Published online Jul 28, 2006. doi: 10.3748/wjg.v12.i28.4588
Revised: March 1, 2006
Accepted: April 21, 2006
Published online: July 28, 2006
Leiomyomas are the most common benign tumors of the esophagus. They usually occur as a single lesion or as two or three nodules. Only two cases of esophageal multiple leiomyomas comprising more than 10 nodules have been reported previously. Moreover, there have been few reports of esophageal squamous cell carcinoma overlying submucosal tumors. We describe a 71-year-old man who was diagnosed as having a superficial esophageal cancer coexisting with two or three leiomyoma nodules. During surgery, 10 or more nodules that had not been evident preoperatively were palpable in the submucosal and muscular layers throughout the esophagus. As intramural metastasis of the esophageal cancer was suspected, we considered additional lymphadenectomy, but had to rule out this option because of the patient’s severe anoxemia. Microscopic examination revealed that all the nodules were leiomyomas (20 lesions, up to 3 cm in diameter), and that invasion of the carcinoma cells was limited to the submucosal layer overlying a relatively large leiomyoma. This is the first report of superficial esophageal cancer coexisting with numerous solitary leiomyomas. Multiple minute leiomyomas are often misdiagnosed as intramural metastasis, and a leiomyoma at the base of a carcinoma lesion can also be misdiagnosed as tumor invasion. The present case shows that accurate diagnosis is required for the management of patients with coexisting superficial esophageal cancer and multiple leiomyomas.
- Citation: Iwaya T, Maesawa C, Uesugi N, Kimura T, Ikeda K, Kimura Y, Mitomo S, Ishida K, Sato N, Wakabayashi G. Coexistence of esophageal superficial carcinoma and multiple leiomyomas: A case report. World J Gastroenterol 2006; 12(28): 4588-4592
- URL: https://www.wjgnet.com/1007-9327/full/v12/i28/4588.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i28.4588
Leiomyomas are the most common benign tumors of the esophagus, accounting for roughly two-thirds of all benign tumors of this organ. Although its overall incidence reported in autopsy ranges from 0.005% to 5%,[1,2] this may be an underestimation because many small lesions are missed at autopsy unless the esophagus is examined carefully. Studies involving detailed histological examinations have reported the frequency to be higher, at 7.9%[3]. Since esophageal leiomyomas are generally slow-growing and the size of tumors may not change for many years, most affected patients are asymptomatic. Considering the risk of surgery and the patient’s quality of life, non-surgical management is recommended.
Surgical resection of esophageal leiomyomas is warranted only when: (1) there is severe dysphagia due to giant or multiple lesions, (2) there is a possibility of symptomatic transformation, (3) there is a need to obtain a definitive histological diagnosis, (4) malignancy can only be ruled out by surgical removal, or (5) malignant epithelial tumors are also present.
Both giant and multiple lesions involving the entire esophagus can cause severe and debilitating dysphagia. The presence of a giant lesion itself is a risk factor for malignancy, and such lesions should be treated surgically even if they cause no symptoms. Otherwise, esophageal leiomyoma usually appears as a solitary tumor (97%). Occasionally (less than 2.4% of all cases), more than one esophageal leiomyoma; i.e., generally two or three, may occur in the same patient. Multiple leiomyomas of the esophagus are extremely rare, and only two such cases, involving more than 10 nodules, have been reported previously[4,5]. Diagnosis of medium-sized leiomyomas is generally easy using endoscopic ultrasonography (EUS) and computerized tomography (CT). However, this is difficult when multiple leiomyomas coexist with carcinoma lesions. In cases where carcinoma overlies a submucosal leiomyoma, there is a possibility of overestimating the extent of tumor invasion, and multiple minute leiomyomas are sometimes misdiagnosed as intramural metastasis.
Here, we describe a case of superficial esophageal squamous cell carcinoma (SCC) coexisting with multiple (more than 20) leiomyoma lesions, and we discuss the management of such patients and the histogenesis of carcinomas overlying esophageal submucosal tumors (SMT).
