Published online Jun 21, 2006. doi: 10.3748/wjg.v12.i23.3776
Revised: January 28, 2006
Accepted: February 18, 2006
Published online: June 21, 2006
Acute ischemic proctitis is a rare pathological condition. We report here a patient presented with massive rectal haemorrhage from a bleeding vessel superimposed on an underlying pathology of ischemic proctitis. This case report illustrates the difficulties in making the clinical distinction between ischemic proctitis and other pathological entities. We also discussed the beneficial role of arteriogram with embolotherapy as an effective therapeutic measure in the management of lower gastrointestinal bleeding. The literature on the subject is reviewed.
- Citation: Yip VS, Downey M, Teo NB, Anderson JR. Management of ischemic proctitis with severe rectal haemorrhage: A case report. World J Gastroenterol 2006; 12(23): 3776-3778
- URL: https://www.wjgnet.com/1007-9327/full/v12/i23/3776.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i23.3776
Ischemic proctitis is a rare pathological condition. Bharucha et al[1]reviewed all ischemic proctosigmoiditis cases between 1976 and 1991, and only identified 10 cases (6 acute and 4 chronic cases) out of 328 cases of colonic ischemia. Most ischemic proctitis reported was secondary to radiotherapy, previous vascular intervention, aorto-iliac surgery, vasculitis or myointimal hyperplasia of the mesenteric vein[1-5]. These interventions or pathologies can potentially compromise the arterial supply of the rectum, leading to ischemia. It is even less common for the occurrence of spontaneous ischemic proctitis, which accounted for less than 2% of all cases of ischemic colitis.
We present herein a patient with severe rectal haemorrhage from a bleeding vessel and a co-existing pathology of ischemic proctitis.
A 62-year-old male, with grade 2 primary hypertension (1999 WHO/ISH classification) and no other past medical history, first presented as an emergency with a 2-wk history of diarrhoea, colicky lower abdominal pain and proctalgia. Vital signs and abdominal examination were unremarkable but rectal examination revealed marked tenderness and fresh rectal bleeding.
Full blood count, CRP, urea and electrolytes were normal. Abdominal radiology and stool culture were negative. Examination under anaesthesia revealed marked inflammation and superficial ulceration in the rectum and distal sigmoid colon. These changes were in keeping with a presumptive diagnosis of inflammatory bowel disease. Whilst histology of rectal biopsy was awaited, the patient was commenced on steroid enemata and discharged with out-patient follow-up.
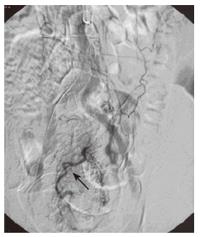
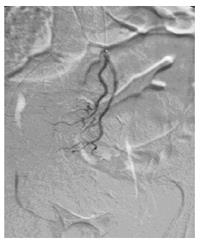
The patient was readmitted three days later with hypovolaemic shock secondary to profuse rectal bleeding. Following resuscitation and stabilization, an emergency mesenteric arteriogram was performed. Selective examination of the inferior mesenteric artery revealed for the first time vasculature abnormality arising from a branch of the superior rectal artery with early filling of a large vein, consistent with a radiological evidence of arterio-venous fistula (Figure 1). The artery was selectively catheterised and the feeding vessel was embolized with Gel foam pledgets (Figure 2). The rectal blood supply appeared to be intact after the embolization.
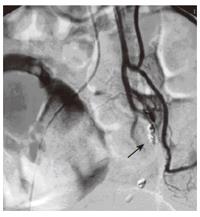
The patient rebled two days later and repeated arteriography demonstrated re-canalisation of the venous drainage. In view of the re-canalisation, segment of superior rectal artery was embolized with Gel foam pledgets and metallic coils. There was no radiological evidence of further extravasations following the second embolization (Figure 3). After the second radiological intervention, result of the rectal biopsy from the first admission was then available and demonstrated features consistent of ischemic proctitis.
The patient had another episode of rectal bleeding 48 h later. Flexible sigmoidoscopy showed a grossly ischemic mucosa with numerous vertical linear ulcers. The segment of the affected rectum was well demarcated. A low Hartmann’s procedure was successfully carried out with the preservation of the anal sphincter complex. Histology of the resected rectum demonstrated broad areas of necrosis in both mucosal and submucosal layers, confirming the diagnosis of ischemic proctitis.
Patient had a slow recovery. The colostomy was reversed twelve months later with the fashioning of a colo-anal anastomosis.
Rectum has an extensive arterial supply network from the inferior mesenteric, internal iliac, internal pudendal arteries, and the marginal artery. This rich collateral supply explain why rectum is normally spared in ischemic colitis and hence the rare occurrence in literatures.
The exact mechanism for acute ischemic proctitis remains unknown. Physiological vasoconstriction secondary to mild central hypovolaemia has been shown to reduce intestinal mucosal perfusion, which might explain in part to the occurrence of acute ischemic proctitis[1,6]. This similar view was also expressed by Bharucha et al[1]. The hypovolaemic event in our patient would have therefore further compromised the arterial supply of the rectum, leading to the worsening of the ischemic proctitis.
Clinical presentation of patients with ischemic proctitis may be non-specific and often misleading, since they often present with lower abdominal pain, diarrhoea with bloody discharge, proctalgia, and rectal mucosal erosion on inspection. These presentations are also commonly seen in patients with inflammatory bowel disease, pseudomembranous colitis or neoplasia, and the distinction between these pathological entities can be difficult[7-9]. Histology is often required to confirm the diagnosis.
Conservative management is normally sufficient for majority of the cases of lower gastrointestinal bleeding. When conservative management fails, the aim for the subsequent treatment is to identify the source of bleeding, and coagulate the bleeding point. Emergency arteriography has been shown to be an effective option to locate the bleeding point, with a reported of successful localisation of active bleeding site between 40%-77%[10]. Our treatment was similar to the two-stage embolization approach described by Waugh et al[11]. We employed the super-selective technique for the initial embolization, and then a second more proximal embolization when the first attempt failed. Because histological diagnosis of ischemic proctitis from the initial biopsy was not available prior to both arteriogram interventions, rectal ischemia was aggravated by the embolization procedure in our case.
In retrospect, this case presented a clinical dilemma with a visualised extravasation in arteriogram ready for embolization in one hand, but with a co-existing pathology of ischemic proctitis in the other. Nevertheless, arteriogram embolizations offered window opportunities for adequate fluid resuscitation and stabilisation. As with the opinions of Waugh et al, arteriogram embolization allows the conversion of an emergency case to a semi-elective case scenario[11]. Due to the ability to localise an active bleeding site, a hemicolectomy can be performed as comparing to a subtotal colectomy, which carried a significantly higher mortality (10% vs 22%-37%, respectively)[12-15].
In conclusion, ischemic proctitis is difficult to diagnose clinically because of its rarity and close resemblance in clinical presentation to other pathological conditions. It represents a difficult management problem when there are co-existing clinical scenarios of a massive haemorrhage secondary to a bleeding vessel and an underlying ischemia. Emergency trans-catheterisation embolization can be a beneficial diagnostic and therapeutic tool in the management of similar cases, by providing a window period for optimal resuscitation prior to definitive surgical intervention.
S- Editor Wang J L- Editor Kumar M E- Editor Liu WF
| 1. | Bharucha AE, Tremaine WJ, Johnson CD, Batts KP. Ischemic proctosigmoiditis. Am J Gastroenterol. 1996;91:2305-2309. [PubMed] |
| 2. | Haglund U, Bergqvist D. Intestinal ischemia -- the basics. Langenbecks Arch Surg. 1999;384:233-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Jaeger HJ, Mathias KD, Gissler HM, Neumann G, Walther LD. Rectum and sigmoid colon necrosis due to cholesterol embolization after implantation of an aortic stent-graft. J Vasc Interv Radiol. 1999;10:751-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Savoie LM, Abrams AV. Refractory proctosigmoiditis caused by myointimal hyperplasia of mesenteric veins: report of a case. Dis Colon Rectum. 1999;42:1093-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Reissman P, Weiss EG, Teoh TA, Lucas FV, Wexner SD. Gangrenous ischemic colitis of the rectum: a rare complication of systemic lupus erythematosus. Am J Gastroenterol. 1994;89:2234-2236. [PubMed] |
| 6. | Thorén A, Ricksten SE, Lundin S, Gazelius B, Elam M. Baroreceptor-mediated reduction of jejunal mucosal perfusion, evaluated with endoluminal laser Doppler flowmetry in conscious humans. J Auton Nerv Syst. 1998;68:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ritchie JK, Lennard-Jones JE. Crohn's disease of the distal large bowel. Scand J Gastroenterol. 1976;11:433-436. [PubMed] |
| 8. | Brandt LJ, Boley SJ, Mitsudo S. Clinical characteristics and natural history of colitis in the elderly. Am J Gastroenterol. 1982;77:382-386. [PubMed] |
| 9. | Brandt LJ, Katz HJ, Wolf EL, Mitsudo S, Boley SJ. Simulation of colonic carcinoma by ischemia. Gastroenterology. 1985;88:1137-1142. [PubMed] |
| 10. | Hoedema RE, Luchtefeld MA. The management of lower gastrointestinal hemorrhage. Dis Colon Rectum. 2005;48:2010-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Waugh J, Madan A, Sacharias N, Thomson K. Embolization for major lower gastrointestinal haemorrhage: five-year experience. Australas Radiol. 2004;48:311-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Browder W, Cerise EJ, Litwin MS. Impact of emergency angiography in massive lower gastrointestinal bleeding. Ann Surg. 1986;204:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 150] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Drapanas T, Pennington DG, Kappelman M, Lindsey ES. Emergency subtotal colectomy: preferred approach to management of massively bleeding diverticular disease. Ann Surg. 1973;177:519-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 74] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Klas J, Madoff R. Surgical options in lower gastrointestinal bleeding. Semin Colon Rectal Surg. 1997;8:736-737. |
| 15. | O'Neill BB, Gosnell JE, Lull RJ, Schecter WP, Koch J, Halvorsen RA, Harris HW. Cinematic nuclear scintigraphy reliably directs surgical intervention for patients with gastrointestinal bleeding. Arch Surg. 2000;135:1076-1081; discussion 1076-1081;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |