Published online Sep 14, 2005. doi: 10.3748/wjg.v11.i34.5416
Revised: April 1, 2005
Accepted: April 2, 2005
Published online: September 14, 2005
A diagnosis of intestinal diverticulosis is difficult to make pre-operatively because the clinical symptoms are usually non-specific. We report the case of a 70-year-old man who had suffered from three episodes of intestinal obstruction in 1 year. He experienced dull pain and a sensation of fullness over the whole abdomen. The symptoms did not improve after conservative treatment. The presumptive diagnosis was intestinal obstruction, and an exploratory laparotomy found diverticulosis of the proximal jejunum, with an adhesion band formed from the base of one diverticulum. Strangulation of a segment of the jejunum resulted from the internal herniation caused by the band. The band was removed and the proximal jejunum segmentally resected. His postoperative course was uneventful.
- Citation: Lin CH, Hsieh HF, Yu CY, Yu JC, Chan DC, Chen TW, Chen PJ, Liu YC. Diverticulosis of the jejunum with intestinal obstruction: A case report. World J Gastroenterol 2005; 11(34): 5416-5417
- URL: https://www.wjgnet.com/1007-9327/full/v11/i34/5416.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i34.5416
The incidence of acquired jejunal diverticulosis varies from 0.2% to 1.3% in autopsy studies to 2.3% when assessed on enteroclysis. The clinical presentation is normally asymptomatic and it is usually diagnosed incidentally on laparotomy. Complications may include perforation, hemorrhage, enterolith formation, diverticulitis, and intestinal obstruction. Enterolith formation is the most common complication and intestinal obstruction is rare. An adhesion band, arising from the base of one of the diverticula, may be formed after repeated diverticulitis, and may cause strangulation of the intestine. We report a rare case of diverticulosis of the jejunum with an adhesion band resulting in intestinal obstruction.
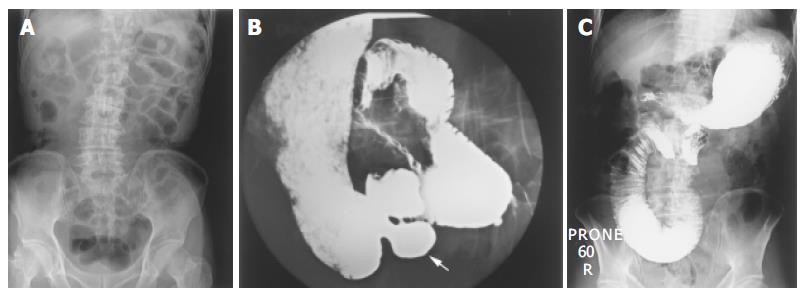
A 70-year-old male was admitted to our emergency department with dull abdominal pain and no passage of stools for 3 d. He reported a sensation of fullness over the whole abdomen and nausea. He had previously been admitted to our hospital thrice in 1 year with partial intestinal obstruction. An abdominal examination showed a diffuse tympanic sound, with percussion and tenderness over the whole abdomen. Laboratory tests indicated a white-cell count of 4 800/μL, and normal serum sodium (136 mmol/L) and potassium levels (3.8 mmol/L). A plain X-ray of the abdomen showed dilatation of the small intestine, especially in the proximal jejunum (Figure 1A). An upper gastrointestinal (GI) oral contrast study showed multiple diverticula in the proximal jejunum and a mechanical obstruction of the proximal jejunum (Figure 1B). The presumptive diagnosis was partial intestinal obstruction and the patient was admitted. After admission, nasogastric tube decompression was performed. The sensation of abdominal fullness was persistent 3 d later. An exploratory laparotomy revealed minimal clear ascites and diverticulosis of the proximal jejunum and an adhesion band with a dilated proximal jejunum (Figure 2). Segmental resection of the proximal jejunum (20 cm in length) with end-to-end jejuno-jejunostomy was performed. The final pathological diagnosis was diverticulosis of the jejunum with serosal fibrosis, hemorrhage, calcification, and inflammatory change.
The patient had an uneventful post-operative course and was discharged 8 days after the procedure.
Diverticulosis of the small bowel (excluding Meckel’s diverticulosis) is uncommon, and is found in less than 5% of post-mortem examinations[1]. It is caused by herniation of the mucosa and submucosa through the muscular layer of the bowel wall (false diverticula). Diverticula are usually multiple and occur at the mesenteric border, in contrast to the true congenital Meckel’s diverticulum. The probable cause of diverticulosis of the small bowel is motor dysfunction of the smooth muscle or the myenteric plexus in the small bowel. If contraction of the affected small intestine is disordered, it may increase the intraluminal pressure, and the mucosa and submucosa would pass through the weakest mesenteric site in the bowel wall[3]. This condition is usually asymptomatic and is found incidentally. Most patients have chronic abdominal pain and a bloated sensation. Complications include hemorrhage, perforation, diverticulitis, and intestinal obstruction. Mechanical intestinal obstruction occurs in 2.3-4.6% of cases of jejuno-ileal diverticulosis, and is reported to be the most frequent complication of jejunal diverticula requiring surgery[3-6]. Previous cases of intestinal obstruction associated with intestinal diverticulosis include distended diverticula, inflammatory mass associated with diverticulitis, stricture or adhesions from recent or past diverticulitis, and intussusception at the site of the diverticulum, most of which are caused by enteroliths[3]. The obstruction is induced by adhesion band rarely, as it occurred in our case.
Lobo et al[2] reported that dynamic intestinal obstruction is the most frequent complication of jejunal diverticulosis necessitating surgery and may be due to enteroliths, adhesions secondary to diverticulitis, volvulus, or intussusception.
This is the first report of strangulation of the jejunum caused by a mesodiverticular band in the literature. The band may have formed during recurrent diverticulitis, because it arose from the mesodiverticulum. Although this phenomenon is rare, we should keep in mind that intestinal diverticulosis may induce intestinal obstructions of different kinds, repeat physical examinations and X-ray films are needed and enteroclysis studies or CT scan are helpful in diagnosis. Surgery is indicated for acute abdominal or repeated intestinal obstruction.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Hayee B, Khan HN, Al-Mishlab T, McPartlin JF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003;9:883-884. [PubMed] |
| 2. | Lobo DN, Braithwaite BD, Fairbrother BJ. Enterolith ileus complicating jejunal diverticulosis. J Clin Gastroenterol. 1999;29:192-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 56] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Fronticelli CM, Bellora P, Ferrero A, Anselmetti GC, Passarino G, Burlo P. Complicated jejunal diverticulosis: report of a case. Surg Today. 1996;26:192-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Chiu KW, Changchien CS, Chuah SK. Small-bowel diverticulum: is it a risk for small-bowel volvulus? J Clin Gastroenterol. 1994;19:176-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Palder SB, Frey CB. Jejunal diverticulosis. Arch Surg. 1988;123:889-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 1.4] [Reference Citation Analysis (0)] |