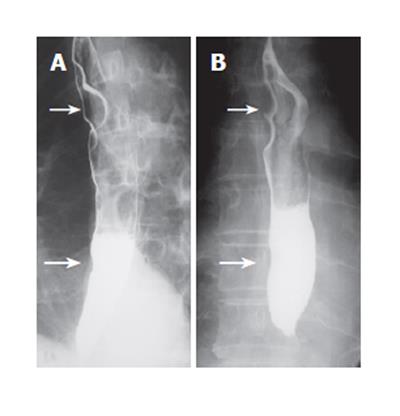
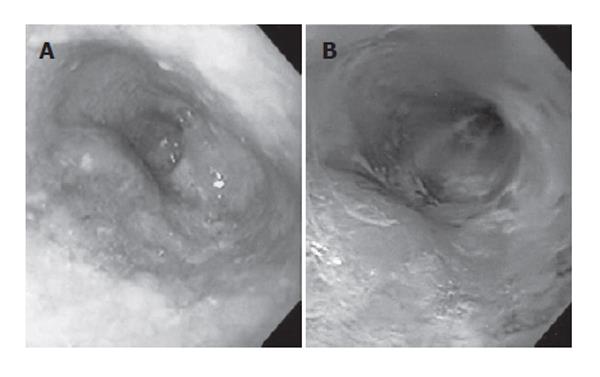
The patient is a 71-year-old man who presented with a cervical tumor in October 2000. He was diagnosed as having a malignant lymphoma of the thyroid and esophageal leiomyomas. The thyroid tumor disappeared completely after chemotherapy, and the patient maintained a status of complete remission. Barium swallow esophagograms showed two smoothly rounded defects. The larger tumor, 40 mm in diameter and exhibiting two or three bumps, was located in the middle third of the esophagus. The smaller one, 20 mm in diameter, was in the lower third of the esophagus (Figure 1A). Both tumors were covered by normal mucosa, and showed no signs of malignancy in CT and EUS examinations. Therefore, we diagnosed these SMTs as two (or possibly three) leiomyomas. One year later, in December 2001, no marked changes were evident in a barium swallow examination (Figure 1B). However, endoscopy revealed a superficial ulcerative tumor (24 mm in diameter) in the lower third of the esophagus, overlying the smaller SMT (Figure 2: Left). Chromoendoscopy with Lugol’s iodine solution demonstrated that the polypoid lesion was located within the non-staining area and that part of the surface was covered by normal mucosa (Figure 2: Right). Multiple biopsies revealed that the ulcerative tumor was SCC. EUS demonstrated that the cancer overlaid one of the leiomyomas, originating in the muscular layer, suggesting that the cancer may have invaded only as far as the submucosal layer. In February 2002, the patient underwent esophagectomy with a gastric pull-up reconstruction and cervical anastomosis via abdominal, left cervical and right thoracotomy incisions at the Department of Surgery I, Iwate Medical University School of Medicine, Morioka, Japan. During the operation, 10 or more nodules that had not been evident preoperatively were palpable in the submucosal and muscular layers throughout the esophagus. Intramural metastasis of the esophageal cancer was therefore suspected, and additional lymphadenectomy was considered. However, this option was ruled out because of the patient’s severe anoxemia.
