally invasive surgery is superior to conventional open surgery because it offers significant benefits to the patients including much shorter incision, less pain and faster recovery. Despite instrumentation has dramatically improved over the past decade, laparoscopic resection of abdominal large organ still has several concerns regarding the safety, technical difficulties, rapidity and complications such as bleeding, injury to major adjacent structures, which affect the short-term and long-term outcomes[5].
In an effort to largely simplify and shorten the procedure, provide an easier, safer approach, and decrease patients’ postoperative pain and stay, we have designed a method for laparoscopic resection of abdominal large viscera. Usually, several 5-12 mm trocars are placed in the abdominal wall in laparoscopic surgery. However, there must be 5-6 cm port for extraction of a resected specimen in removal of abdominal large visceral organ. From “1 port + 2 trocars” as the minimal invasive wounds, we used a quick and safe hand-assisted laparoscopic technique for resection of abdominal large viscera, by taking advantages of both open and laparoscopic techniques.
From May 2001 to December 2002, 26 patients, 15 males and 11 females with a mean age of 61.8 yeas (range 42-71 years), underwent hand-assisted laparoscopic surgery involving resection of liver, spleen, colon, jejunum, ileocecum, stomach and gallbladder, including 2 emergency operations: a 71 year-old female had uncontrolled bleeding from multiple diverticulosis of ascending colon, and another 54 year-old female suffered from carcinoma of terminal ileum associated with ileus. The procedure was carried out endocorporeally and extracorporeally, by means of the HandPort system (Smith & Nephew Inc. Andover, Massachusetts), harmonic scalpel (HCS 15 and HCS C5, Ethicon, Endo-surgery, Cincinnati, Ohio. Ultra shears 5 mm instrument, US Surgical, Tyco Healthcare) or Ligasure(10 mm Atlas, Vallylab, Boulder, Tyco Healthcare). All procedures were performed with the patients in the supine position, rotated appropriately, or with rolls under the flank of the appropriate side. The operations and indicating diseases are listed in Table 1.
| Cases | Operations | Indicating diseases |
| 1-2 | Left lateral segmentectomy | Hepatitis B-related cirrhosis supervened hepatocellular carcinoma (HCC), hepatic cavernous hemangioma |
| 3 | S 6 segmentectomy | Hepatitis B-related cirrhosis supervened HCC |
| 4 | S 5 and 6 segmentectomy | Hepatitis B-related cirrhosis supervened HCC |
| 5 | S 5, 6 and partial 4 segmentectomy + cholecystectomy | Hepatitis B-related cirrhosis supervened HCC |
| 6 | Partial S 4 segmentectomy | Hepatic cavernous hemangioma |
| 7-11 | Deroofing of the hepatic huge cysts | The 4, 6, 7, 8 segmental hepatic cysts; the 4, 5, 6, 7, 8 segmental hepatic cysts; the 5, 6, 7 segmental hepatic cysts (2); the 5, 6, 7 segmental hepatic cysts with calcification of cystic wall |
| 12-15 | Right hemicolectomy | Carcinoma of the ascending colon (3) 1Multiple diverticulosis of ascending colon with massive hemorrhage |
| 16 | Left hemicolectomy + partial jejunectomy | Carcinoma of the splenic flexure of colon with metastasizing to liver and jejunum, |
| 17 | Left hemicolectomy | 2Carcinoma of the sigmoid with metastasizing to left ureter and common iliac artery |
| 18-19 | Ileocecectomy | 1Carcinoma of the terminal ileum with ileus, multiple diverticulosis of the ileocecum and chronic appendicitis |
| 20-21 | Splenectomy | Idiopathic thrombocytopenic purpura, carcinoma of pancreatic body and tail |
| 22-25 | Subtotal gastrectomy | Duodenal ulcer (2), gastric ulcer, gastric ulcer with massive hemorrhage |
| 26 | Half gastrectomy + cholecystectomy | Diverticulitis of duodenum and gall stone |
The location of HandPort device was preferred to be directly over or close to the main (core) vessels of the target organ, in order to provide direct visualization to transect the core vessels or dissect the radical lymph notes. The location of ports and positioning of the operator are listed in Table 2.
| Operations | HandPort | Camera1 | Scalpel1 | Operator2 |
| Left hepatic lateral segmentectomy | R upper transrectus3 | Umbilicus | L upper quadrant | R |
| Right hepatic segmentectomy | R pararectus abdominis | Umbilicus | L upper quadrant | R |
| Deroofing of the hepatic huge cyst | R subcosta | Umbilicus | L upper quadrant | L |
| R upper transrectus | Umbilicus | L upper quadrant | L | |
| R pararectus abdominis | Umbilicus | L upper quadrant | R | |
| Splenectomy | Upper midline4 | Umbilicus | L umbilicus level | R |
| L upper transrectus | Umbilicus | L lower umbilicus level | R | |
| Right hemicolectomy | Upper midline | Umbilicus | Lower midline | R |
| Left hemicolectomy + partial jejunectomy | Upper midline | Umbilicus | Lower midline | R |
| Subtotal gastrectomy | Upper midline | Umbilicus | L lower umbilicus level | R |
| Half gastrectomy +cholecystectomy | Upper midline | Umbilicus | R lower umbilicus level | R |
| Ileocecectomy | Lower midline3 | Umbilicus | R middle quadrant | L |
A 5-6 cm abdominal incision was performed, before placement of HandPort device to allow for introduction of the hand to assist in placing two trocars, similar to placement of abdominal drains in open surgery, and also to allow the hands to perform abdominal exploration. If the dissection preceded the resection, the following procedures were done under direct vision, including mobilizing intraperitoneal adhesion, dissecting the peripheral structures, or placing a loop for occlusion of hepatic hilar pedicles, in case of emergency use.
The HandPort device was placed, with the abdomen insufflated under a pressure of 13-14 mmHg. The left hand was reintroduced. While exposing and retracting or pulling tissues with the hand, the peripheral structures including adhesions, peritoneum, ligaments, omentum, mesentery, as well as the hepatic parenchyma around the “core” pedicles were dissected by harmonic scalpel or Ligasure, occasionally by combined use of electrocoagulation without any laparoscopic suture or ligation.
Once the target organ was mobilized, its core vessels were treated openly through the port incision by conventional open technique or vascular endo-stapler, as the location of the port incision was most direct over or close to the core vessels of the target organ.
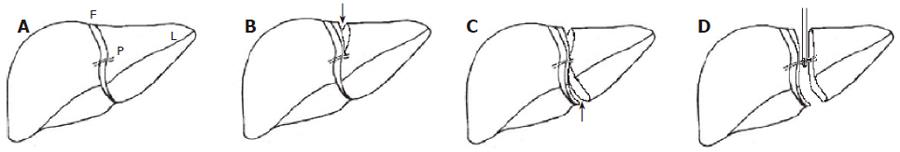
Among our patients, a 71 year-old woman suffered from hepatitis B-related cirrhosis supervened HCC and arrhythmia. She had had an open partial gastrectomy 5 years ago due to leiomyoma of stomach. She underwent hand-assisted laparoscopic left lateral segmentectomy. The HandPort incision of 6 cm in length was located at the previous wound scar at the right upper transrectus abdominis (the previous incision of 18 cm in length). The strategy of the procedure was to treat the portal pedicles of the left lateral segment as core vessels. First, the adhesions between wound peritoneum and omentum, liver and stomach were dissected. A loop was then placed around hepatic hilar pedicles, in case of requiring interrupting hepatic afferent blood flow. Two trocars for camera and harmonic scalpel were introduced by the open method of making abdominal drains. Following placement of HandPort system, the left hand was reintroduced and the target segment retracted. Ligament attachments of the left lobe were divided until the left lateral segment was completely freed, as shown in Figure 1A. The peripheral parenchyma around the core vessels was dissected from top toward bottom down to the core vessels (portal pedicles) with a harmonic scalpel (HCS 15 from Ethicon, Cincinati) (Figure 1B). Then, dissection switched from the bottom toward top up to the core vessels. The core vessels were completely freed (Figure 1C). Finally, the core vessels were transected by a vascular endo-stapler through the port incision openly (Figure 1D). The resected specimen was extracted immediately. There was no active blood oozing from the resected raw surface of the liver, which was covered with absorbable hemostasis gauze. The blood loss was less than 60 mL, without temporary inflow occlusion during operation. There was no need for abdominal drain. The resected left lateral segment was 15 cm × 8 cm × 4 cm.
