Published online Oct 21, 2005. doi: 10.3748/wjg.v11.i39.6225
Revised: April 1, 2005
Accepted: April 2, 2005
Published online: October 21, 2005
Retrorectal, developmental tail gut cysts, include dermoid cysts, rectal duplication cysts and retrorectal cyst-hama-rtomas. Retrorectal cyst-hamartomas (RCH) are derived from remnants of the tail gut, the most caudal part of the embryonic hind gut, which normally involutes by the 8th wk of embryonic development (3-8 mm stage). They have specific radiological and histopathological features that distinguish them from other similar formations (dermoid cysts, enteric duplication cysts and teratomas). We report a patient with adenosquamous carcinoma arising within RCH, who underwent complete resection of the cyst through anterior laparotomy, and reached complete (recurrence-free for 14 mo, so far) functional recovery. The cyst was incidentally discovered during hysterectomy 12 years ago. Diagnostic, therapeutic and histopathological aspects of this rare case are discussed. The mentioned period between diagnosis and surgical treatment suggests that RCH, given enough time, can develop malignant degeneration, and should be resected at the time of diagnosis.
- Citation: Krivokapic Z, Dimitrijevic I, Barisic G, Markovic V, Krstic M. Adenosquamous carcinoma arising within a retrorectal tailgut cyst: Report of a case. World J Gastroenterol 2005; 11(39): 6225-6227
- URL: https://www.wjgnet.com/1007-9327/full/v11/i39/6225.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i39.6225
The report was about a 47-year-old woman with a family history, where both her mother and daughter underwent surgery for presacral cysts in other institutions. Both of these cysts were benign in nature. The patient also had a positive history of obstructional bronchitis. The presacral cyst was discovered 11 years ago during hysterectomy because of myomatous uterus. Physical examination showed a fistulous opening on the perianal skin near posterior commissure with no apparent communication with the cyst. Proctoscopic examination showed posterior extrinsic compression of the rectum. Aside from these findings, there were no other abnormalities. Laboratory studies showed anemia and hypoproteinemia (RBC 2, 40?0E12/L; HGB 79 g/L; total proteins 45 g/L). Abdominal ultrasound showed no abnormalities. Transrectal ultrasound showed the tailgut cyst posterior to and causing deformity of rectal wall. The scan identifies five layers of the rectal wall of which the outer hypoechoic layer represents the muscularis propria (Figure 1). There was no radiological evidence of extrapelvic disease. After preoperative immunological testing, because of hypersensitivity to a number of drugs, she underwent complete resection of the mass through anterior laparotomy. The cystic mass was loosely connected to the lower sacrum through fibrous attachments. Communication with the opening was not established. After removal of the intact cyst, the opening on perianal skin was sutured. The patient soon reached a complete functional recovery.
Gross examination revealed irregularly shaped ovoid multiloculated cystic formation measuring 85 mm in greatest diameter (Figure 2). On cut surface, there was a large dominant cyst surrounded by number of small irregular cysts with diameter up to 15 mm, all of them showing muco-purulent content. Microscopically, a wide range of epithelial covering were represented, commonly found in gastrointestinal tract, focally eroded or displaced by respiratory-type epithelium in some areas. Ulcerated areas were surrounded with strong histiocyte infiltrate.
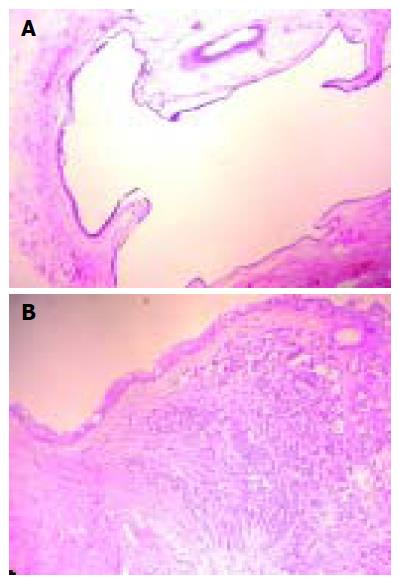
Malignant alteration of the cyst was presented as ill-defined nodular thickening (7 mm), histologically presenting adenosquamous carcinoma, mostly well-differentiated adenocarcinoma admixed with foci of squamous differentiation or poorly differentiated areas and clear resection margins (Figures 3A and B).
Retrorectal cyst-hamartomas (RCH) are reasonably rare, and they are always localized within the retrorectal space, which is bordered by rectum anteriorly, posteriorly by the sacrum, superiorly by the peritoneal reflection, inferiorly by the levator ani and coccygeus muscle, and laterally by the ureters and iliac vessels[1].
They can be found in all age groups including infancy, but they are more commonly reported in middle-aged females, and as mentioned, they are thought to arise from postnatal primitive gut remnants[2,3]
The clinical presentation of the cyst is non-specific, and it is most frequently related to a compressive effect of a growing mass within the pelvis (e.g. rectal fullness, urinary frequency, change in stool caliber, rectal bleeding)[4]
Around 50% of the cysts are discovered incidentally on routine physical examination[1]. Symptoms due to infection are also possible, and fistulous communication with the rectum or with the perianal skin can develop, often after inappropriate surgery. Recurring retrorectal abscess or recidivant perianal fistula can in fact be the infected tail gut cyst[1]
Plain radiography may show a soft tissue mass without destruction of the bone. Irigography can only confirm extramural compression of the rectum[1]. Computed tomography (CT) shows a well marginated retrorectal mass with CT numbers varying from water to soft tissue density.
Transrectal ultrasound is used to asses rectal and perirectal masses[1]. Its good sides are that it is simple, accurate and inexpensive. A diagnostic biopsy for cystic masses is not advised[4]. It may fail to confirm potential malignant diagnosis, and it carries a significant hazard of spillage of malignant cells, or may lead to the infection of the cyst.|
Malignant transformation of RCH is very rare. Prasad et al.[5], identified 10 cases of malignancy in the literature. The outcome of the treatment of these malignancies varies from case to case. The most important factors for the prognosis are the time of the diagnosis, radicality of surgical resection and histopathological diagnosis; much better prognosis is with neuroendocrine cases, than with adenocarcinomas.
Complete excision of the cyst along with the margin of normal tissue followed by careful examination of the specimen is recommended. Anterior approach, as mentioned, was used in this case. Posterior approach is used for resection of the cyst localized below the level of S4, higher lesions are addressed through anterior approach, and smaller lesions can be reached through transvaginal approach. Combined anterior and posterior pelvic approach is advised by some authors[4] in cases of malignant transformation of the cyst.
Although this case demonstrates how malignant cyst can be successfully removed, with complete functional and oncological recovery, other experiences[4] show rapid and diffuse systemic failure and it is strongly recommended to aggressively address all RCHs as early as identifiable. For the same reason, adjuvant chemotherapy should be considered in some cases at least. Other interesting aspect of this case is the possible hereditary component, which certainly needs additional investigation.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Hutton KA, Benson EA. Case report: tailgut cyst--assessment with transrectal ultrasound. Clin Radiol. 1992;45:288-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Hjermstad BM, Helwig EB. Tailgut cysts. Report of 53 cases. Am J Clin Pathol. 1988;89:139-147. [PubMed] |
| 3. | Mourra N, Caplin S, Parc R, Flejou JF. Presacral neuroendocrine carcinoma developed in a tailgut cyst: report of a case. Dis Colon Rectum. 2003;46:411-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Schwarz RE, Lyda M, Lew M, Paz IB. A carcinoembryonic antigen-secreting adenocarcinoma arising within a retrorectal tailgut cyst: clinicopathological considerations. Am J Gastroenterol. 2000;95:1344-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Prasad AR, Amin MB, Randolph TL, Lee CS, Ma CK. Retrorectal cystic hamartoma: report of 5 cases with malignancy arising in 2. Arch Pathol Lab Med. 2000;124:725-729. [PubMed] |
| 6. | Böhm B, Milsom JW, Fazio VW, Lavery IC, Church JM, Oakley JR. Our approach to the management of congenital presacral tumors in adults. Int J Colorectal Dis. 1993;8:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 63] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 7. | Madanes AE, Kennison RD, Mitchell GW. Removal of a presacral tumor via a Schuchardt incision. Obstet Gynecol. 1981;57:94S-96S. [PubMed] |
| 8. | Freier DT, Stanley JC, Thompson NW. Retrorectal tumors in adults. Surg Gynecol Obstet. 1971;132:681-686. [PubMed] |
| 9. | Abel ME, Nelson R, Prasad ML, Pearl RK, Orsay CP, Abcarian H. Parasacrococcygeal approach for the resection of retrorectal developmental cysts. Dis Colon Rectum. 1985;28:855-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Spencer RJ, Jackman RJ. Surgical management of precoccygeal cysts. Surg Gynecol Obstet. 1962;115:449-452. [PubMed] |