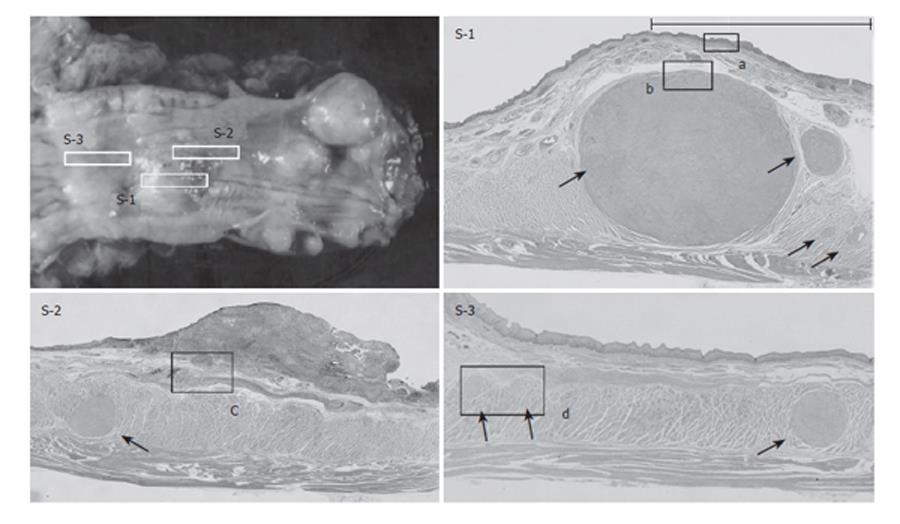
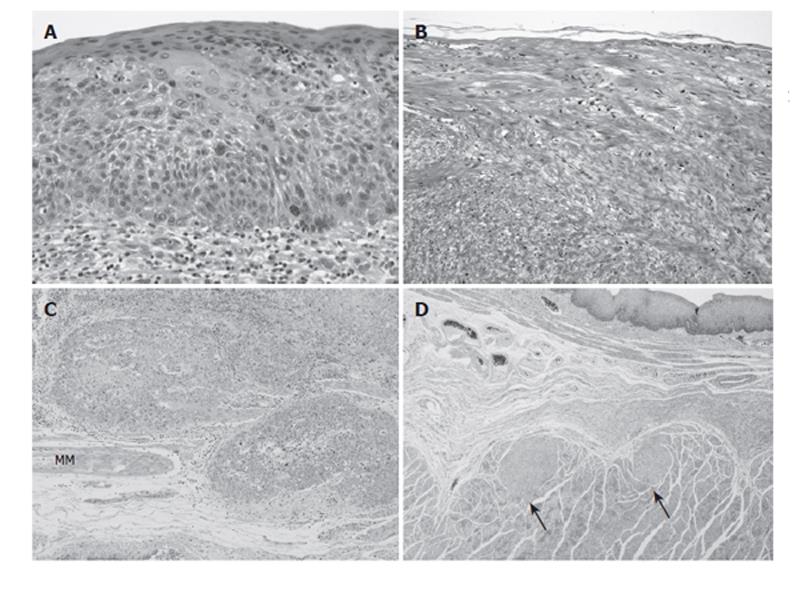
The resected specimen showed a superficial ulcerative tumor and multiple SMTs of various sizes (Figure 3). Macroscopically, about 10 SMTs were evident throughout the esophagus. Each SMT appeared as a well demarcated round nodule, and none of the tumors showed continuity with others, which is a characteristic feature of leiomyomatosis. Microscopically, more than 20 SMTs, measuring from 1 mm to 3 cm in diameter, were scattered throughout the esophagus (Figures 4 and 5: Arrows). All the SMTs showed low overall cellularity, and were composed of interlaced smooth-muscle cells with hypovascularity and no mitosis (Figure 5B). These findings are characteristic of leiomyoma. The ulcerative tumor overlaid one of the leiomyoma nodules in the lower third of the esophagus. The tumor was confirmed as SCC, and extensive carcinoma in situ (CIS) was observed on the leiomyoma (Figures 4(S-1) and 5A). On the oral side of the SMT, the cancer had invaded into the submucosal layer, without lymph node metastasis (Figures 4(S-2) and 5C).
The patient was discharged one month after the operation. At the time of writing, three years later, no local recurrence or distant metastasis of the SCC or malignant lymphoma has been observed.
As a distinct entity, multiple leiomyoma of the esophagus involving solitary lesions needs to be clearly distinguished from diffuse leiomyomatosis. Multiple leiomyoma of the esophagus is extremely rare, and only two such cases, involving more than 10 lesions, have been reported previously[4,5]. Bradford et al reported a patient with 14 esophageal leiomyomas measuring 1 to 4 cm in diameter, and Seremetis et al reported another patient who had 15 such leiomyomas 0.4 to 6 cm in diameter. In our patient, more than 20 leiomyomas, measuring from 1 mm to 3 cm in diameter, were scattered throughout the esophagus.
There have been several reports of esophageal SCC coexisting with benign SMT[6-14]. This presentation shows two types: one is the overlying type, where the carcinoma covers the benign SMT, and in the other type the two lesions are separate. Generally, most SMTs in the separate type are minute leiomyomas that are discovered only during postoperative examination of pathology specimens[3]. This type of presentation is often encountered during esophagectomy for esophageal SCC. Otherwise, twelve cases of the overlying type have been reported previously[6-14] and are summarized in Table 1. Although benign tumors of various sizes have been reported, all of them protruded into the esophageal lumen. Some investigators have speculated that the pathogenesis of the overlying type may involve chronic irritation of the esophageal mucosa, due to intraluminal protrusion of the SMT, leading to carcinoma development[9-11]. This hypothesis has been suggested in reports of SCC coexisting with lipomas as well as leiomyomas[15]. In the present patient, both overlying and separate types were observed. Although there were 20 leiomyomas scattered throughout the esophagus, the SCC overlaid a relatively large and protruding tumor. Thus, the size and location of SMTs might affect the degree to which the esophageal mucosa is exposed to chronic irritation.
| Authors | Age | Sex | Submucosal tumor(SMT) | Size of SMT (cm) | Depth of cancer invasion | Subviews and <Management> | |
| 1 | Marcial-Rojas RA | 63 | Male | Lipoma | 11 × 3.5 | Mucosal layer | <Cervical esophagotomy, excision> |
| 2 | Iizuka et al | 75 | Male | Leiomyoma | 3.0 × 2.0 | Mucosal layer | <Blunt dissection> |
| 3 | Watanabe et al | 53 | Male | Leiomyoma | 0.8 × 0.6 × 0.25 | Intraepithelium | Dysplasia <Chemotherapy,esophagectomy> |
| 4 | Callanan et al | 54 | Male | Leiomyoma | 1.25 | Muscular layer | <Esophagectomy> |
| 5 | Kuwano et al | 45 | Male | Leiomyoma | 4 | Muscular layer | <Esophagectomy> |
| 6 | 63 | Male | Leiomyoma | 1 | Mucosal layer | Dysplasia <Esophagectomy> | |
| 7 | 71 | Male | Lipoma | 1.5 | Mucosal layer | <Esophagectomy> | |
| 8 | Yosikane et al | 52 | Male | Leiomyoma | 1.5 × 1.1 × 0.7 | Mucosal layer | CIS and dysplasia <Esophagectomy> |
| 9 | 67 | Male | Lipoma | 2.8 × 4.5 | Intraepithelium | Separate cancer <Esophagectomy> | |
| 10 | Nagashima et al | 61 | Male | Leiomyoma | 2.9 × 2.0 | Lamina propria | <Endoscopic resection> |
| 11 | Mizobuchi et al | 64 | Male | Leiomyoma | 0.7 × 0.65 | Lamina propria | <Esophagectomy> |
| 12 | Fu et al | 62 | Male | Leiomyoma | 2 | Mucosal layer | <Endoscopic resection> |
| 13 | Present case | 73 | Male | Leiomyoma | 2.0 × 1.5 | Submucosal layer | Multiple leiomyomas <Esophagectomy> |
Recently, curative endoscopic resection has been performed for patients with carcinomas overlying SMTs. However, such cases require accurate diagnosis of the depth of invasion using EUS[7,8]. Mizobuchi et al reported a case in which an early esophageal SCC was overdiagnosed because the leiomyoma appeared to be a component of the carcinoma[6]. In these reports, the authors emphasized that accurate diagnosis of the leiomyoma made it possible to avoid excessive surgery. Several diagnostic modalities, such as ballium swallow, endoscopy, CT and EUS, allow esophageal leiomyoma to be diagnosed effectively, and most of them have been monitored[16]. With these examinations, however, small leiomyomas are often difficult to diagnose. Indeed, as in the present case, a number of small SMTs may not be apparent preoperatively. During surgery, we were unable to completely rule out the possibility that some of the SMTs were intramural metastases of the ESC, as multiple leiomyoma of the esophagus is quite rare and intramural metastasis of esophageal superficial carcinoma is relatively common.
Since many coexisting carcinomas reported previously have been superficial, it has been speculated that the coexisting SMT may in fact inhibit the growth and invasion of the carcinoma[10]. In the present case, the overlying SCC had invaded only as far as the mucosal layer, and submucosal invasion was limited to only a very narrow region where the SMT was absent. This case appears to support the speculation that SMT inhibits the growth of SCC. During the operation, lymphadenectomy was ruled out because of the patient’s anoxemia. If conditions had been more favorable, the patient might have undergone more aggressive surgery. Therefore, in cases where a coexisting superficial carcinoma overlies a benign SMT, a more noninvasive therapeutic procedure (EMR, thoracoscopic approach, and omission of lymphadenectomy etc.) should be chosen.
S- Editor Wang J L- Editor Lutze M E- Editor Liu WF
| 1. | Kramer MD, Gibb SP, Ellis FH Jr. Giant leiomyoma of esophagus. J Surg Oncol. 1986;33:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Postlethwait RW, Musser AW. Changes in the esophagus in 1,000 autopsy specimens. J Thorac Cardiovasc Surg. 1974;68:953-956. [PubMed] |
| 3. | Takubo K, Nakagawa H, Tsuchiya S, Mitomo Y, Sasajima K, Shirota A. Seedling leiomyoma of the esophagus and esophagogastric junction zone. Hum Pathol. 1981;12:1006-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Seremetis MG, Lyons WS, deGuzman VC, Peabody JW Jr. Leiomyomata of the esophagus. An analysis of 838 cases. Cancer. 1976;38:2166-2177. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Bradford ML, Mahon HW, Grow JB. Mediastinal cysts and tumors. Surg Gynecol Obstet. 1947;85:467-491. [PubMed] |
| 6. | Mizobuchi S, Kuge K, Matsumoto Y, Yokoyama Y, Ookawauchi K, Tamura S, Kurabayashi A, Sasaguri S. Co-existence of early esophageal carcinoma and leiomyoma: a case report. Jpn J Clin Oncol. 2004;34:751-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Fu KI, Muto M, Mera K, Sano Y, Nagashima F, Tahara M, Boku N, Ohtsu A, Kanomata N, Ochiai A. Carcinoma coexisting with esophageal leiomyoma. Gastrointest Endosc. 2002;56:272-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Nagashima R, Takeda H, Motoyama T, Tsukamoto O, Takahashi T. Coexistence of superficial esophageal carcinoma and leiomyoma: case report of an endoscopic resection. Endoscopy. 1997;29:683-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Kuwano H, Sadanaga N, Watanabe M, Yasuda M, Nozoe T, Sugimachi K. Esophageal squamous cell carcinoma occurring in the surface epithelium over a benign tumor. J Surg Oncol. 1995;59:268-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Yoshikane H, Tsukamoto Y, Niwa Y, Goto H, Hase S, Maruta S, Shimodaira M, Miyata A. The coexistence of esophageal submucosal tumor and carcinoma. Endoscopy. 1995;27:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Watanabe M, Baba T, Hotchi M. A case of leiomyoma of the lamina muscularis mucosae of the esophagus with a complication of carcinoma in situ of the overlying mucosa. Acta Pathol Jpn. 1987;37:1845-1851. [PubMed] |
| 12. | Iizuka T, Kato H, Watanabe H, Itabashi M, Hirota T. Superficial carcinoma of the esophagus coexisting with esophageal leiomyoma: a case report and review of the Japanese literature. Jpn J Clin Oncol. 1984;14:115-122. [PubMed] |
| 13. | MARCIAL-ROJAS RA. Epidermoid carcinoma in mucosa overlying a pedunculated lipoma of the esophagus. J Thorac Surg. 1959;37:427-434. [PubMed] |
| 14. | Callanan JG. Simultaneous occurrence of simple and malignant tumors in the esophagus. J Thorac Surg. 1954;28:4-10. [PubMed] |
| 15. | Zschiedrich M, Neuhaus P. Pedunculated giant lipoma of the esophagus. Am J Gastroenterol. 1990;85:1614-1616. [PubMed] |
| 16. | Lee LS, Singhal S, Brinster CJ, Marshall B, Kochman ML, Kaiser LR, Kucharczuk JC. Current management of esophageal leiomyoma. J Am Coll Surg. 2004;198:136-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |