Published online Sep 14, 2005. doi: 10.3748/wjg.v11.i34.5398
Revised: February 13, 2005
Accepted: February 18, 2005
Published online: September 14, 2005
Colonoscopic diagnosis of asymptomatic early acute appendicitis is exceedingly rare. Although obstruction of the lumen due to various causes is believed to be the most common physiologic mechanism of acute appendicitis, all of the previously documented cases in the literature have only shown a patent appendiceal lumen with pus flowing into the cecum. We present the case of a patient undergoing colonoscopy for colorectal cancer evaluation with no abdominal symptoms. An obstructed, swollen appendix was seen. The process was probably initiated during the colonoscopy, documenting perhaps the earliest stage of acute appendicitis for the first time. Endoscopic, CT and microscopic documentation of the case is also presented.
- Citation: Petro M, Minocha A. Asymptomatic early acute appendicitis initiated and diagnosed during colonoscopy: A case report. World J Gastroenterol 2005; 11(34): 5398-5400
- URL: https://www.wjgnet.com/1007-9327/full/v11/i34/5398.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i34.5398
Colonoscopic diagnosis of asymptomatic early acute appendicitis is exceedingly rare. Acute appendicitis has been described as a complication of colonoscopy[1-4]. Although obstruction of the appendiceal lumen due to various causes is believed to be the most common physiologic mechanism of acute appendicitis, the few endoscopically documented cases thus far have demonstrated a patent appendiceal lumen with pus flowing out. An obstructed appendix has not been documented earlier in the literature. We describe a case of a patient undergoing colonoscopy for evaluation of colorectal cancer that demonstrated an obstructed, swollen appendix, which is the earliest stage of acute appendicitis.
WT is a 53-year-old Caucasian gentleman who presented to our endoscopy suite for colonoscopic evaluation for colon cancer. Pre-colonoscopic evaluation did not reveal any abdominal pain, fever, chills, night sweats, nausea, vomiting, change of appetite, anorexia, hematemesis, diarrhea, constipation, hematochezia or melena. His past medical history was significant only for positive hepatitis C virus antibody. He had no past surgical history. His family history was negative for gastrointestinal cancer and polyps. His physical exam revealed a healthy Caucasian male in no acute distress with normal vital signs. Cardiovascular and pulmonary findings were within normal limits. Abdominal exam revealed normal active bowel sounds in all four quadrants. His abdomen was soft, without any evidence of tenderness or peritoneal signs.
He underwent an uneventful colonoscopy with one diminutive polyp removed with cold biopsy forceps in the ascending colon during the insertion phase. Once the cecum was reached, a mildly erythematous and markedly edematous appendiceal orifice was seen with the appendix bulging into the cecal lumen (Figure 1). The cecum was quickly deflated and the scope was withdrawn.
Surgical consultation was immediately requested. A complete blood count performed following the colonoscopy revealed a WBC count of 11.5 K with 70% segmented neutrophils and no bands.
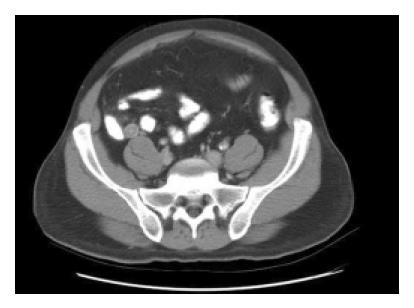
The patient was admitted to the hospital. Although he felt well initially, later that afternoon he developed some tenderness at McBurney’s point. A computed tomography scan of the abdomen revealed an enlarged appendix that was 1.6 cm in total diameter with a thickened appendiceal wall measuring 6 mm (Figure 2). There were no fluid collections or strands around the appendix.
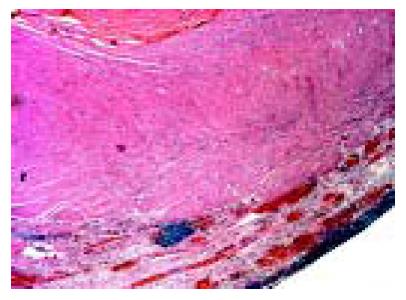
He underwent an uneventful open appendectomy post-colonoscopy and the intraoperative findings were consistent with mild, early acute appendicitis. Microscopy demonstrated very early, mild, acute appendicitis (Figure 3). There was acute mucosal inflammation with some necrosis, mild acute inflammation of the muscularis mucosa (less neutrophils than are typically seen with appendicitis), and mild acute serosal inflammation. The lumen had some pus in it. No perforation was seen. The patient did well and was discharged the next day.
Our case represents a unique situation of where appendicitis was diagnosed and probably initiated during the colonoscopy, thus documenting perhaps the earliest stage of the pathologic process.
Obstruction of the appendix is believed to be the inciting event for the development of acute appendicitis. In young patients, lymphoid follicular hyperplasia is the main cause. This process is either initiated or exacerbated by an infectious event. In elderly patients, obstruction is more likely to be caused by fibrosis, stool, or neoplasia. In endemic areas, parasites as benign as Enterobius vermicularis may be the culprit.
Since the only cases reported in literature have showed a patent lumen, it appears that the early obstructed appendix may follow either of the two courses. The appendix may continue to be obstructed which then leads to perforation and abscess formation or rather benign course occurs where the obstruction is relieved as the infection progresses resulting in pus flowing intraluminally into the cecum. This is consistent with the postulate advanced by some authors that some people with acute appendicitis may not have any symptoms, if the pus drains into the cecum and they do not develop serositis. These cases may be self-limiting or result in recurrent or chronic appendicitis[5].
In patients undergoing colonoscopy, the obstruction may occur in the preparation phase during aggressive catharsis or rarely even during the actual procedure. We believe the inciting event in our case may have been that the fecal material was forced into the appendix by the air insufflation, although we do not have any direct evidence. This is supported by the following facts: (1) the symptoms of appendicitis appeared after the colonoscopic diagnosis; (2) WBC count was borderline normal without any left shift; and (3) even though surgery occurred almost 12 h after the colonoscopic diagnosis, a mild acute appendicitis was noted during surgery as well as on histopathology. The other etiologic possibilities include de novo or coincidental infection or the irritation by cathartics used for colonic cleansing.
Development of acute appendicitis following colonoscopy has been described as a rare complication of this procedure[1-4]. One such case describes an appendiceal colic, due to probable inspissation of fecal material into the lumen of the appendix during insufflation of air in the cecum.
The diagnosis is primarily clinical with supporting laboratory and CT findings. A false negative rate of about 10-15% still persists although it has declined somewhat with the advent of newer imaging modalities. The role of colonoscopy has been determined to be possibly useful in the diagnosis of appendicitis in patients with symptoms atypical for appendicitis and/or with nondiagnostic imaging studies[5].
There has also been a reported case of a patient presenting with atypical symptoms in whom appendicitis was both diagnosed and treated during colonoscopy by insertion of a catheter into the appendiceal orifice to drain the pus[6]. An elective appendectomy was then performed 5 mo later, after all the symptoms had resolved. The histopathology of the resected appendix showed fibrous thickening of the appendiceal wall correlating with an old inflammatory process, along with changes typical for acute ulcero-phlegmonous appendicitis.
Colonoscopic diagnosis of acute appendicitis has been reported in the literature of patients with atypical symptoms associated with right lower quadrant pain, and/or non-diagnostic imaging. In one case, a mildly inflamed and erythematous cecum was seen with pus exuding from an edematous appendiceal orifice[7]. Another paper documented an appendix bulging into the cecum with frank pus flowing from the orifice[8]. Histopathology revealed acute inflammation limited primarily to the lumen and mucosa, which was mostly ulcerated, with an inflammatory infiltrate in the lumen. Earlier, we had described an endoscopic view of appendicitis similar to others[9]. However, the appearance was different from the one we are demonstrating now, i.e., an obstructed/ impacted appendix not previously endoscopically documented in the literature.
Chronic appendicitis has also been diagnosed incidentally by colonoscopy[10,11]. The patient had right lower quadrant abdominal pain for 2 wk prior to colonoscopy. The colonoscopy revealed an inflamed appendiceal orifice. Neither pus nor obstruction was described and it was thought to be low grade appendicitis. She was treated conservatively with a course of metronidazole and discharged. Her symptoms persisted and she gradually became worse over the next 5 wk and an appendectomy was performed. Histology showed an abscess arising in an acquired appendiceal diverticulum and connecting with the lumen of the appendix. The appendix itself showed changes consistent with chronic appendicitis.
In conclusion, we have endoscopically documented for the first time an early obstructive phase of acute appendicitis. Endoscopists need to be aware of the potential for appendicitis during colonoscopy and its appearance, so that prompt appropriate management can be initiated.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Srivastava V, Pink J, Swarnkar K, Feroz A, Stephenson BM. Colonoscopically induced appendicitis. Colorectal Dis. 2004;6:124-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Kapral C, Wewalka F, Kopf C, Aufreiter M, Lenz K. Acute appendicitis after colonoscopy: causality or coincidence? Z Gastroenterol. 2003;41:999-1000. [PubMed] |
| 3. | Hirata K, Noguchi J, Yoshikawa I, Tabaru A, Nagata N, Murata I, Itoh H. Acute appendicitis immediately after colonoscopy. Am J Gastroenterol. 1996;91:2239-2240. [PubMed] |
| 4. | Vender R, Larson J, Garcia J, Topazian M, Ephraim P. Appendicitis as a complication of colonoscopy. Gastrointest Endosc. 1995;41:514-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Houghton A, Aston N. Appendicitis complicating colonoscopy. Gastrointest Endosc. 1988;34:489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Chang HS, Yang SK, Myung SJ, Jung HY, Hong WS, Kim JH, Min YI, Ha HK, Kim JC, Yu CS. The role of colonoscopy in the diagnosis of appendicitis in patients with atypical presentations. Gastrointest Endosc. 2002;56:343-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Said M, Ledochowski M, Dietze O, Simader H. Colonoscopic diagnosis and treatment of acute appendicitis. Eur J Gastroenterol Hepatol. 1995;7:569-571. [PubMed] |
| 8. | Triadafilopoulos G. Acute appendicitis. Gastrointest Endosc. 2001;54:624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 9. | Kaushik N, Krasinskas A, Slivka A, McGrath K. Acute appendicitis. Gastrointest Endosc. 2004;60:102-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Minocha A. An endoscopic view of appendicitis. N Engl J Med. 1998;339:1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Courtney ED, Melville D, Leicester RJ. Chronic appendicitis diagnosed incidentally by colonoscopy. Hosp Med. 2003;64:434-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |