Published online Oct 14, 2005. doi: 10.3748/wjg.v11.i38.5984
Revised: April 15, 2005
Accepted: April 18, 2005
Published online: October 14, 2005
AIM: To investigate whether the routine use of fibrin glue applied onto the hepatic resection area can diminish postoperative volume of bloody or biliary fluids drained via intraoperatively placed perihepatic tubes and can thus lower the complication rate.
METHODS: Two groups of consecutive patients with a comparable spectrum of recent hepatic resections were compared: (1) 13 patients who underwent application of fibrin glue immediately after resection of liver parenchyma; (2) 12 patients who did not. Volumes of postoperative drainage fluid were determined in 4-h intervals through 24 h indicating the intervention caused bloody and biliary segregation.
RESULTS: Through the first 8 h postoperatively, there was a tendency of higher amounts of fluids in patients with no additional application of fibrin glue while through the following intervals, a significant increase of drainage volumes was documented in comparison with the first two 4-h intervals, e.g., after 12 h, 149.6 mL +/-110 mL vs 63.2 mL +/-78 mL. Using fibrin glue, postoperative fluid amounts were significantly lower through the postoperative observation period of 24 h (851 mL +/-715 mLvs 315 mL +/-305 mL).
CONCLUSION: For hepatic resections, the use of fibrin glue appears to be advantageous in terms of a significant decrease of surgically associated segregation of blood or bile out of the resection area. This might result in a better outcome.
- Citation: Eder F, Meyer F, Nestler G, Halloul Z, Lippert H. Sealing of the hepatic resection area using fibrin glue reduces significant amount of postoperative drain fluid. World J Gastroenterol 2005; 11(38): 5984-5987
- URL: https://www.wjgnet.com/1007-9327/full/v11/i38/5984.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i38.5984
Hepatic resections are considered as a standard intervention in abdominal surgery. Despite this, there is still a remarkable complication rate. In addition to patient-dependent factors, aspects of the surgical technique play a major role, in particular, with regard to the occurrence of postoperative bleeding and bile leakages. A precise dissection is as important as supplements such as hemostatics and tissue glue for the daily surgical practice to avoid complications, e.g., bleeding and biliary segregation from the resection area of the liver.
The aim of the study was to investigate, whether the sealing of the hepatic resection area using biocompatible glue leads to a significant decrease of postoperative release of blood and/or biliary fluid volume, which was measured in the local drainage(s).
In a pilot study, a comparative non-randomized study of two case series, all consecutive patients with hepatic resections were enrolled with prospective data documentation over a defined observational period until the planned number of individuals was reached (n = 12 per group). Patients were retrospectively (to avoid a study bias) subdivided into two groups with or without sealing of the hepatic resection area using fibrin glue. Patient characteristics are listed in Table 1.
| Fibrin glue | |||
| Without | With | ||
| Sex ratio | |||
| Patients (n) | Male | 8 | 7 |
| Female | 4 | 6 | |
| Mean age (range) (yr) | |||
| Male | 65 (3777) | 68 (4175) | |
| Female | 55 (4470) | 62 (4675) | |
Hepatic resections were carried out according to standardized technique following anatomically adequate resection margins (segmental resection, bi-/tri-segmental resection or hemihepatectomy) or as atypical hepatic resection with a tumor-free resection margin of minimally 5 mm ("wedge" resection).
Perioperative prophylaxis with antibiotics was performed (2 g of Cefotiam iv., Spizef, Grunthal GmbH, Aachen,Germany)After explorative laparotomy, definitely exclusion of extrahepatic tumor manifestation and exploration of the hepatic tumor lesion needs to be approached (if necessary including intraoperative ultrasound of liver parenchyma). The liver was mobilized in a typical manner at the "Ligg. triangularia" and "falciforme", a tourniquet loop was placed around the hepatoduodenal ligament. After marking the resection margins, dissection of liver parenchyma was carried out using cavitron ultrasonic surgical aspirator (CUSA) technology. The intraparenchymatic vessels and ducts of the biliary tree were clipped and cut. Bleeding control at the hepatic resection area was achieved by bi- and/or mono-polar electrocoagulation. During the dissection, Pringle's maneuver (temporary cessation of the blood flow in hepatic artery and portal vein) of maximally 20-min periods was executed to minimize the intraoperative blood loss. Bigger vessels and biliary ducts were ligated. After completion of the hepatic resection, the resection area was repeatedly coagulated (bi- or mono-polar electrocoagulation or infrared coagulation). Depending on the size of the resection area, one (or two) drain (s) was (were) placed into the subhepatic (and subphrenic) space.
According to the aim of the study, the hepatic resection area of the patients was sealed with fibrin glue (Tissucol or Tachocomb seal) or not.
For thrombosis prophylaxis heparin (low dose, low molecular heparin-derivative) was not given for 24 h postoperatively whereas antithrombosis socks were obligatory.
Patients were monitored at the surgical ICU for 24 h postoperatively.
Tissucol(Baxter Deutschland GmbH, Heidelberg, Germany) was applied by spraying it on the hepatic resection area. Tachocomb seal (Tachocomb, fibrin glue on a collagen fleece, Nycomed, Ismaning, Germany) was applied on the hepatic resection area after moistening it.
In the group of the patients with fibrin glue sealing, 13 patients (6 females and 7 males; mean age 62 years) with hepatic resections enrolled (Table 1), were compared with a group of 12 subjects (4 females and 8 males; mean age, 60 years) with no fibrin glue application who were enrolled in the same study period.
The diagnoses and types of resections of both groups are listed in Table 2 and Table 3.
| Diagnosis | Number of patients(sealing with fibrin glue) | |
| Without | With | |
| Hepatocellular carcinoma | 5 | 2 |
| Cholangiocellular carcinoma | ||
| Liver metastases | 5 | 9 |
| Adenoma/FNH | 2 | 2 |
| Type of resections | No. of patients(sealing with fibrin glue) | |
| Without | With | |
| Hemihepatectomy | 4 | 1 |
| Segmental resection | 4 | 10 |
| (more than one segment) | (3 bisegmental resections) | (2 trisegmental and 5 bisegmental resections) |
| Atypical resection | 4 | 2 |
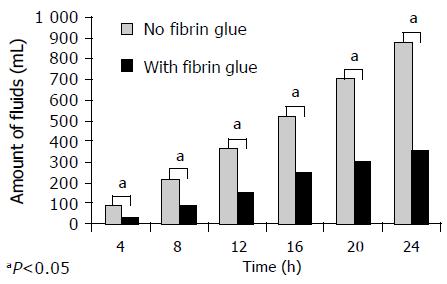
The fluid volumes drained via the intra-abdominally placed drains were documented in 4-h periods in a separate (Table 4) and additive manner (Figure 1), in total through a time period of 24 h.
| Postoperative time interval (h) | Value of significance (one side) |
| 4 | 0.0094 |
| 8 | 0.0129 |
| 12 | 0.0059 |
| 16 | 0.0054 |
| 20 | 0.0026 |
| 24 | 0.0028 |
Informed consent for hepatic resection was obtained from each patient.
In addition to the descriptively statistical presentation of the results (SPSS 10.0 for Windows), fluid volumes of the drains in both patient groups with and without sealing with fibrin glue after hepatic resection were compared by a non-parametric test according to Mann-Whitney (U test) as appropriate. A value of P<0.05 was considered statistically significant.
The mean age and sex ratio of both patient groups appeared to be comparable. The spectrum and surgical extension of hepatic resections in both groups were similar.
The listed diagnoses demonstrate the patient profile, which is treated in our center of hepatobiliary surgery and varies from primary liver tumors, cholangio- and hepatocellular carcinomas (n = 2 and n = 5 in the group with and without fibrin glue, respectively), FNH (n = 2; no fibrin glue) or hepatocellular adenoma (n = 2; no fibrin glue), to metastases of colorectal (n = 8 in the group with fibrin glue vs n = 5 without) or gastric carcinomas (n = 1; with fibrin glue, Table 2). All patients showed an acceptable preoperative liver function, and no patient showed a postoperative decompensation of liver function.
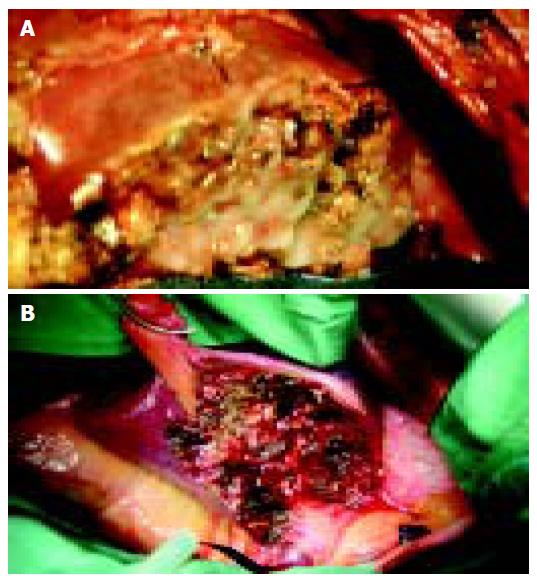
In the spectrum of resections, there were one right hemihepatectomy, 10 segmental resections (trisegmental resections, n= 2; bisegmental resections, n = 5; one segment, n = 3) and two atypical resections in the patient group with no fibrin glue application vs four hemihepatectomies, four segmental resections (bisegmental resections, n = 3; one segment, n = 1) and four atypical resections in the comparison group with fibrin glue (Table 3, Figure 2).
For sealing the hepatic resection area with fibrin glue, Tissucol® was used in 11 patients whereas in two further cases, Tachocomb® was chosen (data not shown).
In none of the patients included in the study, a severe postoperative complication occurred neither as acute nor intermediate problem. The drain fluid was either of serous or bloody-serous nature or serous quality with slight bile impurity. The comparison of the single drain volumes of both groups including the P values is shown in Table 4.
Through the first 8 h postoperatively, there was a tendency of a higher drain fluid volume in the patient group with no fibrin glue, which was indicated by the single (of each 4-h time period) as well as the added amounts of fluids (total volume at specific time points during the postoperative course). Through the following time periods, the segregation increased significantly in this group compared with the first two time periods of 4 h each, resulting in the fact that a significant reduction of the segregated volumes via the drains in the patient group with fibrin glue was observed after 12 h (P = 0.0059). This difference became even more distinct through the following time periods up to 24 h (P = 0.0028). Figure 1 shows the comparison of the added postoperative amount of fluids drained postoperatively from the hepatic resection area. While the summation of the single drain volumes of the patients with fibrin glue through the 24-h time period shows a linear curve, the curve in the comparison group (no fibrin glue) shows an exponential increase.
Using fibrin glue, a significant reduction of the postoperative drain volume of segregated fluids out of the hepatic resection area was found during the study period of 24 postinterventional hours.
By means of a pilot study, two patient groups with similar demographic and treatment characteristics were compared to investigate whether the application of fibrin glue on the hepatic resection area has a significant impact on the postoperative segregation of fluids via the drains. Using a precise surgical technique with accurate dissection of liver parenchyma, in particular, according to the anatomic margins of the liver segments, with CUSA and a subtle control of bleeding, the complication rate in hepatic resections can be kept low.
The hypothesis was that, by the mean of an additive sealing the hepatic resection area with fibrin glue, the rate of local complications such as postoperative bleeding and biliary fistulas can be reduced. As a first step to prove this hypothesis, the amounts of segregated fluid via the drain(s) was compared between the groups of patients with or without application of fibrin glue on the hepatic resection area despite complete control of bleeding and biliary excretion occurred immediately after accomplishing the resection. It showed a significant difference with lower volumes of segregated fluids after 24 h, indicating a further possible reduction of the surgical risk and complication rate, which can be achieved by the use of fibrin glue. However, the main result of this pilot study needs to be confirmed in a currently ongoing study, in which more patients are being included.
The possible impact of a heparin medication was excluded by the department-specific standard since the continuation of the preoperatively initiated heparin administration for antithrombotic prophylaxis was postponed by 24 h postoperatively according to the duration of the study period[1]. In addition, acetylsalicylic acid-based medication was stopped a couple of days prior to the admission. The pathophysiological background to use postinterventional sealing with fibrin glue is as follows: hepatic resection can lead to an activation of fibrinolysis. Even in the case of a perfect hepatic resection from a technical point of view, postoperative bleeding and segregations of fluids can occur though the resection that was accomplished by leaving a dry hepatic resection area[2]. By the mean of fibrin application, the hepatic resection area can be sealed and, thus, smallest microlesions can be closed. In addition, the fibrin excess can avoid early fibrinolysis.
One limitation of the study might be the possibly varying size of the hepatic resection area but which is, because of the similar spectrum of different types of hepatic resections, almost comparable. In addition, the underlying liver disease might affect the drain volume, which cannot be satisfyingly clarified in this study, which included only a limited number of patients. Furthermore, following studies need to focus on the composition of the segregated fluid with regard to the content of hemoglobin and bilirubin and the discrimination between the various types of sealing (Tissucol vs Tachocomb), which has not been the main focus and can be considered as an acceptable approximation in this pilot study.
From a technical point of view, the fast availability of the fibrin-coated collagen fleece seems to be advantageous as compared with the fibrin glue, which needs to be thawed[3].
There is a varying opinion on the additive use of fibrin glue in several surgical departments. In a Japanese study, 231 hospitals were asked about their routine use in hepatic resections. While in 203 hospitals, CUSA was used for resection (87%), only 135 (60%) applied fibrin glue on the hepatic resection area after the resection[4]. Comparison studies on the use of fibrin glue in hepatic resections were undertaken using animal experiments. The difficulty in the judgment of the fibrin effect was the usage of various additional agents, the different experimental designs, and varying animal strains and species. Davidsonshowed the advantage of a sealing with fibrin glue and cellulose gauze application after hepatic resections with regard to a tendency of a lower rate of postoperative bleeding using a pig model[5].
Turner has described the advantage of a composition consisting of thrombin and autologous plasma for control of bleeding after hepatic resections in sheep[6]. In addition, Martis has reported the benefit of Tachocomb in hepatic resections of dogs[7].
In conclusion, the presented pilot study in a clinical setting supports the thesis that an additional application of fibrin glue can contribute to the safe postoperative outcome as shown by the impressive statistically significant reduction of the postoperative volumes of segregated fluids via the perihepatic drain (s). Following studies using a prospective randomized study design, in a greater number of patients, and on various aspects such as the postoperative complication rate in patients with and without fibrin glue on the hepatic resection area may result in further facts and arguments for the impact and the beneficial effect of this additional tool.
We are grateful to Dr. Kropf, Institute for Biometry and Medical Informatics, University Hospital, Magdeburg, for appropriate statistical advice. For critical prereview of the manuscript, we thank M Reymond.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Lippert H, Scheele J. Lebertumoren. ) Praxis der Chirurgie, Allgemein- und Viszeralchirurgie. 1st ed. Stuttgart, New York: Thieme 1998; 549-562. |
| 2. | Kockerling F, Schneider C, Scheidbach H, Hohenberger W. Stellenwert der Fibrinklebung in der Leberchirurgie. ) Leberchirurgie. 1st ed. Heidelberg, Leipzig: Johann Ambrosius Barth 1999; 103-108. |
| 3. | Ringe B. Gewebeklebung in der hepatobiliren und Transplantationschirurgie. ) Gewebeklebung in der Chirurgie: Grundlagen und Anwendung. 1st ed. Stuttgart, New York: Thieme 2001; 63-75. |
| 4. | Nakajima Y, Shimamura T, Kamiyama T, Matsushita M, Sato N, Todo S. Control of intraoperative bleeding during liver resection: analysis of a questionnaire sent to 231 Japanese hospitals. Surg Today. 2002;32:48-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Davidson BR, Burnett S, Javed MS, Seifalian A, Moore D, Doctor N. Experimental study of a novel fibrin sealant for achieving haemostasis following partial hepatectomy. Br J Surg. 2000;87:790-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Turner AS, Parker D, Egbert B, Maroney M, Armstrong R, Powers N. Evaluation of a novel hemostatic device in an ovine parenchymal organ bleeding model of normal and impaired hemostasis. J Biomed Mater Res. 2002;63:37-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Martis G, Mikó I, Szendröi T, Kathy S, Kovács J, Hajdu Z. Results with collagen fleece coated with fibrin glue (TachoComb). A macroscopical and histological experimental study. Acta Chir Hung. 1997;36:221-222. [PubMed] |