Twenty-six patients underwent uneventful operation courses. One patient was converted to open procedure because his left ureter and common iliac artery were invaded by the sigmoid cancer. The conversion rate was 3.8% (1/26). The length of the procedures was under 2 hours (range 30 min-2 h). The operative blood loss was between 8 to 120 mL. There were no postoperative complications except that a 70 year-old man with chronic pulmonary emphysema and carcinoma of ascending colon, who underwent hand-assisted laparoscopic right hemicolectomy, developed 2 split stitches at the wound because of a violent cough on the 2nd postoperative day, and another patient had a wound stitch reaction. After operation, all patients felt less pain, resumed earlier oral intake of food, and faster recovery, compared with 25 consecutive corresponding cases of conventional surgery. The data are summarized in Tables 3 and 4.
| Cases | Operations | Indications |
| 1-2 | Left lateral segmentectomy | Hepatitis B-related cirrhosis supervened HCC, hepatic cavernous hemangioma |
| 3-6 | Deroofing of the hepatic huge cysts | Right hepatic huge cysts (4) |
| 7-8 | Hepatic S 5 and 6 segmentectomy | Hepatic cavernous hemangioma, hepatitis B-related cirrhosis supervened HCC |
| 9-10 | Hepatic S 6 segmentectomy | Hepatitis B-related cirrhosis supervened HCC, hepatic cavernous hemangioma |
| 11 | Hepatic S 5 segmentectomy + cholecystectomy | Hepatitis B-related cirrhosis supervened HCC |
| 12-13 | Splenectomy | Splenic infarction, splenic cysts |
| 14-17 | Right hemicolectomy | Carcinoma of the ascending colon (3), multiple polyps of ascending colon |
| 18 | Left hemicolectomy | Carcinoma of the descending colon |
| 19-20 | Ileocecectomy | Carcinoma of the terminal ileum, multiple diverticulosis |
| 21-25 | Subtotal gastrectomy | Duodenal ulcer(2), 1gastric ulcer with bleeding, gastric ulcer, diverticulitis of duodenum with bleeding |
Compared with full minimal laparoscopic large organ resection, an incision is often required for extraction of the resected specimen. In fact, there are often “1 port + more than 2 trocars” abdominal wounds in full minimal laparoscopic large viscera resection. By use of currently available tools including HandPort system, harmonic scalpel, Ligasure[6], we designed “1 port + 2 trocars” specific HALS for safe and quick resection of large abdominal visceral organs.
This technique can be of real significance in avoidance of vascular bleeding during removal of the target organ, because the final step is transection of the core vessels. There is no need for worrying about bleeding as the staplers are taken off. Furthermore, a hand inside the abdomen can play an important role in preventing or controlling bleeding. On the contrary, for total laparoscopic operation, which were several times higher in blood loss and longer in operative time, the unmanageable bleeding has become the main cause to convert to open surgery. Total laparoscopic operation does not equal to the minimally invasive surgery. The minimally invasive surgery presents not only the minimal abdominal wound, but also the minimal surgical intervention and complications including bleeding, injury to major adjacent structures, conversion to open surgery and operative time. The technique we employed is by all means the small ports to accomplish the big organ resection with minimal surgical stress, better hemostasis and shorter operative time, and faster recovery of the patients.
Hand-assisted laparoscopic hemicolectomy by this technique is presumed to be an excellent approach combining advantages of laparoscopic and open surgeries. The procedure includes: (1) Laparoscopically, the distal peripheral structures are mobilized by harmonic scalpel or Ligasure with hand-assistance; (2) Conventionally, the mobilized target colon is long enough to be extracted through the optimal base retractor of HandPort system, through which the major core vessel pedicles are transected, or the radical lymph nodes are dissected under direct vision, then the specimen is removed and delivered to prevent port side “seeding”; (3) Extracorporeally, end to end coloileostomy or colocolostomy is performed by sutureless biofragmentable anastomosis ring (BAR), or single layer anastomosis.
In our series, the HALS wound length of 5-6 cm (mean 5.3 cm) was much shorter than the open surgical wound length of 16-33 cm (mean 22.5 cm). Other studies have reported full laparoscopic wound length of 8.5 cm[7]. The operative time in our group was under 2 h. In addition, previous studies revealed mean operative times for full laparoscopic colectomy, converted procedures, right, and sigmoid resection were 164, 203, 121 and 177 min, respectively[8].
Our specifically designed HALS in splenectomy has advantage over total laparoscopic splenectomy. First, through the small incision port, the gastrosplenic ligament was dissected as much as possible by open technique before pneumoperitoneum. Second, after placement of the HandPort device, a hand into the abdomen assisted harmonic scalpel or Ligasure to dissect the rest ligaments. It seemed the spleen was retracted by hand with more safety. It also provided better exposure, easier and faster performance than other instruments. Third, splenic pedicle was transected by endo-stapler laparoscopically, or through the small incision with open visualization. Lastly, the resected specimen was extracted immediately after removal of the spleen. However, in full laparoscopic splenectomy with about 4 trocars, the specimen is bagged, one port incision is extended, and the spleen is broken into pieces, and then delivered.
Our study demonstrates HALS in resection of the segments lying at outer edge of the liver (segments 2 to 6) can be performed with ease, safety and rapidity. Placement of the hand into the abdomen plays an important role, because there is no ideal instrument available for grasping the liver but the hand, which acts as a comparatively atraumatic grasping clamp and retractor providing good exposure, and also allows for fingers to identify major pedicles after finishing parenchymal division with Ligasure or harmonic scalpel. The major pedicles are transected using vascular endo-stapler under direct vision through the small incision, and the specimen is delivered at once without breaking.
First, the greater and lesser omentum are dissected using this technique much easier and quicker. Second, the stomach is transected and gastrojejunostomy is performed by using open staplers, which are much easier, quicker, more reliable, and less expensive than using endo-staplers in full laparoscopic subtotal gastrectomy. Third, a big and hard duodenal ulcer like the one in our cases is not the indication for full laparoscopic technique, because such duodenal ulcer can neither be transected, nor can the stump be closed with staplers.
The design of the approach for HALS in resection of abdominal large viscera is based on the minimal abdominal wound “1 port + 2 trocars”, as well as the minimal surgical intervention, combining the laparoscopic benefits with the advantages of a conventional open technique. Even though the target organs include parenchymatous and hollow viscera, the rules of resection are the same, which allow for first dissecting the peripheral structures, and finally transecting the core vessel pedicles. This technique is minimal in access, safe, and rapid in laparoscopic resection of abdominal large viscera.
S- Editor Wang J L- Editor Zhu LH E- Editor Liu WF
| 1. | Perissat J, Vitale GC. Laparoscopic cholecystectomy: gateway to the future. Am J Surg. 1991;161:408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Tuech JJ, Pessaux P, Regenet N, Rouge C, Hennekinne S, Bergamaschi R, Arnaud JP. Laparoscopic colectomy for sigmoid diverticulitis: a prospective study in the elderly. Hepatogastroenterology. 2001;48:1045-1047. [PubMed] |
| 3. | Kusminsky RE, Boland JP, Tiley EH, Deluca JA. Hand-assisted laparoscopic splenectomy. Surg Laparosc Endosc. 1995;5:463-467. [PubMed] |
| 4. | Kusminsky RE, Boland JP, Tiley EH. Hand-assisted laparoscopic surgery. Dis Colon Rectum. 1996;39:111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Litwin DE, Darzi A, Jakimowicz J, Kelly JJ, Arvidsson D, Hansen P, Callery MP, Denis R, Fowler DL, Medich DS. Hand-assisted laparoscopic surgery (HALS) with the HandPort system: initial experience with 68 patients. Ann Surg. 2000;231:715-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 123] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Msika S, Deroide G, Kianmanesh R, Iannelli A, Hay JM, Fingerhut A, Flamant Y. Harmonic scalpel in laparoscopic colorectal surgery. Dis Colon Rectum. 2001;44:432-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Brown SR, Eu KW, Seow-Choen F. Consecutive series of laparoscopic-assisted vs. minilaparotomy restorative proctocolectomies. Dis Colon Rectum. 2001;44:397-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Lauter DM, Froines EJ. Initial experience with 150 cases of laparoscopic assisted colectomy. Am J Surg. 2001;181:398-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |