Published online Mar 28, 2006. doi: 10.3748/wjg.v12.i12.1969
Revised: November 2, 2005
Accepted: November 18, 2005
Published online: March 28, 2006
Hepatocellular carcinoma (HCC) is a so highly invasive tumor that metastasizes hematogenously and lymphogenously to distant site. Frequent sites are lung, regional lymph node, bone, and adrenal gland. But metastasis to the gastrointestinal (GI) tract is rare, and most common site is stomach. Metastasis to the small intestine is extremely rare. Moreover, metastatic HCC of the small bowel causing intussusception has not been reported until now. Here, we report a case of metastasis of HCC to the small bowel manifested by intussusception.
- Citation: Kim HS, Shin JW, Kim GY, Kim YM, Cha HJ, Jeong YK, Jeong ID, Bang SJ, Kim DH, Park NH. Metastasis of hepatocellular carcinoma to the small bowel manifested by intussusception. World J Gastroenterol 2006; 12(12): 1969-1971
- URL: https://www.wjgnet.com/1007-9327/full/v12/i12/1969.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i12.1969
Hepatocellular carcinoma (HCC) is a highly malignant tumor with frequent metastasis. Extrahepatic metastases have been reported in 25 to 65 percent of autopsy series, with lung, bones, and regional lymph nodes as the most commonly involved sites[1-5]. Metastasis of HCC to the gastrointestinal (GI) tract is rare and most common site of metastasis is reported stomach by direct invasion of tumor[4,5]. The distant hematogenous metastasis of HCC to the small intestine is extremely rare[6].
The majority of adult intussusceptions arising in the small bowel are due to benign lesions, and metastatic melanoma is the most frequent malignancy causing small bowel intussusception[7]. Intussusception caused by the metastatic HCC to the small bowel has not been reported until now. We report a case of metastasis of HCC to the small bowel manifested by intussusception.
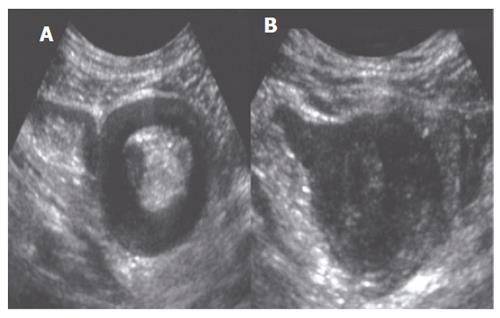
A 65-year-old man was referred to emergency room with complaint of sudden onset, cramping periumbilical pain for 2 d. The pain was continuous with frequent exacerbation, and was associated with nausea and vomiting. The patient had been assigned a diagnosis of hepatitis B virus associated cirrhosis 3 years previously. Two months before, he was diagnosed as HCC with multiple bones and regional lymph nodes metastases according to the large enhanced hepatic mass on computed tomography scan with elevated level of serum alpha-fetoprotein (629 µg/L). On physical examination, the abdomen was distended, with provocable pain in the periumbilical area and increased bowel sound. Complete blood cell count revealed anemia (Hb 72 g/L) and leukocytosis (15.1×109/µL). Liver function tests and renal function test were not remarkable. Plain radiography of abdomen demonstrated presence of marked distension of bowel loops with air fluid level and absence of colonic gas, which were known as a characteristic finding of small bowel obstruction (Figure 1). Computed tomography scan showed ill defined hepatic mass with regional lymph node enlargement and a “target mass” lesion in the right lower abdomen (Figure 2). Abdominal ultrasound showed
10 cm long intussusception in the mid small bowel level (Figure 3A) and a small mass which was suspected of leading point of intussusception was also observed at the head of intussusception (Figure 3B).
After five days of conservative management, segmental small bowel resection and end-to-end anastomosis was performed. At surgery, intussusceptional segment was located at the level of jejunum 110 cm distal from the Treitz ligament and 8 cm sized protruding mass was grown into the lumen of small intestine within intussusceptional segment. Other three masses which measured 0.5 cm, 0.8 cm, and 3 cm respectively were also grown into the lumen at the level of jejunum 170 cm distal from the Treitz ligament.
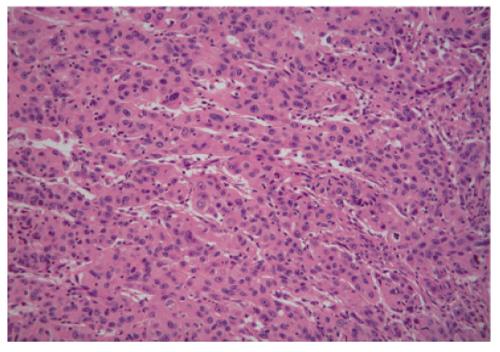
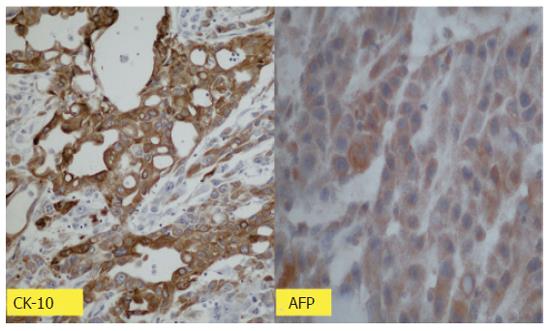
Macroscopic examination of the surgical specimen showed multiple luminal protruding submucosal mass with extension to the subserosa (Figure 4). The largest mass measured 3.0 cm × 2.0 cm × 0.8 cm. In microscopic examination, the atypical epithelial cells were poorly differentiated carcinoma with hepatoid feature of the trabecular pattern (Figure 5). There tumor cells were positive for alpha-fetoprotein and cytokeratin 18 on the immunohistochemical staining (Figure 6). These evidences supported HCC metastasis to small bowel.
HCC is so highly invasive that extrahepatic metastasis is frequently observed [2,5]. The most common site of metastasis is lung, followed by regional lymph node, adrenal gland and bone. HCC metastasis to gastrointestinal tract is a rare condition, being found only in 4-12% of cases in autopsy series[5]. These metastatic lesions are usually asymptomatic, and most are discovered on postmortem examination[8]. Reports of premoterm diagnosis of GI tract involvement in HCC are extremely rare and are associated with poor prognosis[8,9]. Chen et al reported that median survival following the diagnosis of GI tract involvement in HCC was only one month[8].
The modes of metastasis of HCC are known as hematogenous, lymphatic spread and local infiltration[8]. The presumed mode of metastasis of HCC to GI tract is mostly direct invasion to adjacent GI tract via adhesion to the serosal side by bulky mass. Lin et al. reported that nine of eleven patients with HCC represented direct invasion of HCC to adjacent GI tract[9]. In Park’s series, the mode of spread was direct invasion from a contiguous HCC (66.7 %), hematogenous metastasis (17%), peritoneal seeding (6%)[10]. Characteristic features of HCC with direct involvement of GI tract were large, located at the subcapsular area, and had exophyting growth pattern[9,10]. HCC has a high incidence of venous invasion and thrombosis formation. Hematogenous spread of HCC to the GI tract may be caused by tumor thrombi via the portal system and disseminated by hepatofugal portal spread to the GI tract. In previous reports, most of patients with hematogenous metastasis of HCC to the GI tract showed main portal vein thrombosis[8,9]. But in some cases, vascular involvement was not observed. In our case, the presumed mode of metastasis to small intestine was hematogenous spread. However despite of bulky mass with multiple bone metastases, main portal vein thrombosis was not observed.
The most commonly involved site of the GI tract in HCC was reported to be the stomach[9]. The small intestine can often be involved in tumors such as melanoma, carcinoma of the lung, cervix of the uterus, the breast, and colon[11,12]. HCC metastasis to small intestine was rarely reported. Few cases with the involvement of the duodenum have been reported, but in those cases, the duodenum was directly invaded by tumor in the liver[6,8-10]. In our case, HCC metastasized to jejunum by hematogenous spread and formed multiple polypoid masses.
Metastatic tumors in the small intestine predominantly involve the bowel wall, the subserosa, the serosa or the mesentery. But submucosal involvement is rare. According to Farmer and Hawk, metastatic masses to small bowel are divided into three types: (1) spherical mesenteric masses encroaching on or extension into the intestine, (2) intramural masses, often with ulceration; and (3) bulky polypoid masses extending into the bowel lumen [11]. Polypoid lesions are resulted from mucosal or submucosal involvement rather than intramural involvement. In the present case, histological examination showed that polypoid mass sprouted from submucosa and extended to serosa. This finding suggested that the main metastatic site of HCC was the submucosa of the small intestine.
Intussusception, although common in children, is rare in adults and represents 1% of cause of small bowel obstruction in adult [13]. Adult intussusception presents with a variety of acute, intermittent, and chronic symptoms mimicking partial small bowel obstruction[14]. Thus, the diagnosis of intussusception is difficult to make before surgery and computed tomography scan is the most useful diagnostic tool. In distinction to intussusception in children, intussusceptions in adults are mainly resulted from organic lesion. The most common cause of benign lesion was postoperative band and malignant lesions were mainly consisted of metastatic tumor[13]. In previous report, melanoma was the most common tumor of small intestine and lymphoma, followed by sarcoma, squamous cell carcinoma[13]. In our case, cause of small bowel intussusception was diagnosed as metastatic HCC by pathologic examination.
We reported an extremely rare case of metastatic HCC to small intestine, which caused small bowel intussuception in adult. Up to our knowledge, this is the first case report of small bowel intussuception resulting from HCC metastasis.
S- Editor Guo SY L- Editor Zhang JZ E- Editor Cao L
| 1. | Edmondson HA, Steiner PE. Primary carcinoma of the liver: A study of 100 cases among 48,900 necropsies. Cancer. 1954;7:462-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 2. | Kay CJ. Primary hepatic cancer: review of 96 case. Arch Intern Med. 1964;113:46-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Sung JL, Wang TH, Yu JY. Clinical study on primary carcinoma of the liver in Taiwan. Am J Dig Dis. 1967;12:1036-1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 53] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Anthony PP. Primary carcinoma of the liver: a study of 282 cases in Ugandan Africans. J Pathol. 1973;110:37-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 126] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Nakashima T, Okuda K, Kojiro M, Jimi A, Yamaguchi R, Sakamoto K, Ikari T. Pathology of hepatocellular carcinoma in Japan. 232 Consecutive cases autopsied in ten years. Cancer. 1983;51:863-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 6. | Yang PM, Sheu JC, Yang TH, Chen DS, Yu JY, Lee CS, Hsu HC, Sung JL. Metastasis of hepatocellular carcinoma to the proximal jejunum manifested by occult gastrointestinal bleeding. Am J Gastroenterol. 1987;82:165-167. [PubMed] |
| 7. | Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review: adult intussusception--a CT diagnosis. Br J Radiol. 2002;75:185-190. [PubMed] |
| 8. | Chen LT, Chen CY, Jan CM, Wang WM, Lan TS, Hsieh MY, Liu GC. Gastrointestinal tract involvement in hepatocellular carcinoma: clinical, radiological and endoscopic studies. Endoscopy. 1990;22:118-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 63] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Lin CP, Cheng JS, Lai KH, Lo GH, Hsu PI, Chan HH, Hsu JH, Wang YY, Pan HB, Tseng HH. Gastrointestinal metastasis in hepatocellular carcinoma: radiological and endoscopic studies of 11 cases. J Gastroenterol Hepatol. 2000;15:536-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Park MS, Kim KW, Yu JS, Kim MJ, Yoon SW, Chung KW, Lee JT, Yoo HS. Radiologic findings of gastrointestinal tract involvement in hepatocellular carcinoma. J Comput Assist Tomogr. 2002;26:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Farmer RG, Hawk WA, Metastatic tumors of the small bowel. Gastroenterology. 1964;47:496-504. [PubMed] |
| 12. | de Castro CA, Dockery MB, Mayo CW. Metastatic tumors of the small intestines. Surg Gynecol Obstet. 1957;105:159-165. [PubMed] |
| 13. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 666] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 14. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 382] [Article Influence: 13.6] [Reference Citation Analysis (0)] |