INTRODUCTION
Having a biopsy specimen histologically proving melanoma of the gallbladder, it is difficult to determine whether it is a primary or secondary tumor. Even though gallbladder and this metastatic lesion comprises between 50%-66% of gallbladder metastasis[1], the occurrence of metastasis in the gallbladder is rare and has only been reported in the literature exceptionally[2-7]. Both primary melanoma in the gallbladder and isolated metastasis to the gallbladder, are not common events. In fact, primary melanoma in the gallbladder is an extremely rare condition and its existence is still questioned by some. According to the literature, primary malignant melanoma in the gallbladder is a controversial issue, and it is still far from clear whether primary melanoma of this organ is a definite entity in itself. Herein, we present a patient in whom malignant melanoma developed initially in the gallbladder. There was no evidence of another acceptable primary site in postoperative investigation and no previous history could be obtained of a pigment cutaneous lesion, which had been treated or regressed.
CASE REPORT
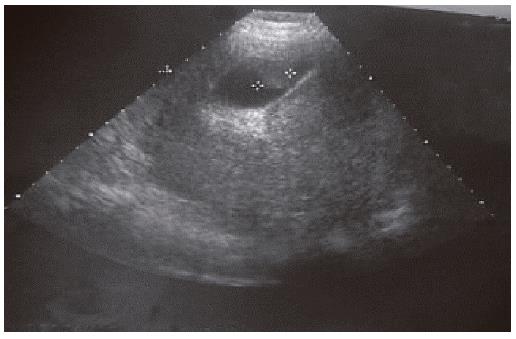
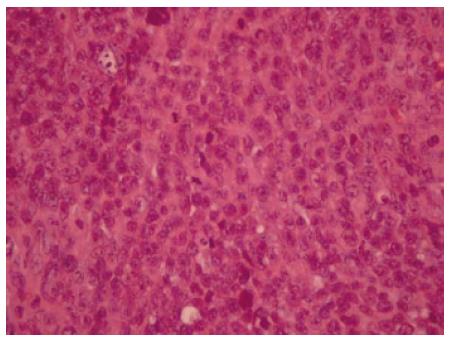
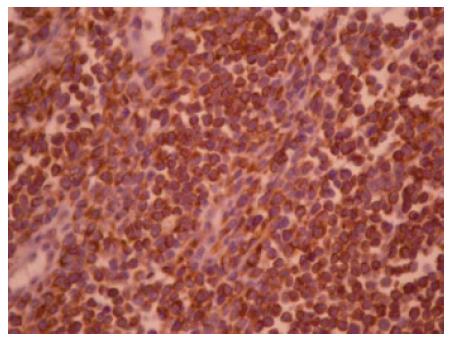
A 38-year old woman presented with a 36-h history of right upper abdominal pain associated with nausea, vomiting and a temperature 38.6°C. Physical examination revealed the presence of severe tenderness in the right upper quadrant of the abdomen. The gallbladder was not palpable. The hematological tests showed an elevation of her white blood cell count (WBC) to 13 800/mm3 with neutrophilia. Liver function studies were normal; these laboratory findings disclosed the following values (the normal reference range is given in parentheses): serum aspirate aminotransferase, 21 IU/L (< 30 IU/L); alanine aminotransferase, 19 IU/L (< 30 IU/L); serum alkaline phosphatase, 184 IU/L (100-320 IU/L); serum g-glutamyl transpeptidase, 30 IU/L (16-73 IU/L); and the serum bilirubin, 0.7 mg/dL (< 1 mg/dL). Ultrasound examination of the gallbladder did not demonstrate lithiasis but a polypoid mass without acoustic shadowing (Figure 1). The patient underwent open cholecystectomy. The specimen was opened and a polypoid mass measuring 1.5 cm × 2.0 cm of dark-yellow color was revealed. The postoperative course of the patient was uneventful, but the histological report indicated a melanoma of the gallbladder (Figures 2 and 3). In H&E stain the diagnosis of a primary melanoma was suspicious, confirmed by immunostaining (HMB-45). After that, a meticulous medical history, physical examination and imaging check did not reveal any other primary focus of the disease. No evidence of the disease was marked after six months in the periodical control, however, four months later the patient died from cerebral hemorrhage due to brain metastasis. Although the patient was informed of her disease, she refused any chemotherapy as well as the proposed transplenic immunostimulation[8,9].
Figure 1 Ultrasound of melanoma of gallbladder.
Figure 2 Histological appearance of melanoma of gallbladder stained with HE.
× 400.
Figure 3 Neoplastic cells immunostained with anti-HMB-45 antibodies.
× 400.
DISCUSSION
Theoretically, according to histogenesis, melanoblasts have not yet been demonstrated in organs of endodermal origin[10] and as gallbladder is an endodermal derivative, it is unlikely that melanoma arises from this organ or other visceral structures. On the other hand, non neoplastic melanoblasts resulting from migration of melanin-producing cells from the neural crest to endodermal derivatives during embryologic development explains the presence of melanocytes within their mucosa[11-13] and supports the possibility of developing primary melanomas at these sites[14]. Therefore, primary melanoma of the gallbladder is at least theoretically possible[4,15]. Even though primary melanoma of the gallbladder remains a debatable clinical entity, reports on this subject continue to accrue. In 1907 the first primary melanoma of the gallbladder was described by Wieting and Handi[16] and fifty years later Walsh reported the first histologically proven case of primary gallbladder melanoma[17]. Since that time there have been additional reports of primary melanoma of the gallbladder[12,15,18-20]. In fact, it is very difficult to differentiate primary from metastatic lesions based on histological features. Mac Fadden et al, compared primary and metastatic biliary melanomas and found that the two groups displayed remarkable similarity with regard to pathologic findings[13]. To help in the differentiation between primary and metastatic melanoma of the gallbladder, according to the literature, the following clinical and pathological criteria should be fulfilled: (1) any other obvious primary site must be excluded by medical history and laboratory investigation, and (2) the tumor, either papillary or polypoid, must be solitary arising from the mucosa of the gallbladder and display junctional activity[2-4]. Junctional activity, i.e, intraepithelial extension in the mucosa overlying the tumor is considered as significant finding in the diagnosis of the primary melanoma of mucosal surfaces[11,21]. However, the presence of atypical melanocytes in the adjacent epithelium of invasive tumor does not necessarily define a primary tumor[22]. Although the presence of “junctional changes” of the mucosa is still controversial, the presence of a solitary polypoid tumor within the lumen of the gallbladder accompanied by junctional activity within the tumor and the absence of an antecedent history of melanoma, or lack of another obvious primary site, are factors that suggest the gallbladder as the primary site of origin. Finally, even today, the establishment of primary histogenesis in these cases is contingent upon a detailed medical history of the patient, a thorough cutaneous and ophthalmic inspection and a radiologic control. However, there always exists the possibility that a regressed primary tumor is a hidden source of gallbladder melanoma. In regard to clinical presentation, involvement of the gallbladder rarely produces symptoms, which could explain the paucity of cases reported in the literature[23], however, as it is usually reported including our case, acute cholecystitis without the presence of stone in the majority of cases was the initial clinical manifestation and the reason for emergency admission in the hospital. In contrast to gallbladder cancer, melanoma of the gallbladder does not seem to be associated to cholelithiasis. In 1999 Dong et al, after having reviewed the literature, found that gallstones appear to be only incidentally and namely in 21.1% of cases (4 of 19 patients) with primary lesions and 27.3% of cases (3 of 11 patients) with symptomatic metastatic disease and this was consistent with the results of their series[24]. Several diagnostic modalities have been employed to investigate gallbladder lesions. Ultrasound is by far the most useful tool in this attempt. Upper ultrasound abdominal examinations are frequently requested in patients with thick high grade malignant melanoma or clinical suspicion of metastasis. Ultrasound may document metastatic lesions within the gallbladder. However, polypoid lesions in the lumen of the gallbladder present a focal thickening of the gallbladder wall without acoustic shadowing, due to their lower density in relation with gallstones. As autopsy studies have confirmed the incidence of the gallbladder metastasis from malignant melanoma to be 15%, a careful review of the gallbladder is advocated when abdominal ultrasound examination is performed on patient with malignant melanoma. Ultrasound helps to distinguish between metastasis and benign polyps. The importance of size of the lesion is obvious as 94% of the benign lesions are less than 1 cm in diameter, whereas, 88% of malignant lesion are more than 1 cm[25]. If the presence of vascular flow within the mass itself is documented, the usefulness of colour-flow Doppler ultrasonography is evident[26]. Computed tomography is of some value especially in detecting metastatic disease.
Surgical excision is the treatment of choice of both primary and metastatic melanomas of gallbladder. During surgery a thorough search is needed in order to detect any possible abdominal metastasis, as the majority of gallbladder metastases are totally asymptomatic. Although in most cases these metastases are in the form of multiple serosal implants, there are intraluminal metastases involving the mucosa and this fact creates difficulties in detecting these metastases during surgery. Although the mainstay of treatment is surgical removal of the gallbladder, we believe that study of the clear role of adjuvant chemotherapy, hormonotherapy or immunotherapy at increasing the survival rate is necessary. Basically, the presence of multiple metastases is an indication of systematic chemotherapy. Till today, the usefulness of adjuvant chemotherapy for both primary and metastatic melanomas remains to be clarified, as only one controlled trial has shown significant improvement in response rate mid survival with the combination dacarbazine and tamoxifen[27]. Despite appropriate therapy, the diagnosis of either condition portends a poor prognosis with few patients surviving more than two years. Furthermore, according to Langley, the prognosis of metastatic melanoma is dismal and the average survival is 7 mo[28].
In conclusion, firstly, the outlook of patients with gallbladder melanoma remains bleak and secondly, the existence of primary melanoma of the gallbladder is still questionable, and certainly will not be settled by this article.