Published online Jul 21, 2006. doi: 10.3748/wjg.v12.i27.4428
Revised: March 8, 2006
Accepted: March 27, 2006
Published online: July 21, 2006
This article reports the case of a 34-year-old woman with xanthogranulomatous cholangitis who developed obstructive jaundice. Microscopically, the bile duct was surrounded and narrowed by a xanthogranulomatous lesion, but no xanthogranulomatous cholecystitis was seen. Although percutaneous cholangiograms done via the transhepatic biliary drainage showed smooth narrowing of the upper to middle bile duct, the cytology of bile was diagnosed as class V adenocarcinoma. Therefore, right extended hepatectomy and extrahepatic bile duct resection were performed. The differentiation of benign and malignant strictures at the hepatic hilum is often difficult. Xanthogranulomatous cholangitis is one possible diagnosis of a bile duct stricture. Precise review of all the preoperative information is required to make a correct diagnosis.
- Citation: Kawate S, Ohwada S, Ikota H, Hamada K, Kashiwabara K, Morishita Y. Xanthogranulomatous cholangitis causing obstructive jaundice: A case report. World J Gastroenterol 2006; 12(27): 4428-4430
- URL: https://www.wjgnet.com/1007-9327/full/v12/i27/4428.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i27.4428
The differential diagnosis of bile duct strictures at the hepatic hilum is often difficult. When computed tomograms or magnetic resonance imaging show an invasive tumor around the bile duct, the tumor should be diagnosed as malignant. The correct diagnosis is difficult when there is a discrepancy between the imaging and cytologic diagnosis. The sensitivity of bile cytology to detect malignancy is too low to make a conclusive diagnosis. We present a case of bile duct stricture due to xanthogranulomatous cholangitis where a cytological diagnosis of class V adenocarcinoma was made preoperatively. Microscopically, the bile duct was surrounded and narrowed by a xanthogranulomatous lesion, but no xanthogranulomatous cholecystitis (XGC) was seen.
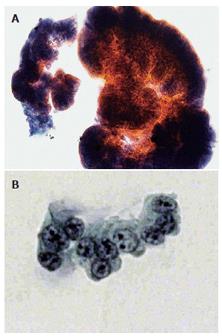
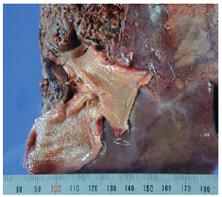
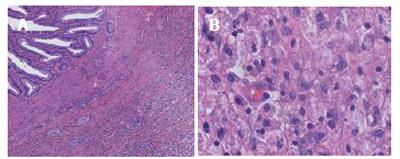
A 34-year-old woman visited a neighborhood doctor because of jaundice in January 2003. The serum total bilirubin concentration was 7.5 mg/dL. The serum alkaline phosphatase and γ-glutamyltranspeptidase concentrations were 1588 IU/L and 286 IU/L, respectively. There was no leukocytosis. The serum carcinoembryonic antigen, carbohydrate antigen 19-9, and α-fetoprotein levels were within normal limits. Percutaneous transhepatic cholangiodrainage (PTCD) was performed. The cholangiogram showed smooth stenosis of the common bile duct and both hepatic ducts (Figure 1). Bile cytology specimens from the PTCD revealed some cohesive groups of columnar cells with partial papillary growth (Figure 2A). The nucleocytoplasmic ratio was increased and variously sized round nuclei with granular chromatin and prominent nucleoli were observed (Figure 2B). The cytology of the bile was diagnosed as class V adenocarcinoma. She was transferred to our hospital for surgical treatment in February 2003. Computed tomograms of the abdomen demonstrated ascites, but no tumor mass was detected around the bile duct. A diagnostic laparoscopic examination revealed no peritoneal deposits. After percutaneous transhepatic embolization of the right portal vein, extended right hepatectomy and extrahepatic bile duct resection were performed. On inspection, the resected specimen showed wall thickening of the biliary tree from the hepatic duct to the common bile duct. However, the surface mucosa of the extrahepatic bile duct and gallbladder was smooth with no evident neoplastic change. Neither gallstones nor biliary sludge were seen. The cut surface of the bile duct showed a yellowish xanthomatous lesion expanding from the lamina propria toward the serosa (Figure 3). Microscopically, there was fibrous thickening and marked infiltration of foamy macrophages, lymphocytes, plasma cells, and eosinophils in the lamina propria of the bile duct mucosa (Figure 4). These fibrotic, inflammatory, and xanthogranulomatous changes were localized to the extrahepatic bile duct sparing the gallbladder, and resulted in luminal narrowing of the bile duct. The gallbladder showed mild infiltration of lymphocytes and plasma cells, thickening of the smooth muscle layer, and edema of the subserosa. Although the surface epithelia of the bile duct showed some hyperplastic features, namely increased luminal folds, no significant structural or cellular atypia were noted. A diagnosis of xanthogranulomatous cholangitis without cholecystitis was made.
XGC is a relatively rare inflammatory disease of the gallbladder. Xanthogranulomatous cholangitis is rare, though there are some reports of bile duct stenosis due to extension of XGC[1,2]. The pathogenesis of XGC remains elusive; cystic duct obstruction with gallstones and bile stasis are thought to be important etiologic factors[3,4]. In our case, there was no stone in the gallbladder or the bile duct, and XGC was never seen microscopically, although mild inflammation was seen in the gallbladder. Therefore, the cause of the xanthogranulomatous cholangitis in this case remains unclear.
The manifestations of this case were similar to those of other causes of bile duct stricture, and must be distinguished from gallstone disease, bile duct carcinoma, and primary sclerosing cholangitis (PSC). It is not known whether XGC and gallbladder carcinoma are associated; some authors have indicated an association, and it can be difficult to differentiate XGC from gallbladder carcinoma[5,6]. We initially suspected that the bile stricture was PSC or a submucosal lesion like a MALToma, based on the smooth stricture of the bile duct seen in the cholangiograms. However, we diagnosed the bile duct stricture as malignant adenocarcinoma because repeated bile duct cytology was class V adenocarcinoma. Two prospective studies of the bile cytology of biliary stritures have shown that the accuracy of brush cytology for cholangiocarcinoma is approximately 60%[7,8]. In addition, Gerhards et al reported a false-positive diagnosis of malignancy resulted in a 15% resection rate for benign hilar strictures. They concluded that resection of a benign lesion mimicking a malignant stricture at the proximal bile duct could not be avoided[9].
Xanthogranulomatous cholangitis is included in the differential diagnosis of benign and malignant strictures at the hepatic hilum. Precise reviews of all available findings are required to make the correct diagnosis. Finally, the surgeons must know that the bile cytologic diagnosis is sometimes falsely positive for malignancy.
S- Editor Wang J L- Editor Misra SP E- Editor Liu Y
| 1. | Kawana T, Suita S, Arima T, Hirayama Y, Ishii K, Minamishima I, Ueda K, Hirata T, Nagoshi M, Enjoji M. Xanthogranulomatous cholecystitis in an infant with obstructive jaundice. Eur J Pediatr. 1990;149:765-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Prasil P, Cayer S, Lemay M, Pelletier L, Cloutier R, Leclerc S. Juvenile xanthogranuloma presenting as obstructive jaundice. J Pediatr Surg. 1999;34:1072-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Benbow EW. Xanthogranulomatous cholecystitis. Br J Surg. 1990;77:255-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Dixit VK, Prakash A, Gupta A, Pandey M, Gautam A, Kumar M, Shukla VK. Xanthogranulomatous cholecystitis. Dig Dis Sci. 1998;43:940-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Enomoto T, Todoroki T, Koike N, Kawamoto T, Matsumoto H. Xanthogranulomatous cholecystitis mimicking stage IV gallbladder cancer. Hepatogastroenterology. 2003;50:1255-1258. [PubMed] |
| 6. | Maeda T, Shimada M, Matsumata T, Adachi E, Taketomi A, Tashiro Y, Tsuneyoshi M, Sueishi K, Sugimachi K. Xanthogranulomatous cholecystitis masquerading as gallbladder carcinoma. Am J Gastroenterol. 1994;89:628-630. [PubMed] |
| 7. | Mansfield JC, Griffin SM, Wadehra V, Matthewson K. A prospective evaluation of cytology from biliary strictures. Gut. 1997;40:671-677. [PubMed] |
| 8. | Kurzawinski TR, Deery A, Dooley JS, Dick R, Hobbs KE, Davidson BR. A prospective study of biliary cytology in 100 patients with bile duct strictures. Hepatology. 1993;18:1399-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 85] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Gerhards MF, Vos P, van Gulik TM, Rauws EA, Bosma A, Gouma DJ. Incidence of benign lesions in patients resected for suspicious hilar obstruction. Br J Surg. 2001;88:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 132] [Article Influence: 5.5] [Reference Citation Analysis (0)] |