Published online Jul 21, 2006. doi: 10.3748/wjg.v12.i27.4420
Revised: January 8, 2006
Accepted: January 9, 2006
Published online: July 21, 2006
AIM: To retrospectively evaluate the vaccination-induced anti-HBs seroconversion rates in treatment-naïve and treatment-experienced chronic hepatitis C (CHC) patients. Also to prospectively evaluate the seroconversion rates in CHC patients during pegylated interferon (PEG) plus ribavirin (RIB) treatment.
METHODS: Seventy treatment-naïve CHC patients (group A), 22 sustained virological responders-SVR following interferon (IFN) plus RIB treatment CHC patients (group B) and 121 healthy subjects (group C) had been participated in the same HBV vaccination schedule (20 μg, 0-1-6 mo). Seroconversion was considered if anti-HBs levels were above 10 mIU/mL within 3 mo following the third dose of the vaccine. Moreover, we prospectively selected 30 non-cirrhotic CHC patients and evaluated them for the efficacy of the same vaccine schedule randomizing them in two groups: Group-1, 15 CHC patients received the first dose of the vaccine in parallel with the initiation of PEG plus RIB treatment and Group-2, 15 patients received the same vaccination schedule without concomitant treatment. Determination of anti-HBs was performed at mo 1, 2, and 7. Statistical analysis of data was based on ANOVA student’s t-test and chi-square analysis (P < 0.05).
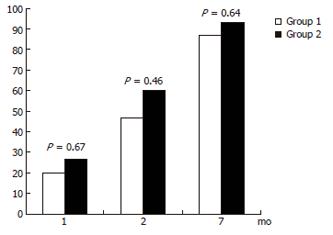
RESULTS: Fifty-eight of 70 group A patients (82.85%), 20/22 group B (90.9%) and 112/121 healthy subjects (92.56%) had been seroconverted. The seroconversion rates were significantly higher in the control group than in treatment-naïve CHC patients (P = 0.04). The corresponding rates were comparable between group A and group B CHC patients (P = 0.38). The vast majority of non-responders (10/14, 71.43%) had been infected by genotype-1 of HCV. The seroconversion rates were comparable between group 1 and 2 CHC patients at mo 1 (20% versus 26.7%, P = 0.67), mo 2 (46.7% vs 60%, P = 0.46) and mo 7 (86.7% versus 93.3%, P = 0.54) of follow-up.
CONCLUSION: The immunogenicity of HBV vaccine seems to be lower in CHC patients compared to healthy subjects. SVR following IFN plus RIB treatment does not affect the antibody response to HBV vaccine. Infection by genotype-1 seems to negatively influence the seroconversion rates. Vaccination against HBV during PEG plus RIB combination treatment is not beneficial in terms of anti-HBs seroconversion rates.
- Citation: Elefsiniotis IS, Vezali E, Kamposioras K, Pantazis KD, Tontorova R, Ketikoglou I, Moulakakis A, Saroglou G. Immunogenicity of recombinant hepatitis B vaccine in treatment-naïve and treatment-experienced chronic hepatitis C patients: The effect of pegylated interferon plus ribavirin treatment. World J Gastroenterol 2006; 12(27): 4420-4424
- URL: https://www.wjgnet.com/1007-9327/full/v12/i27/4420.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i27.4420
Hepatitis B virus (HBV) and hepatitis C virus (HCV) are two of the most common causes of chronic liver disease and hepatocellular carcinoma in the world. Both viral infections share many of the same routes of transmission, including parenteral exposure, promiscuous sex and vertical transmission[1,2,3]. HBV infection can be prevented by the administration of a safe and immunogenic vaccine[4,5,6] whereas no vaccine exists until now for HCV infection due to the high variability of the virus and its subsequent ability to escape immune surveillance.
Dual infection by HBV and HCV is clearly associated with more severe liver disease than infection by a single virus, whereas acute HBV infection in patients with chronic HCV-related liver disease is associated with a severe and often fulminant course of the disease[7,8,9]. Hepatitis B vaccination is recommended for patients with chronic HCV infection without immunity to HBV[10] in a cost-effectiveness approach[11]. Several studies suggest that the immunogenicity of recombinant hepatitis B vaccine is decreased in patients with chronic hepatitis C, compared to healthy controls[12,13], especially in those with advanced liver disease[14]. In only one study from Taiwan, was the antibody response to hepatitis B surface antigen (anti-HBs) similar in chronic hepatitis C patients and healthy subjects, who were both susceptible to HBV infection, after the first, second and third dose of the vaccine[15]. HCV viral load does not seem to correlate with the vaccination-induced anti-HBs response in chronic HCV infected patients vaccinated against HBV[12,13] whereas the main predictive factors for non-response to HBV vaccine seem to be age (> 50 years), body weight (> 75 kg) and the presence of cirrhosis[12,14]. The ideal time for HBV vaccination and the optimum HBV vaccination schedule (dose/interval) of chronic HCV infected patients have not been defined yet.
To our knowledge data about the impact of antiviral-immunomodulatory treatment against HCV infection on the safety and efficacy of the recombinant HBV vaccine are limited[16]. Moreover, there are no data about the impact of pegylated-interferon alpha (PEG-IFNα) plus ribavirin (RIB) treatment in the vaccination-induced anti-HBs response rates in chronic HCV infected patients. In our study we retrospectively evaluated the vaccination-induced anti-HBs response rates in treatment-naïve chronic HCV infected patients and in chronic HCV infected patients who exhibit sustained virological response after interferon-alpha plus ribavirin treatment, in comparison with healthy-HBV susceptible subjects vaccinated against hepatitis B with available data. The second aim of the study was to prospectively evaluate the vaccination-induced anti-HBs response rates in a group of chronic hepatitis C patients during PEG-IFNα plus RIB treatment in order to gain information about the optimum period of HBV vaccination.
The study was performed at the Hepatology Unit of Hippokration Hospital of Athens, Greece. In this study we retrospectively analyzed 92 patients with serologically, virologically and histologically confirmed chronic hepatitis C (CHC) and 121 healthy subjects, with available data from medical records between October 2000 and October 2004, for the immunogenicity of recombinant hepatitis B vaccine, at a regular dose (20 μg) and classical vaccination schedule (0, 1, 6 mo). Seventy CHC patients had never experienced treatment for hepatitis C before (group A) and 22 CHC patients of the study population had been treated with interferon-alpha plus ribavirin and they had been characterized as sustained virological responders (group B), according to virological data. Sustained virological response (SVR) was confirmed by undetectable serum HCV-RNA at the end of treatment and again six months after completion of treatment, as well as just before the beginning of the vaccination schedule. Healthy subjects with available data who had participated in the vaccination schedule were characterized as control group (group C).
All participants of the study population had their height and weight recorded at the beginning of the study and their body mass index (BMI) was calculated by dividing patient’s weight (kg) by the squared height (m2). Patients had also been queried about their drinking behavior, so an individual who had been drinking at least 30 gm of alcohol per day for at least 5 years was considered as an alcoholic and was excluded from the study. Patients excluded from our study were also those with histologically confirmed or clinically decompensated liver cirrhosis, transplanted HCV infected patients or those on waiting list for liver transplantation, patients with chronic renal failure, HIV-positive patients, patients with solid tumors or hematological malignancies, immunosuppressed patients in general or those who had ever received immunosuppressive treatment. Pregnant women and patients under 18 or over 70 years of age, as well as people, who had already been exposed to hepatitis B virus as confirmed by their serological status, were also excluded.
Routine biochemical and hematological tests were performed using automated techniques. Hepatitis B surface antigen (HBsAg), antibody to hepatitis B surface antigen (anti-HBs), and total antibody to hepatitis B core antigen (anti-HBc) as well as antibody to human immunodeficiency virus (anti-HIV) and antibody to hepatitis C virus (anti-HCV) were detected using routine commercially available enzyme immunoassays (Abbott Laboratories, Abbott Park, Illinois, USA). Serum HCV-RNA levels were measured in anti-HCV positive patients by a commercially-available quantitative polymerase chain reaction (PCR) assay (Cobas Amplicor HCV test, version 2, Roche Diagnostics, Branchburg, New Jersey, USA) and HCV genotype was defined in HCV-RNA positive patients using INNOLIPA HCV assay (Innogenetics, Belgium).
Liver biopsy was performed in CHC patients according to Menghini technique. Eligible anti-HCV positive/HCV-RNA positive patients had at least two available biochemical determinations of serum alanine transaminase (ALT) levels being above 60 IU/L (> 1.5 times the upper limit of normal) and had no contraindication to liver biopsy. Patients were excluded from liver biopsy if they had a serious medical condition (heart failure, renal failure, uncontrolled hypertension or diabetes mellitus etc), or elevated bleeding risk (platelets < 100 000/mm3, prothrombin time ≥16 s, treatment with heparin or coumadin, aspirin or non-steroidal anti-inflammatory drugs in the past 8 d). Liver tissue was fixed in 10% formalin and paraffin-embedded sections were stained with hematoxylin-eosin and trichrome stains. A single experienced hepatopathologist, who was blinded to clinical markers other than HCV-antibody status, evaluated all biopsy specimens that were scored according to Ishak scoring system (grade = 0-18, stage = 0-6)[17]. As previously mentioned, CHC patients with histologically confirmed cirrhosis were excluded from the study.
All patients and healthy subjects (controls) received 20 μg of recombinant DNA vaccine for hepatitis B (Engerix-B, GSK) intramuscularly (deltoid region) at three different time intervals (0, 1, 6 mo). Determination of anti-HBs antibodies was performed in all individuals of the study population within 3 mo following the third dose of the vaccine. Seroconversion was considered if anti-HBs levels were above 10 mIU/mL and non-reagent response if anti-HBs levels were below 10 mIU/mL.
Moreover, we prospectively selected 30 non-cirrhotic CHC patients and evaluated them for the efficacy of the same vaccine, using the same dose (20 μg) and treatment schedule (0, 1, 6 mo) randomized them (1/1 randomization) in two groups. In group-1, 15 patients received the first dose of the vaccine in parallel with the initiation of pegylated interferon-α2a plus ribavirin treatment, whereas in group-2, 15 patients received the same vaccination schedule without concomitant treatment for chronic hepatitis C. All group-1 patients were treated with fixed dose of pegylated interferon-α2a (180 μg/wk) and genotype-related ribavirin dose (800 mg/d for genotype 2/3 and 1000-1200 mg/d for genotype 1/4-infected patients, depending on baseline body weight-< or ≥ 85 kg, respectively). The duration of treatment was genotype-based (24 wk for genotype 2/3 infected patients and 48 wk for genotype 1/4-infected ones). Determination of anti-HBs antibodies was performed in all CHC patients from both groups at baseline as well as one month following every dose of the vaccine (at mo 1, 2, and 7) and seroconversion was also considered if anti-HBs levels were above 10 mIU/mL.
The study conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Written informed consent forms were obtained from the participants in the prospective schedule of the study before the liver biopsy procedure.
Statistical analysis of data was based on ANOVA student’s t-test and chi-square analysis (χ2). The results are presented as mean ± SD. A probability value of less than 5% (P < 0.05) was considered significant.
Group A, group B and group C participants of the study population were age, sex and BMI matched [age: 27.1 ± 4.0 versus 27.8 ± 4.4 versus 26.7 ± 4.5, respectively, P = 0.63, sex (male/female): 44/26 versus 14/8 versus 63/58, respectively, P = 0.52, BMI: 22.46 ± 1.6 versus 22.05 ± 0.8 versus 23.01 ± 1.4, respectively, P = 0.43]. Twenty seven of the 70 chronic HCV-infected patients from group A (38.57%) and 10 of 22 from group B (45.45%) were prior injecting drug users (IDU) whereas 13 patients from group A (18.57%) and 4 from group B (18.18%) had post-transfusion hepatitis (PTH) C. The rest of chronic hepatitis C patients from both groups had the cryptogenic form of transmission of HCV infection. Twenty five of 70 group-A patients (35.71%) and 9 of 22 group B ones (40.9%) had been infected by genotype-1 of HCV. The remaining 58 chronic HCV-infected patients of the study population had been infected by genotype-3 (50/58, 86.2%) or 2 (8/58, 13.8%) of HCV.
Fifty-eight of the 70 group A patients (82.85%), 20 of the 22 group B ones (90.9%) and 112 of 121 healthy subjects (92.56%) had been seroconverted (anti-HBs ≥ 10 mIU/mL) within three months following the third dose of the vaccine. The vaccination-induced seroconversion rates were significantly higher in the control group than in treatment-naïve CHC patients (P = 0.04) whereas the corresponding rates were comparable between group A and group B CHC patients (P = 0.38). Overall, among the 92 CHC patients who had been evaluated, 78 (84.78%) had been seroconverted to anti-HBs, a percentage significantly lower than the corresponding one from the control group (P < 0.05). The finding that among the 14 non-responders to vaccination schedule chronic HCV-infected patients from both groups (12 treatment-naïve and 2 SVR's), the vast majority (10/14, 71.43%) had been infected by genotype-1 of HCV seems very important and needs further investigation.
Table 1 shows the epidemiological, virological and histological baseline data of group-1 and group-2 CHC patients of the study population. The two groups were comparable for all baseline parameters (age, sex, BMI, viral load, HCV-genotype, grade and stage of liver disease) before the initiation of the vaccination schedule, with (group-1) or without (group-2) concomitant antiviral-immunomodulatory treatment. The anti-HBs antibody response rates were comparable between these two groups of CHC patients at mo 1 (20% vs 26.7%, P = 0.67), mo 2 (46.7% vs 60%, P = 0.46) and mo 7 (86.7% vs 93.3%, P = 0.54) of follow-up, as shown in Figure 1.
| Group 1(n = 15) | Group 2(n = 15) | P-value | |
| Age (yr) | 26.9 ± 3.8 | 27.3 ± 4.1 | 0.510 |
| Sex (male/female) | 8/7 | 9/6 | 0.713 |
| ΒΜΙ (kgr/m2) | 22.45 ± 1.8 | 22.12 ± 0.9 | 0.390 |
| HCV-RNA (-log10 IU/mL) | 5.32 ± 0.67 | 5.24 ± 0.52 | 0.765 |
| Grade (0-18) | 5.6 ± 2.3 | 4.2 ± 1.5 | 0.089 |
| Stage (0-6) | 1.3 ± 0.5 | 1.5 ± 0.7 | 0.276 |
| Genotype (1/non-1) | 3/12 | 2/13 | 0.624 |
The main findings of our study were that chronic HCV infected patients exhibit a lower response to recombinant HBV vaccine compared to healthy subjects, using the recommended dose (20 μg) and the typical vaccination schedule (0, 1, 6 mo), irrespective of the virological response to prior interferon-alpha plus ribavirin treatment. Moreover, we found that concomitant pegylated interferon-alpha plus ribavirin treatment does not influence the antibody response to HBV vaccine in chronic HCV infected treated patients.
Factors known to affect HBV vaccine immunogenicity include age, sex, BMI and smoking[18]. In our study all these parameters except for the smoking behavior, which had not been taken under consideration, were comparable between the patients and the control group of the study population. Occult HBV infection (confirmed as serum HBV-DNA positivity by a sensitive PCR assay in the absence of serological markers of HBV infection) is considered to be associated with the absence of response to recombinant HBV vaccine[19]. Cacciola et al reported that chronic HCV infected patients exhibit a particularly high incidence of occult HBV infection[20], which means that the absence of serum HBV-DNA testing in our study population possibly represents a limitation of our study. On the other hand, the results of our study reflect the expected immunogenicity of HBV vaccine in chronic HCV-infected patients in the current clinical practice where HBV seronegative, chronic HCV-infected patients, are not routinely tested for serum HBV-DNA.
Hyporesponsiveness to HBV vaccine in chronic HCV infected patients had been previously demonstrated by other studies, especially in cirrhotic patients[12,13,14]. Several factors can explain the reduced cellular and humoral arms of immune response in these patients, including the lymphocytopenia and the altered composition of the T-lymphocyte subpopulation in the peripheral blood, the inappropriate interaction between antigens, T-cells and T-cell receptor/major histocompatibility complex molecule, and the impaired proliferative response to T-cell activation by various mitogens[14]. Liver cirrhosis, confirmed either by liver biopsy or signs of decompensation (jaundice, ascites, variceal bleeding, etc) was one of the exclusion criteria of our study population, suggesting that chronic HCV infected patients exhibit a lower response to HBV vaccine even in the absence of severe liver disease. A possible impairment in both humoral and cellular-mediated immune responses in non-cirrhotic chronic HCV-infected patients has been suggested to explain this low response to HBV vaccination in such individuals[13,21].
HCV viral load does not seem to correlate with the vaccination-induced anti-HBs response in chronic HCV infected patients vaccinated against HBV[13], a finding that was also observed in our study. Sustained virological response following interferon-alpha plus ribavirin combination treatment was not related to statistically significant increase in anti-HBs seroconversion rates compared to untreated chronic HCV-infected patients in our study. On the other hand, there are some studies that suggest a negative correlation between viral load of HCV and antibody response to HBV vaccination[12], considering that detection of leukocytes, monocytes/macrophages and B-lymphocytes HCV genomic sequences in chronic HCV-infected patients[22] could possibly influence the immune response to HBV vaccine. The results of our study suggest that the sustained absence of viremia following interferon plus ribavirin combination treatment is possibly not enough to positively influence the impaired immune response of chronic HCV-infected patients. In concern to HCV genotype, there is only one study that showed a worse response to HBV vaccine in patients who had been infected by genotype-1 of HCV as compared to those infected by genotype 2 or 3[23], suggesting that in genotype-1 infected patients a different HBV vaccination schedule with possibly higher doses and shorter intervals between the vaccine doses should be used in order to obtain a better response. As previously noted the majority of non-responders to vaccine of the chronic HCV-infected patients of our study population (71.43%) had been infected by genotype-1 of HCV, a finding that needs further investigation.
There is currently no consensus on the optimal HBV vaccination schedule for chronic HCV-infected patients, especially in those who need antiviral-immunomodulatory treatment. Nowadays pegylated interferon-alpha plus ribavirin represent the initial treatment of chronic hepatitis C patients. Interferon-alpha has been previously used as a co-stimulant in non-responders to primary HBV vaccination schedules[24]. Chlabicz et al published a study that did not demonstrate any beneficial or detrimental effect of interferon-alpha on HBV vaccine immunogenicity[16]. Moreover, this study suggests that vaccination against HBV during treatment with interferon-alpha is safe and well tolerated. It should be noted however that, in this study, the interferon-treated group was small and the patients had received varying numbers of interferon doses as well as different interferon types (α2a, α2b). In our study we evaluate the HBV vaccination induced anti-HBs seroconversion rates in chronic HCV-infected patients during fixed dose pegylated interferon-alpha plus ribavirin combination treatment. We found no differences in the anti-HBs seroconversion rates between the treatment-naïve and the treatment-experienced group of chronic HCV-infected patients; this finding needs further confirmation in prospectively scheduled large-scale controlled studies.
In conclusion, the immunogenicity of the recombinant HBV vaccine seems to be lower in chronic HCV-infected patients as compared to healthy subjects. Sustained virological response following interferon plus ribavirin combination treatment does not affect the antibody response to HBV vaccine in chronic HCV-infected patients, whereas infection by genotype-1 of HCV seems to negatively influence the anti-HBs seroconversion rates. Vaccination against HBV during pegylated interferon-alpha plus ribavirin combination treatment is not beneficial in terms of anti-HBs seroconversion rates, as compared to treatment-naïve HBV-vaccinated chronic HCV-infected patients.
S- Editor Wang J L- Editor Karam SM E- Editor Liu WF
| 1. | Lee WM. Hepatitis B virus infection. N Engl J Med. 1997;337:1733-1745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1728] [Cited by in RCA: 1712] [Article Influence: 61.1] [Reference Citation Analysis (0)] |
| 2. | Alter MJ. Epidemiology of hepatitis C. Hepatology. 1997;26:62S-65S. [PubMed] |
| 3. | Delage G, Infante-Rivard C, Chiavetta JA, Willems B, Pi D, Fast M. Risk factors for acquisition of hepatitis C virus infection in blood donors: results of a case-control study. Gastroenterology. 1999;116:893-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Lemon SM, Thomas DL. Vaccines to prevent viral hepatitis. N Engl J Med. 1997;336:196-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 197] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Encke J, zu Putlitz J, Wands JR. DNA vaccines. Intervirology. 1999;42:117-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Coates RA, Halliday ML, Rankin JG, Stewart JD, Bristow NJ, Granero R, West DJ. Viral Hepatitis and Liver Disease. New York: AR Liss 1998; 1038-1042. |
| 7. | Zarski JP, Bohn B, Bastie A, Pawlotsky JM, Baud M, Bost-Bezeaux F, Tran van Nhieu J, Seigneurin JM, Buffet C, Dhumeaux D. Characteristics of patients with dual infection by hepatitis B and C viruses. J Hepatol. 1998;28:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 243] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Crespo J, Lozano JL, Carte B, de las Heras B, de la Cruz F, Pons-Romero F. Viral replication in patients with concomitant hepatitis B and C virus infections. Eur J Clin Microbiol Infect Dis. 1997;16:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Pontisso P, Ruvoletto MG, Fattovich G, Chemello L, Gallorini A, Ruol A, Alberti A. Clinical and virological profiles in patients with multiple hepatitis virus infections. Gastroenterology. 1993;105:1529-1533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 168] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | National Institutes of Health (NIH) Consensus Development Conference Panel Statement. Management of hepatitis C. Hepatology. 1997;suppl 26:S2-10. |
| 11. | Siddiqui F, Mutchnick M, Kinzie J, Peleman R, Naylor P, Ehrinpreis M. Prevalence of hepatitis A virus and hepatitis B virus immunity in patients with polymerase chain reaction-confirmed hepatitis C: implications for vaccination strategy. Am J Gastroenterol. 2001;96:858-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Leroy V, Bourliere M, Durand M, Abergel A, Tran A, Baud M, Botta-Fridlund D, Gerolami A, Ouzan D, Halfon P. The antibody response to hepatitis B virus vaccination is negatively influenced by the hepatitis C virus viral load in patients with chronic hepatitis C: a case-control study. Eur J Gastroenterol Hepatol. 2002;14:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Wiedmann M, Liebert UG, Oesen U, Porst H, Wiese M, Schroeder S, Halm U, Mössner J, Berr F. Decreased immunogenicity of recombinant hepatitis B vaccine in chronic hepatitis C. Hepatology. 2000;31:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 117] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Idilman R, De MN, Colantoni A, Nadir A, Van Thiel DH. The effect of high dose and short interval HBV vaccination in individuals with chronic hepatitis C. Am J Gastroenterol. 2002;97:435-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Lee SD, Chan CY, Yu MI, Lu RH, Chang FY, Lo KJ. Hepatitis B vaccination in patients with chronic hepatitis C. J Med Virol. 1999;59:463-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Chlabicz S, Grzeszczuk A, Łapiński TW. Hepatitis B vaccine immunogenicity in patients with chronic HCV infection at one year follow-up: the effect of interferon-alpha therapy. Med Sci Monit. 2002;8:CR379-CR383. [PubMed] |
| 17. | Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F, Denk H, Desmet V, Korb G, MacSween RN. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3521] [Cited by in RCA: 3782] [Article Influence: 126.1] [Reference Citation Analysis (1)] |
| 18. | Rosman AS, Lieber CS. Improving the response to hepatitis B vaccine. Infect Med. 1999;16:205-210. |
| 19. | Luo KX, Wang LP, Nie J, Jiang S. Is nonresponsiveness to hepatitis B vaccine due to latent hepatitis B virus infection. J Infect Dis. 1992;165:777-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Cacciola I, Pollicino T, Squadrito G, Cerenzia G, Orlando ME, Raimondo G. Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease. N Engl J Med. 1999;341:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 474] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 21. | Van Thiel DH. Vaccination of patients with liver disease: who, when, and how. Liver Transpl Surg. 1998;4:185-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Lerat H, Rumin S, Habersetzer F, Berby F, Trabaud MA, Trépo C, Inchauspé G. In vivo tropism of hepatitis C virus genomic sequences in hematopoietic cells: influence of viral load, viral genotype, and cell phenotype. Blood. 1998;91:3841-3849. [PubMed] |
| 23. | Mattos AA, Gomes EB, Tovo CV, Alexandre CO, Remião JO. Hepatitis B vaccine efficacy in patients with chronic liver disease by hepatitis C virus. Arq Gastroenterol. 2004;41:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Goldwater PN. Randomized comparative trial of interferon-alpha versus placebo in hepatitis B vaccine non-responders and hyporesponders. Vaccine. 1994;12:410-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |