Published online Nov 21, 2005. doi: 10.3748/wjg.v11.i43.6884
Revised: April 1, 2005
Accepted: April 2, 2005
Published online: November 21, 2005
Primary splenic cyst is a relatively rare disease, and the majority of cases are classified as epithelial cysts. Three cases with nonparasitic splenic cysts are presented: two epithelial and one pseudocyst. All cases had an atypical symptomatology, consisted mainly of fullness in the left upper abdomen and a palpable mass. Preoperative diagnosis was established with ultrasonography and computerized tomography. Two cases with large cysts located in the splenic hilum were treated with open complete splenectomy. The most recent case, a pseudocyst, was managed laparoscopically with partial cystectomy. All cases did not have any problems or recurrence during follow-up. Laparoscopic partial cystectomy is an acceptable procedure for the treatment of splenic cysts, because it cures the disease preserving the splenic tissue. Complete splenectomy is reserved for cases in which cyst excision cannot be done otherwise.
- Citation: A M, EP M, T L, D M, C F, G K. Non-parasitic splenic cysts: A report of three cases. World J Gastroenterol 2005; 11(43): 6884-6887
- URL: https://www.wjgnet.com/1007-9327/full/v11/i43/6884.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i43.6884
Splenic cysts are unusual in everyday surgical practice. They can be parasitic (hydatid), caused by the parasite Echinococcus granulosus, or nonparasitic[1,2]. Non-parasitic cysts are classified as primary (true, epithelial), lined by an epithelial cover (epidermoid, dermoid, and mesothelial) or endothelial cover (hemangioma, lymphangioma), and secondary (pseudocysts, non-epithelial), which are usually of post-traumatic origin[3,4].
Primary splenic cysts comprise 30-40% of the total and are encountered more commonly in children and young adults[5,6]. Most of the cysts are asymptomatic, and they are incidental findings during abdominal ultrasonography. The number of diagnosed splenic cysts seems to rise because of the increased use of abdominal imaging techniques[7].
Laparotomy with splenectomy has been the method of choice for the treatment of primary splenic cysts[5,8]. Today, performance of more conservative surgical procedures has been advised, especially in children and young adults, in order to avoid overwhelming postsplenectomy infection[4,8]. Herein, we present three cases with non-parasitic splenic cysts, their diagnostic evaluation and surgical management.
A 15-year-old girl was admitted to our Department with a chief complaint of abdominal fullness. An elastic, hard mass of approximately 15 cm in diameter was palpable in the left upper abdomen. A chest X-ray showed a mild elevation of the left hemidiaphragm. Ultrasonography of the upper abdomen showed a giant cystic lesion with irregular echoic patterns. Computerized tomography confirmed the splenic localization of the cyst and demonstrated almost total displacement of the remaining splenic parenchyma.
At laparotomy, a huge splenic cyst of approximately 15 cm of maximal diameter was revealed, located in the middle of the splenic parenchyma, displacing it towards the splenic poles. First, reduction of the cyst with intraoperative drainage of 1 000 mL of serous fluid was done. However, due to the cyst location, preservation of the spleen was considered impossible, and complete splenectomy followed. The aspirated cystic fluid showed no evidence of malignancy. Histology report revealed that the cyst wall consisted of dense fibrous tissue, covered by stratified squamous or cuboid epithelium. Thus, the diagnosis of a primary epidermoid splenic cyst was established. The postoperative clinical course of the patient was satisfactory and was discharged on postoperative d 7. She received a pneumococcal vaccine and chemoprophylaxis with oral penicillin at a dose of 1 500 000 IU twice daily, for a period of 6 months. Today, the patient is in excellent condition, 8 years after surgery.
A 27-year-old woman presented with mild dyspeptic symptoms, an atypical pain and a sensation of fullness in the epigastrium. Past medical history was negative, and physical examination revealed a 6-7 cm palpable mass in the left upper quadrant of her abdomen. All laboratory tests were normal, and serological tests gave no evidence of parasitic infection with Echinococcus granulosus. Plain abdominal films of the abdomen were negative. Ultrasound and computerized tomography of the abdomen showed a solitary cystic mass in the splenic hilum with a maximum diameter of 8 cm, displacing the splenic parenchyma (Figure 1). Endoscopic examination of the upper gastrointestinal tract did not reveal any significant findings.
The diagnosis of a splenic cyst was confirmed and the patient was subjected to exploratory laparotomy. On exploration, there was a medium-sized splenic cyst located in the hilum, which made splenectomy inevitable. Postoperative recovery was uneventful. Histological examination of the specimen showed a normal splenic parenchyma and an epidermoid splenic cyst with a fibrous wall lined by epithelial cells. The patient had no problems after surgery and she received pneumococcal vaccine and oral penicillin for 6 months. Today she is in good clinical condition, 4 years postoperatively.
A 24-year-old female presented with an asymptomatic lump in the left hypochondriac region, since 2 years. The patient did not have any specific symptoms except for a mild abdominal discomfort and a sensation of fullness in her left upper abdomen. She had a negative medical history. On physical examination, a cystic mass was palpable under the left costal margin, which was moving according to the respiratory movements. The routine hematological and biochemical tests were normal.
Casoni’s skin test and complement fixation test for hydatid disease were negative. A clinical diagnosis of cystic splenomegaly was made and the patient was subjected to radiological investigations. Ultrasonography of the upper abdomen revealed a single unilocular spherical cystic lesion in the anterior surface of the spleen. Computerized tomography confirmed the ultrasound findings of a subcapsular cystic lesion with an almost 10 cm of maximal diameter within the spleen with attenuation value near that of water with a non-calcified wall.
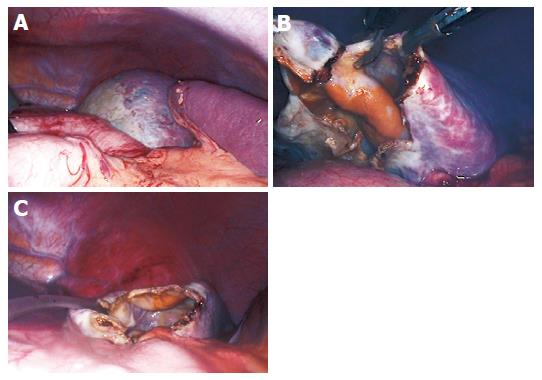
With a preoperative diagnosis of a splenic cyst, the patient was subjected to laparoscopy. Before starting with the procedure, a thorough video-guided inspection of the peritoneal cavity was performed. After focusing on the left upper quadrant, the greater omentum was pulled down, and the cyst was clearly visible in the upper pole of the spleen (Figure 2A). The cyst roof was punctured and about 700 mL of yellowish (serous) fluid was aspirated and sent for culture and cytological examination. A 3 cm×3 cm portion of the collapsed cyst wall was then excised with monopolar scissors, paying attention to remove the cyst wall segment free of splenic parenchyma (Figure 2B).
Thus, there was minimal blood loss and unroofing of the cyst wall was accomplished. The specimen was extracted through a 10-mm port and sent for histological examination. The tip of an elastic drainage tube was left inside the remaining cavity (Figure 2C). The postoperative course was uneventful. The patient resumed oral diet on the first postoperative day, and was discharged on the second postoperative day after the drain was removed.
Bacteriological cultures of the fluid were negative. Cytological examination of the fluid showed a few lymphocytes and histiocytes. Histological examination of the cyst wall revealed the presence of dense cytopenic connective tissue without any epithelial lining, and confirmed the diagnosis of a splenic pseudocyst. The patient is in good clinical condition, one year after surgery, and on follow-up tomographic scan had no evidence of recurrence.
Benign true non-parasitic splenic cysts cannot be clinically distinguished from other types of splenic cysts. They have an inner lining of epithelial cells and are usually of congenital etiology[3,6]. Pseudocysts have an inner lining of connective tissue and are usually secondary to blunt trauma or hemorrhage in the splenic parenchyma, but they may also be of infectious and degenerative origin[9,10]. Both types of splenic cysts do not produce any specific symptoms, until they reach a significant size. Large cysts may cause atypical pain and heaviness in the left hypochondriac region, due to distension of the capsule or space-occupying mechanisms within the abdominal cavity, or they may present as a palpable mass[3,5,9]. Indeed, in our patients, symptomatology was atypical with a sensation of fullness and a palpable mass in the left upper abdominal quadrant, as well as mild dyspeptic symptoms. Symptoms secondary to pressure on surrounding organs, such as nausea, vomiting, flatulence, and diarrhea may gradually appear. Also, pressure in the cardiorespiratory system may cause pleuritic pain or dyspnea, and irritation of the left diaphragm may cause persistent cough[10]. Occasionally splenic cysts may present with complications, such as infection, rupture and hemorrhage[9,11].
When a lump is detected in the left upper quadrant of the abdomen, it is necessary to exclude any disease associated with splenomegaly, mononucleosis, fever of unknown origin, hemolytic anemia, chronic leukemias, collagen vascular disease, and liver diseases[12]. Serological studies are useful in excluding most of the above-mentioned diagnosis. In our cases hematological, biochemical, and serological investigations were negative. Angiography is useful in differentiating a splenic cyst, which is usually avascular, from solid malignant tumors (lymphoma, sarcoma), which usually have neoplastic vasculature in a disorganized pattern[10,13]. Ultrasonography is able to see that the cysts are either anechoic or hypoechoic and they have a smooth thin wall[14], whereas solid tumors are either isoechoic or hypoechoic. In addition, computerized tomography and magnetic resonance imaging may give most of the necessary information, regarding the morphology of the cyst, the composition of the cystic fluid, the location in the spleen, the position of the cyst and its relationship with the surrounding tissues[5,7,10]. Calcifications of both the primary and secondary cysts are frequently found, which are useful in diagnosing cysts from other causes of splenomegaly[5]. In our cases, ultrasonography and computerized tomography had preoperatively set the diagnosis of solitary unilocular noncalcified splenic cysts.
Due to the increased risk of complications in splenic cysts with a diameter larger than 4-5 cm should be managed surgically[9,11,15], because conservative options, such as percutaneous aspiration or sclerosis, do not result in long-term control[5,8,16]. There are different types of surgical treatment according to the patient’s age and the size, location and nature of the cyst. The classical approach to splenic cysts has been open complete splenectomy[5,8,17]. However, there was a trend towards more conservative surgery after the 1970s, because of the appearance of overwhelming life-threatening septicemia, especially in children who underwent splenectomy[5,10,18]. Indeed, the spleen plays an important role in hematopoiesis, immune function, and protection against infections and malignancies[5,19]. Today the optimal treatment options are partial splenectomy, total cystectomy, marsupialization, or cyst decapsulation (unroofing), accessed either by open laparotomy or laparoscopy[5,11,19,20,21].
Partial splenectomy preserves more than 25% of splenic parenchyma, which is the minimal splenic tissue to preserve immunologic protection without increasing the risk of recurrence[5,20]. Partial splenectomy can be performed safely with the laparoscopic approach[4,11,20,21]. This procedure is recommended, if the cyst is located in the poles of the spleen, or if the cyst cavity is deep, due to the higher risk of recurrence[5,8]. Incision of the splenic capsule and hemostasis is performed with the ultrasonic or the monopolar scissors[5,11]. A more conservative option could be a partial cystectomy (unroofing) of the cyst. However, it has yet to be determined how much of the cyst wall should be resected, and whether unroofing should be partial or radical. It is supported that as much of the cyst wall as possible should be resected to prevent reclosure of the cyst[11,15].
Marsupialization of the cyst is another conservative option recommended for superficial splenic cysts, and can be performed safely with the laparoscopic method. This approach reduces the duration of the operation and carries no risk of recurrence[5,8]. In general, the laparoscopic management of splenic cysts offers the benefits of minimally invasive surgery: minimal postoperative pain, faster recovery, shorter hospital stay, and reduced morbidity and recovery[21].
However, any type of conservative procedure is difficult to perform, if the cyst is very large, is located in the splenic hilum, or is covered completely by the splenic parenchyma (intrasplenic cyst), or if there are multiple cysts (polycystic cases): in these cases, a complete splenectomy should be performed either using the open or the laparoscopic approach[1,21,22,23].
In all our cases, the cysts were of significant size and had produced clinical manifestations. Therefore, surgical treatment was absolutely indicated. Our first and second cases have been treated earlier, when laparoscopic splenectomy was not performed routinely in our center. In both the cases, we had to treat large cysts located in the splenic hilum, whereas the splenic parenchyma consisted of a rim of tissue pushed to the periphery. Therefore, both indications were met, location and dimension, and a successful open complete splenectomy was accomplished. In both cases the cysts were proved to be true epithelial cysts.
In the third case, there was a large subcapsular cyst located in the lower pole of the spleen, and thus a laparoscopic cystectomy looked as a feasible option. A partial cystectomy was done using the monopolar scissors followed by placement of a drainage tube in the remaining cavity. In this case, histology revealed a cyst without an epithelial lining (pseudocyst), and thus recurrence is not expectable[15,24]. Since there was no history of trauma, this cyst was probably of degenerative origin. We conclude that laparoscopic partial cystectomy is considered as an adequate procedure in cysts devoid of epithelial lining[24], as was our third case. No neoplastic growth has been found in any of our cases.
In conclusion, splenic cysts larger than 5 cm or symptomatic ones should be treated surgically, trying to preserve as much of splenic parenchyma as possible. If the cyst is very large and almost completely covered by splenic parenchyma, or if it is located in the splenic hilum, complete splenectomy is recommended, because of the risk of intractable bleeding from the spleen. Partial cystectomy (unroofing) could be an acceptable procedure in the majority of other cases. The laparoscopic approach seems to be a safe procedure, having all the benefits of minimally invasive surgery.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Avital S, Kashtan H. A large epithelial splenic cyst. N Engl J Med. 2003;349:2173-2174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Safioleas M, Misiakos E, Manti C. Surgical treatment for splenic hydatidosis. World J Surg. 1997;21:374-378; discussion 378. [PubMed] |
| 3. | Reddi VR, Reddy MK, Srinivas B, Sekhar CC, Ramesh O. Mesothelial splenic cyst--a case report. Ann Acad Med Singapore. 1998;27:880-882. [PubMed] |
| 4. | Heidenreich A, Canero A, di Pasquo A. Laparoscopic approach for treatment of a primary splenic cyst. Surg Laparosc Endosc. 1996;6:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Hansen MB, Moller AC. Splenic cysts. Surg Laparosc Endosc Percutan Tech. 2004;14:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 84] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Ough YD, Nash HR, Wood DA. Mesothelial cysts of the spleen with squamous metaplasia. Am J Clin Pathol. 1981;76:666-669. [PubMed] |
| 7. | Robertson F, Leander P, Ekberg O. Radiology of the spleen. Eur Radiol. 2001;11:80-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 108] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Smith ST, Scott DJ, Burdick JS, Rege RV, Jones DB. Laparoscopic marsupialization and hemisplenectomy for splenic cysts. J Laparoendosc Adv Surg Tech A. 2001;11:243-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Trompetas V, Panagopoulos E, Priovolou-Papaevangelou M, Ramantanis G. Giant benign true cyst of the spleen with high serum level of CA 19-9. Eur J Gastroenterol Hepatol. 2002;14:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Labruzzo C, Haritopoulos KN, El Tayar AR, Hakim NS. Posttraumatic cyst of the spleen: a case report and review of the literature. Int Surg. 2002;87:152-156. [PubMed] |
| 11. | Till H, Schaarschmidt K. Partial laparoscopic decapsulation of congenital splenic cysts. A medium-term evaluation proves the efficiency in children. Surg Endosc. 2004;18:626-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Knudson P, Coon W, Schnitzer B, Liepman M. Splenomegaly without an apparent cause. Surg Gynecol Obstet. 1982;155:705-708. [PubMed] |
| 13. | Nakashima A, Nakashima K, Seto H, Kamei T, Kakishita M, Kitagawa M. Primary splenic lymphoma presenting as a large cyst. Radiat Med. 1994;12:42-45. [PubMed] |
| 14. | Siniluoto TM, Päivänsalo MJ, Lähde ST, Alavaikko MJ, Lohela PK, Typpö AB, Suramo IJ. Nonparasitic splenic cysts. Ultrasonographic features and follow-up. Acta Radiol. 1994;35:447-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Morgenstern L. Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg. 2002;194:306-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 135] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Cowles RA, Yahanda AM. Epidermoid cyst of the spleen. Am J Surg. 2000;180:227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Desai MB, Kamdar MS, Bapat R, Modhe JM, Medhekar ST, Kokal KC, Abraham P. Splenic cysts: (report of 2 cases and review of the literature). J Postgrad Med. 1981;27:251-252. [PubMed] |
| 18. | Grinblat J, Gilboa Y. Overwhelming pneumococcal sepsis 25 years after splenectomy. Am J Med Sci. 1975;270:523-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Sakamoto Y, Yunotani S, Edakuni G, Mori M, Iyama A, Miyazaki K. Laparoscopic splenectomy for a giant splenic epidermoid cyst: report of a case. Surg Today. 1999;29:1268-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Touloukian RJ, Maharaj A, Ghoussoub R, Reyes M. Partial decapsulation of splenic epithelial cysts: studies on etiology and outcome. J Pediatr Surg. 1997;32:272-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Tagaya N, Oda N, Furihata M, Nemoto T, Suzuki N, Kubota K. Experience with laparoscopic management of solitary symptomatic splenic cysts. Surg Laparosc Endosc Percutan Tech. 2002;12:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Birmole BJ, Kulkarni BK, Vaidya MM, Borwankar SS. Splenic cyst. J Postgrad Med. 1993;39:40-41. [PubMed] |
| 23. | Yagi S, Isaji S, Iida T, Mizuno S, Tabata M, Yamagiwa K, Yokoi H, Imai H, Uemoto S. Laparoscopic splenectomy for a huge splenic cyst without preoperative drainage: report of a case. Surg Laparosc Endosc Percutan Tech. 2003;13:397-400. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Losanoff JE, Richman BW, Jones JW. Laparoscopic management of splenic cysts. Surg Laparosc Endosc Percutan Tech. 2003;13:63-64; author reply 64. [PubMed] |