Published online Dec 28, 2005. doi: 10.3748/wjg.v11.i48.7684
Revised: February 13, 2005
Accepted: February 18, 2005
Published online: December 28, 2005
Liposarcomas are rare soft tissue tumors, commonly affecting the lower limbs and less commonly the retroperitoneum. Although other organs can be affected, the pancreas is one of the rarest, and metastasis at presentation has never been reported. We describe the case of a 76-year-old gentleman presenting with abdominal pain and an abdominal mass. Imaging confirmed a primary tumor in the body and tail of the pancreas, with a metastatic deposit in the mesentery adjacent to the second part of the duodenum. Biopsy confirmed a liposarcoma, and subsequently a complete surgical excision was achieved. He then received adjuvant radiotherapy and has remained disease free for the next 26 mo.
- Citation: Dodo I, Adamthwaite J, Jain P, Roy A, Guillou P, Menon K. Successful outcome following resection of a pancreatic liposarcoma with solitary metastasis. World J Gastroenterol 2005; 11(48): 7684-7685
- URL: https://www.wjgnet.com/1007-9327/full/v11/i48/7684.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i48.7684
Primary retroperitoneal neoplasms account for only 0.1-0.2% of all malignancies. Liposarcoma is a rare mesenchymal tumor that occurs most commonly in the soft tissues of the extremities, but other sites such as the retroperitoneum can also be involved. Retroperitoneal liposarcomas grow slowly and silently. Prognosis is poor due to relapse, so only complete excision, which is often difficult, produces a ‘cure’[1]. There are only four cases of pancreatic liposarcoma in the literature. To our knowledge, this is the first reported case of metastatic pancreatic liposarcoma at the time of presentation, with successful outcome following surgery.
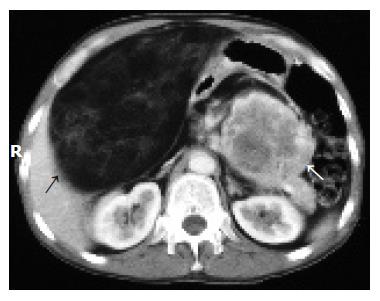
A 76-year-old retired civil engineer presented with a 1-mo history of abdominal pain. He had anorexia associated with significant weight loss. His medical history was unremarkable. He was a smoker and drank a moderate amount of alcohol. On examination he was cachectic and had a large, firm, but non-tender, upper abdominal mass. All blood results including tumor markers (CEA, CA 19.9, AFP, CA125) were within the normal limits. Abdominal ultrasound showed two large masses adjacent to the pancreas. CT scan revealed a 20-cm mass in the mesentery adjacent to the second part of the duodenum, and an 8-cm tumor of the body and tail of the pancreas (Figure 1). The appearances were suggestive of liposarcoma, and this was confirmed by CT-guided core biopsy.
At laparotomy, he had a primary tumor (9 cm×6 cm×2.5 cm) (Figure 2A) in the distal body and tail of the pancreas attached to the spleen and a further tumor (27 cm×20 cm×10 cm) (Figure 2B) adjacent to the second part of the duodenum, not infiltrating the bowel or the pancreas. He underwent distal pancreatectomy with splenectomy and the second lesion, which was encapsulated, was completely enucleated. His post-operative recovery was slow with the development of sepsis and a pancreatic fistula, which was managed conservatively with drainage.
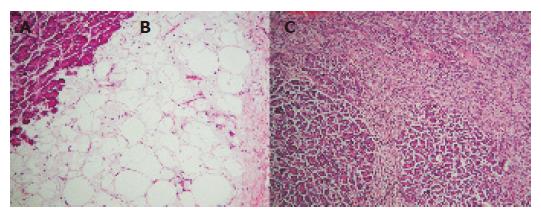
Histology of both masses demonstrated a well diffe-rentiated sclerosing liposarcoma (Figure 3A) with an area within the primary mass of dedifferentiation (Trojani grade 3) (Figure 3B). The patient received adjuvant radiotherapy and was under follow-up with abdominal CT every 6 mo. At 26 mo, there was no evidence of recurrence and he remained asymptomatic.
Liposarcomas are intermediate (locally aggressive) malignant mesenchymal tumor comprising 16-18% of all malignant soft tissue tumors in adults[2]. The incidence is the same in the USA and Europe, with a slight male preponderance[2]. These tumors can grow slowly by direct invasion and can metastasize to the lungs, liver and other viscera[3]. Histologically they can be classified into well differentiated (WD), myxoid, round cell poorly differentiated myxoid and pleomorphic[4,5]. WD liposarcomas are the commonest, accounting for approximately 40-45%[6]. WD liposarcomas can in turn be subdivided morphologically into four main subtypes: adipocytic, sclerosing, inflammatory and spindle cell. This case was a WD sclerosing liposarcoma, which ranks second in frequency, and is most often seen in retroperitoneal and paratesticular lesions[6].
WD liposarcomas show no potential for metastasis unless they undergo dedifferentiation. Dedifferentiation occurs in up to 10%, with 90% arising de novo and the rest in recurrences. Risk of dedifferentiation appears higher with deep-seated (particularly retroperitoneal) lesions and is markedly less in the limbs. This is probably a time-dependant phenomenon. However, it is often impossible to obtain a wide surgical resection margin and local recurrence is almost inevitable and often leads to death[6].
Retroperitoneal liposarcomas produce non-specific symptoms and are often extensive on diagnosis[1]. Most tumors occur at 40-60 years of age, though they may appear at any time. The etiology of these tumors is unknown, although trauma or radiation exposure has been suggested. CT scan is good at characterizing the lesions and aspiration cytology is recommended to differentiate from other pancreatic neoplasms[2]. Pancreatic liposarcomas are very rare with eventual metastases reported in 30-60% of cases[3]. Regardless of cell type, aggressive surgical excision offers the best chance of cure[3]. Some patients may benefit from adjuvant radiotherapy and less commonly chemotherapy. This patient had successful resection of the primary tumor and a giant metastasis followed by adjuvant radiotherapy, and had remained disease free. Prognosis depends on tumor location and histological type[2]. Reported 5-year survival following surgical excision varies from 41%[3] to 50%[4]. Radiotherapy can increase the duration of remission after incomplete excision and possibly achieve clinical cure[3].
Aggressive resection combined with adjuvant radiotherapy should be considered for metastatic pancreatic liposarcomas when feasible as this offers the best chance of cure and follow-up is essential.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | Osmanağaoğlu MA, Bozkaya H, Ozeren M, Cobanoğlu U. Primary retroperitoneal liposarcoma. Eur J Obstet Gynecol Reprod Biol. 2003;109:228-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Amano H, Harima K, Aibe T, Nagatomi Y, Kawashima M, Maetani N, Azuma M, Ariyama S, Fuji T, Kawamura S. A case of pancreatic liposarcoma (author's transl). Nihon Shokakibyo Gakkai Zasshi. 1981;78:1475-1479. [PubMed] |
| 3. | Elliott TE, Albertazzi VJ, Danto LA. Pancreatic liposarcoma: case report with review of retroperitoneal liposarcomas. Cancer. 1980;45:1720-1723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Milano C, Colombato LA, Fleischer I, Boffi A. Liposarcoma of the pancreas. Report of a clinical case and review of the literature. Acta Gastroenterol Latinoam. 1988;18:133-138. [PubMed] |
| 5. | Choux R, Andrac L, Rodriguez M, Masselot R, Hassoun J. Liposarcoma of the pancreas. Study of a case including ultrastructure. Ann Anat Pathol (Paris). 1979;24:251-259. [PubMed] |
| 6. | Dei Tos AP, Pedeutour F. Atypical lipomatous tumor/Well differentiated liposarcoma and Dedifferentiated liposarcoma. Pathology and genetics of tumors of soft tissue and bone. Lyon: IARC Press 2000; 35-39. |