Published online Sep 7, 2005. doi: 10.3748/wjg.v11.i33.5229
Revised: January 23, 2005
Accepted: January 26, 2005
Published online: September 7, 2005
We report a case of a 74-year-old woman with a 16-year history of a double bilo-enteric anastomosis due to resected hilar cholangiocarcinoma [Type IIIb Klatskin tumor]. The patient presented with cholangitis secondary to benign anastomotic stenosis which resulted in a large intrahepatic biloma. In order to restore the patency of the anastomosis and overcome cholangitis, several attempts took place, including endobiliary stenting, balloon-assisted biloplasty and transhepatic billiary drainage. Anastomotic patency was achieved, complicated, however, by persistent upper gastro-intestinal bleeding, presented as hemobilia. A biloma-induced pseudoaneurysm of the left hepatic artery was diagnosed. This had ruptured into the biliary tract, and presented the actual cause of the hemobilia. Selective embolism of the pseudoaneurysm resulted in control of the hemorrhage, and was successfully combined with transhepatic dilatation of the anastomosis and percutaneous drainage of the biloma. The patient was ultimately cured and seems to be in excellent condition, 5 mo after treatment.
- Citation: Siablis D, Papathanassiou ZG, Karnabatidis D, Christeas N, Vagianos C. Hemobilia secondary to hepatic artery pseudoaneurysm: An unusual complication of bile leakage in a patient with a history of a resected IIIb Klatskin tumor. World J Gastroenterol 2005; 11(33): 5229-5231
- URL: https://www.wjgnet.com/1007-9327/full/v11/i33/5229.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i33.5229
Bleeding into the biliary tree, either traumatic or iatrogenic, represents a rare cause of gastro-intestinal hemorrhage, which occurs in less than 3% of liver injuries[1]. Besides bleeding, typical signs of hemobilia include jaundice and pain[1,2]. Ten percent of hemobilia cases are reported to be secondary to ruptured hepatic artery aneurysms[3]. Apart from trauma and atherosclerosis, hepatic artery pseudoaneurysms may be created as a result of arterial wall erosion by local inflam-mation such as infected bilomas related to bile stasis and cholangitis[3].
In this case, we report an unusual pathological entity of an infected intrahepatic biloma secondary to a stenotic bilo-enteric anastomosis, complicated with a pseudoaneurysm of the left hepatic artery. This resulted in persistent hemobilia, which was ultimately treated by an aggressive combination of interventional radiological procedures.
Sixteen years ago, a 58 year-old woman, was operated on, due to malignant obstruction of the bile duct (Klatskin tumor, stage IIIb). At exploratory laparotomy, the tumor was resected (RO resection) and a double choledocho-jejunal anastomosis was performed (Roux-en-Y). She recovered well and was discharged 15 d later in good health. Histology of the resected specimen verified an adenocarcinoma of the bile ducts. Ever since, she has been in good condition, without evidence of tumor recurrence.
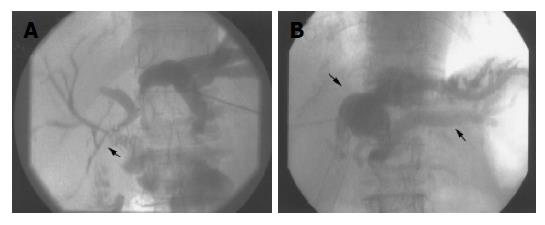
In October 2002, the patient was admitted to hospital, suffering from cholangitis. Transhepatic cholangiography demonstrated a longitudinal stenosis of the main left hepatic duct, at the area of the left bilio-enteric anastomosis, causing dilatation of the left bile ducts (Figure 1A). Considering the results of MRI as well as the long period after resection, the stenosis was finally attributed to benign postoperative fibrosis. Percutaneous balloon-assisted biliary decompression followed by transhepatic insertion of two expandable metallic stents through the bilo-enteric anastomosis resulted in clinical and radiological palliation of the cholangitis.
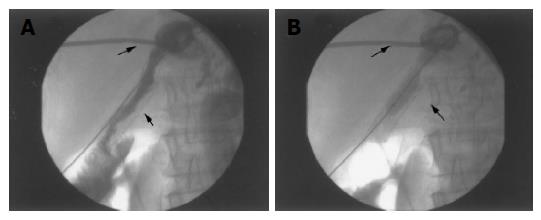
Two years later, a new severe episode of cholangitis led the patient to hospital again. Transhepatic cholangiography showed severe stenosis of the stent lumen that seemed to be secondary to endothelial hyperplasia. A nearby biloma was also depicted, due to bile leakage, probably related to bile stasis (Figure 1B). External drainage of the biloma and percutaneous transhepatic stent re-dilatation (Figures 2A and B) were performed. After receiving antibiotics for five days, the external drainage catheter was removed and the patient was discharged in acceptable clinical condition.
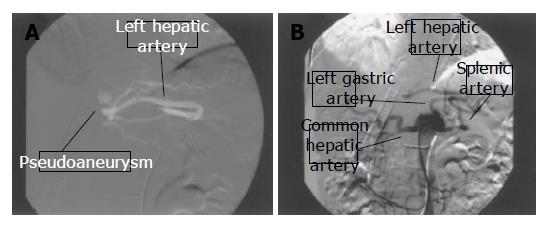
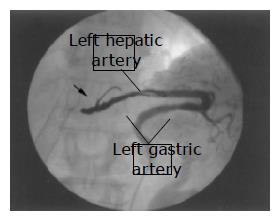
Four weeks later, the patient returned to hospital due to weakness and anemia. She reported a 10-d history of melena. Urgent endoscopy disclosed no evidence of active gastro-duodenal bleeding. Computed tomography-assisted angiography displayed an aneurysmal sac located at the left hepatic arterial tract. A subsequent catheter-directed selective angiography detected precisely a pseudoaneurysm originating from a branch of the left hepatic artery. Technically, this was a particularly demanding procedure, due to an abnormal origin of the left hepatic artery from the left gastric artery (Type II variation, according to Hiatt’s classification[4]) (Figures 3A and B). By means of super-selective catheterization, the neck of the pseudoaneurysm was approached and detachment of adequate metallic coils was performed resulting in full occlusion of the vascular lesion (Figure 4) and immediate control of the bleeding. The patient recovered well and was discharged a week later in good condition.
Five months later, the patient remained in good condition, without clinical or laboratory evidence of hemobilia or cholangitis.
Trauma (iatrogenic or accidental) and atherosclerosis consist of the most common causes of hepatic artery aneurysms[3,5], however, their formation may be less frequently encountered as a result of biliary inflammation. This is usually related to parasitic infection or stone impaction into the biliary tree[6]. The reported case suggests that other additional inflammatory factors such as infected, long lasting, intrahepatic bilomas may erode the arterial wall and lead to pseudoaneurysms.
Nonetheless, arterial injury is an unusual (2%), but possible complication of percutaneous transhepatic billiary drainaging (PTBD), which may also result in severe hemobilia[7]. The reported patient however, had been hospitalized for 5 d after PTBD and was discharged without any evidence of significant blood loss. This makes the scenario of a biloma-induced hepatic pseudoaneurysm that finally ruptures into a bile duct, more reasonable.
Hemobilia usually presents either with melena (90%) or hematemesis (72%)[1]. Other clinical manifestations include upper abdominal pain (71%) and obstructive jaundice (60%)[1]. The complete triad of bleeding, pain and jaundice is reported only in 22% of cases[1]. Hemobilia represents a potential life-threatening complication depending not only on the size of vessel wall deficit[7] but also on the fibrinolytic action of the bile that inhibits proper clot formation[1,8].
Liver angiography is the standard diagnostic method in cases of hemobilia especially, when endoscopic procedures fail to establish diagnosis[1,9]. This minimally invasive method detects precisely the bleeding site, also allowing simultaneous therapeutic intervention, by selective catheterization and embolization with the use of adequate embolic agents. Successful hemostasis rates exceed 95%[1] while procedure-associated morbidity and mortality are considerably lower than surgery[10]. The aforementioned advantages play a significant role especially in the management of patients with anatomic variations of the hepatic artery as well as for elderly patients with poor surgical prognosis, as in this case.
Apart from iatrogenic and accidental injury of the biliary tree, hemobilia may also occur under more complicated circumstances. The possibility of a biloma-induced hepatic pseudoaneurysm that finally erodes a bile duct should be taken into account, especially in patients with chronic obstructive jaundice, extra-ductal and encapsulated bile collections, repetitive episodes of cholangitis and hemobilia.
Transhepatic arterial embolization provides a safe and effective alternative in controlling patients with persistent hemobilia.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Forlee MV, Krige JE, Welman CJ, Beningfield SJ. Haemobilia after penetrating and blunt liver injury: treatment with selective hepatic artery embolisation. Injury. 2004;35:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Sandblom P, Saegesser F, Mirkovitch V. Hepatic hemobilia: hemorrhage from the intrahepatic biliary tract, a review. World J Surg. 1984;8:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Liu TT, Hou MC, Lin HC, Chang FY, Lee SD. Life-threatening hemobilia caused by hepatic artery pseudoaneurysm: a rare complication of chronic cholangitis. World J Gastroenterol. 2003;9:2883-2884. [PubMed] |
| 4. | Koops A, Wojciechowski B, Broering DC, Adam G, Krupski-Berdien G. Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg Radiol Anat. 2004;26:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 165] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 5. | Stauffer JT, Weinman MD, Bynum TE. Hemobilia in a patient with multiple hepatic artery aneurysms: a case report and review of the literature. Am J Gastroenterol. 1989;84:59-62. [PubMed] |
| 6. | Bloechle C, Izbicki JR, Rashed MY, el-Sefi T, Hosch SB, Knoefel WT, Rogiers X, Broelsch CE. Hemobilia: presentation, diagnosis, and management. Am J Gastroenterol. 1994;89:1537-1540. [PubMed] |
| 7. | L'Hermine C, Ernst O, Delemazure O, Sergent G. Arterial complications of percutaneous transhepatic biliary drainage. Cardiovasc Intervent Radiol. 1996;19:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Vagianos C, Karavias D, Dragotis C, Kalofonos H, Androulakis J. Obstructive jaundice due to intracholedochal blood clot: an unusual early presentation of primary hepatic carcinoma. Br J Clin Pract. 1993;47:222-223. [PubMed] |
| 9. | Moodley J, Singh B, Lalloo S, Pershad S, Robbs JV. Non-operative management of haemobilia. Br J Surg. 2001;88:1073-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Lygidakis NJ, Okazaki M, Damtsios G. Iatrogenic hemobilia: how to approach it. Hepatogastroenterology. 1991;38:454-457. [PubMed] |