INTRODUCTION
Bacteremia involving the portal venous system is well documented in patients with inflammatory bowel disease (IBD)[1,2]. While studies of patients with ulcerative colitis (UC) suggest an increased incidence of portal bacteremia[1,2], the development of liver abscesses in these patients is relatively rare[3,4]. Only six such cases have been reported so far[5].
Cytomegalovirus (CMV) infection has been implicated in cases of refractory IBD[6,7], and can complicate severe steroid-resistant UC[8,9]. CMV infection characteristically forms discrete ulcers in the colon that can be seen during colonoscopy and may provide a clue to the diagnosis of this infection in UC patients[10]. The ulceration and loss of mucosal integrity that occur in CMV colitis are likely a predisposing factor for microbial invasion of the portal venous system. The subsequent development of any portal bacteremia might be related to the occurrence of liver abscesses in UC.
In this paper, we report a case of refractory UC accompanied with CMV colitis and multiple liver abscesses. To our knowledge, this is the first reported case of multiple liver abscesses that develop in the course of UC exacerbated by CMV colitis.
CASE REPORT
A 72-year-old male, with a 5-year history of repeated hospital admission for UC, was again admitted to our hospital with a month-long history of bloody diarrhea.
On admission, the patient with unremarkable vital signs complained of bloody diarrhea occurring six to ten times per day. On physical examination, his abdomen was slightly distended with normoactive bowel sounds but no tenderness, while his right upper quadrant was unremarkable. Initial laboratory studies were remarkable for a slightly elevated white blood cell count of 8 640 per microliter (normal range 3 300-8 190/μL) with 66.5% neutrophils and an elevated C-reactive protein of 0.59 mg/dL (normal<0.25 mg/dL). All other laboratory values including liver function tests, were unremarkable. Additionally, the patient had no evidence in his serum of CMV antigen pp65, and stool cultures revealed no pathogenic organisms.
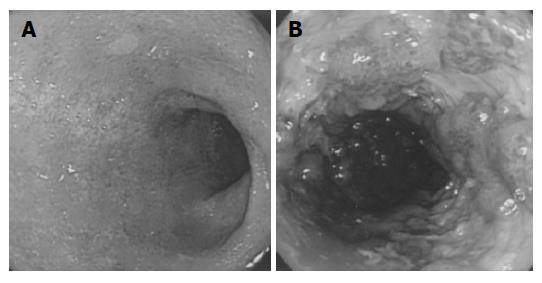
An abdominal X-ray revealed a normal bowel gas pattern, but no evidence of colonic dilatation. Abdominal computed tomography (CT) scan showed the presence of multiple liver cysts, bilateral renal cysts, and colonic inflammation extending from the distal sigmoid colon to the rectum. Sigmoidoscopy revealed diffuse mucosal edema, loss of normal vascular patterns, and friability without ulcerations in the rectum and distal sigmoid colon (Figure 1A).
Figure 1 Diffuse mucosal edema, loss of vascular pattern, and friability without ulcerations in the rectum and distal sigmoid colon (A) and multiple longitudinal ulcers and pseudopolyps in the rectosigmoid colon (B).
Initially, the patient received 30 mg prednisolone orally in addition to 2 250 mg mesalazine orally and 3 mg betamethasone enema daily. Although, this treatment resulted in temporary resolution of the diarrhea, he subsequently developed bloody diarrhea, occurring as often as 14 times per day, accompanied with tenesmus, crampy lower abdominal pain, and elevated temperatures (Lichtiger’s clinical activity index[11] was 17). Sigmoidoscopy on hospital d 18 revealed multiple longitudinal ulcers and pseudopolyps in the recto-sigmoid colon (Figure 1B). Although, colonoscopic findings suggested CMV infection in addition to UC, immunohistochemical CMV studies and serum testing for CMV antigenemia remained negative. Leukocytapheresis was initiated in addition to the other treatment; however, the patient’s bloody and watery diarrhea persisted.
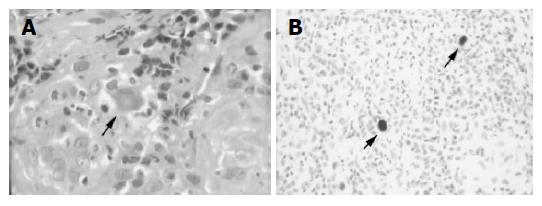
Repeat sigmoidoscopy performed in the hospital on d 29, revealed worsened progression of the previous findings. Biopsy specimens, obtained from the margin and base of the ulcers, showed CMV nuclear inclusion bodies in histiocytes (Figure 2A). Immunohistochemical staining revealed that these cells were indeed positive for CMV (Figure 2B). Moreover, the patient’s serum also became positive for CMV antigenemia. These findings suggested that CMV infection was associated with the patient’s UC exacerbation. His prednisolone was therefore gradually tapered, and ganciclovir (600 mg twice daily) was administered intravenously for 3 wk. Following the initiation of treatment with ganciclovir, his abdominal symptoms gradually resolved. After 3 wk of antiviral treatment, the Lichtiger’s clinical activity index fell from 16 (on the day before ganciclovir was started) to 5.
Figure 2 Enlarged histiocyte with Cowdry A type intranuclear inclusion body (A) and histiocytes positive for immunostaining of the CMV antigen (B).
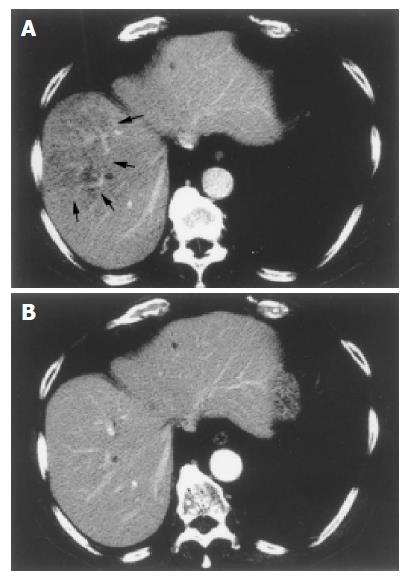
Eight days after ganciclovir was started on, the patient had a spiking temperature of 38.5 °C associated with chills. Laboratory tests revealed an increase in his white blood cell count to 1 240 per microliter with 22.5% band forms, 73.0% polymorphonuclear leukocytes, and 4.5% lymphocytes. His C-reactive protein rose to 4.95 mg/dL. A CT scan demonstrated multiple, small hypo-dense lesions in the right lobe of the liver, suggesting multiple hepatic abscesses (Figure 3A). Blood cultures were positive for Enterococcus fecalis.
Figure 3 Small hypo-dense lesions in the right lobe of the liver, suggestive of multiple liver abscesses (A) and no evidence of residual hypo-dense lesions after treatment with meropenem (B).
The patient was treated with intravenous human immunoglobulin (5 g daily) for 3 d, and 1.0 g meropenem intravenously every 12 h for 6 wk. Fever and diarrhea slowly resolved. Twenty-two days later, follow-up CT scan showed a decrease in the number of hypo-dense lesions in the liver. Another CT scan in the hospital on d 119, revealed no evidence of residual liver abscesses (Figure 3B). A colonoscopy performed in the hospital on d 120, demonstrated marked improvement in the appearance of the longitudinal ulcers. He was discharged from the hospital on the following day.
DISCUSSION
Various hepato-biliary complications are known to have an increased incidence in patients with IBD[3]. These complications include fatty changes in the liver, cholelithiasis, pericholangitis, primary sclerosing cholangitis, cirrhosis, chronic active hepatitis, amyloidosis, and bile duct cancer[3]. Even though portal bacteremia is well documented in patients with IBD[1,2], liver abscess is a rare complication[3,4]. In an epidemiological study of 1 274 UC patients in Sweden over a 25-year period, Broome et al[12] found only three cases of liver abscesses. To our knowledge, there are only six such case reports in the literature[5,12-17].
Recently, there are several reports that associate CMV infection with UC exacerbation and steroid refractoriness[6,18,19]. Several retrospective studies of UC patients undergoing proctocolectomy, document CMV anywhere from 4.6% to 13% of surgical specimens[20-22]. In a retrospective, case-control study of 80 patients, Kambham et al[8] reported that immunohistochemistry detects CMV in 10 of 40 (25%) patients with refractory UC and one of 40 (2.5%) patients with non-refractory UC. Cottone et al[9] looked at the prevalence and outcome of CMV infection in a prospective study and reported that CMV is detected in 5 out of 16 (31%) patients with refractory UC. Together, the data from these studies imply that untreated CMV infection is significantly associated with steroid-refractory UC.
Patients with IBD are at a higher risk of CMV infections, due to the following reasons: (1) the common use of immunosuppressive therapies including steroids, thiopurines, methotrexate, cyclosporine A, mycophenolate, tacrolimus, or other newer immunosuppressive agents; (2) suggested tropism for CMV at sites of inflammation and altered immunity in malnourished IBD patients[7]. Given the association of CMV infection with refractory UC, CMV infection should be ruled out with rectal biopsy and CMV serology, prior to initiating immunosuppressive therapy in UC patients presenting with exacerbation[7,8].
In the present case, we had difficulty in making a diagnosis of complicating CMV infection. Both admission immunologic testing for CMV antigen pp65 and finding from the first sigmoidoscopy did not present any evidence of a complicating CMV infection. After the patient failed to improve with initial therapy, although colonoscopic findings suggested CMV infection in addition to UC, immunohistochemical CMV studies and serum testing for CMV remained negative.
Papadakis et al[7] suggested that CMV infection should be suspected in those with systemic symptoms and signs such as high fever, dyspnea, lymphadenopathy, or splenomegaly; and in those whose bowel disease is unresponsive to steroids; as well as in those who develop worsening clinical symptoms after an initial improvement while on immunosuppression. Though the patient had multiple negative results, we were highly suspicious of CMV colitis, and repeated rectal biopsies and serum antigen testing. Treatment with steroids might be a major predisposing factor for activation of CMV. Our experience suggests that discrete and longitudinal ulcers found during colonoscopy might be indicative of CMV infection in UC patients[10].
Although portal bacteremia does occur in UC patients, the incidence of portal vein bacteremia is unknown. Manousos et al[23] and Brooke et al[24] performed portal vein blood cultures at laparotomy and noted that portal bacteremia occurs in about 25% of patients with active UC. Nonetheless very few reports on liver abscess associated with IBD are available. Song et al[5] reviewed six cases of UC reported until 2003. Approximately 30 cases of CD with liver abscess were reported until 1994[25]. Pylephlebitis, steroid administration, intra-abdominal abscesses related to the bowel, the presence of enteric fistula and perforation of the bowel are associated with the development of liver abscess[5,16,25,26]. However, the significance of these factors in UC patients remains undetermined.
Liver abscess is rare in UC patients. Treusch et al[14] and Taylor[27] suggested that the rarity may be due to the fact that the infection is a chronic one in which the body has the opportunity to throw up local barriers and produce a certain amount of systemic immunity. Song et al[5] described that considering portal bacteremia and pylephlebitis in UC patients, ulceration and loss of integrity of the normal mucosal barrier may predispose to microbial invasion of the portal venous system. The most common microorganisms that go on to cause liver abscesses are Gram-negative aerobes, such as Escherichia coli, Streptococci, Proteus species, Klebsiella species, and Enterobacter species[28]. In our patient, Enterococcus species grew in blood and stool cultures, suggesting that there might be an association between liver abscess and rectal ulcer. The time of the development of liver abscess, after steroid treatment and exacerbation of rectal ulcer, seems to indicate that CMV infection plays an important role in their development. Multiple abscesses have a higher mortality rate than single ones, probably in part related to the inability to effectively drain all sources of infection. However, in some cases, pharmacotherapy alone has produced good results[28,29]. Because of steroid treatment, we considered that he had an immunocompromised status, and then intravenous human immunoglobulin was administered. We believe that early diagnosis of CMV colitis complicating UC ultimately helps the resolution of liver abscesses. It should be considered that administration of ganciclovir and the gradual termination of steroid treatment result in remission of colitis and liver abscesses.
In conclusion, in cases of refractory UC, one should highly suspect underlying CMV infection, and early diagnosis of complicating CMV infection in UC patients may contribute to the resolution of liver abscesses and excellent clinical outcome.