Published online Aug 14, 2005. doi: 10.3748/wjg.v11.i30.4750
Revised: April 6, 2005
Accepted: April 11, 2005
Published online: August 14, 2005
AIM: To investigate the expression of interferon inducible protein-10 (IP-10) in pancreas of mice and to discuss its possible role in the pathogenesis of type 1 diabetes.
METHODS: Non-obese diabetic (NOD) mice were used as experiment group and BALB/c mice as non-diabetic prone model. Immunohistochemistry method was used to evaluate the expression of IP-10 in the pancreas of NOD mice and BALB/c mice. Immunoelectron microscope was used to show the location of IP-10 in pancreatic islet β cells.
RESULTS: Pancreatic islets were positively stained in all the NOD mice. Insulitis could be found in mice at the age of 4 wk. The weakly positive results were found in control group with no insulitis. Immunoelectron microscopy further demonstrated that IP-10 was produced by pancreatic β cells and stored in cytoplasm of the cells.
CONCLUSION: IP-10 can be largely produced in pancreatic islets of NOD mice at the age of 2 wk when there is no significant insulitis, and may play an important part in the pathogenesis of type 1 diabetes by attracting immune cells to infiltrate the pancreatic islets.
- Citation: Li D, Zhu SW, Liu DJ, Liu GL. Expression of interferon inducible protein-10 in pancreas of mice. World J Gastroenterol 2005; 11(30): 4750-4752
- URL: https://www.wjgnet.com/1007-9327/full/v11/i30/4750.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i30.4750
Type 1 diabetes has been recognized as an organ specific autoimmune disease due to the immune destruction of pancreatic islet β cells in genetically susceptible individuals[1]. In both human and rodent models of Type 1 diabetes, the disease has a distinct stage characterized by infiltration of immune cells in the pancreas (insulitis). The major populations of infiltrating cells are macrophages and lymphocytes. Therefore, immune cell infiltration in pancreatic islets may be a crucial step in the pathogenesis of type 1 diabetes[2]. Experiments have shown that interferon induced protein-10 (IP-10), an important member of CXC chemokine subfamily, has chemoattractant effects on monocytes and activated lymphocytes[3]. Thus, we hypothesize that IP-10 may recruit immune cells into the pancreas by binding to the chemokine receptor, CXCR4 expressed on the target cells, thus leading to type 1 diabetes. In this study, we evaluated the expression of IP-10 in the pancreas of animal model of type 1 diabetes and discussed its possible role in the pathogenesis of type 1 diabetes.
Experimental NOD mice were obtained from Shanghai Laboratory Animal Center, Chinese Academy of Sciences. Pancreatic islet infiltration of immune cells appeared and insulitis developed in the mice at the age of 4 wk. Insulitis became most serious at the age of 9-10 wk. The remaining pancreatic β cells decreased to 10% of normal levels and diabetes developed. The incidence of diabetes in female NOD mice was higher than that in males. BALB/c mice were used as non-diabetes and non-autoimmune-prone control. Blood glucose in all the mice was measured before death. If the blood glucose concentrations exceeded 300 mg/L, diabetes could be considered.
The mice were killed by decollation. Pancreases were fixed in 40 g/L formaldehyde and embedded in paraffin. Paraffin-embedded tissues were sectioned and stained with hematoxylin-eosin and analyzed by light microscopy.
Dewaxed sections were stained using streptavidin-biotin-peroxidase complex (SABC) method (Wuhan Boster Biological Technology Co., Ltd). Primary antibody was goat -anti-mouse polyclonal antibody (Santa Cruz Biotechnology, Inc.). The color of the complex was developed using 3,3’-diamino-benzidine tetrahydrochloride (DAB) kit (AR1022). The sections were counterstained with hematoxylin, dehydrated and mounted, examined microscopically.
The samples were fixed with 1% osmic acid, after the color reaction using DAB. Sections were dehydrated in graded ethanol solutions and embedded in Epon 872. Ultra-thin (70 nm) sections were made and stained with uranyl acetate, and then examined under JEM-1200EX (JEOL) electron microscope.
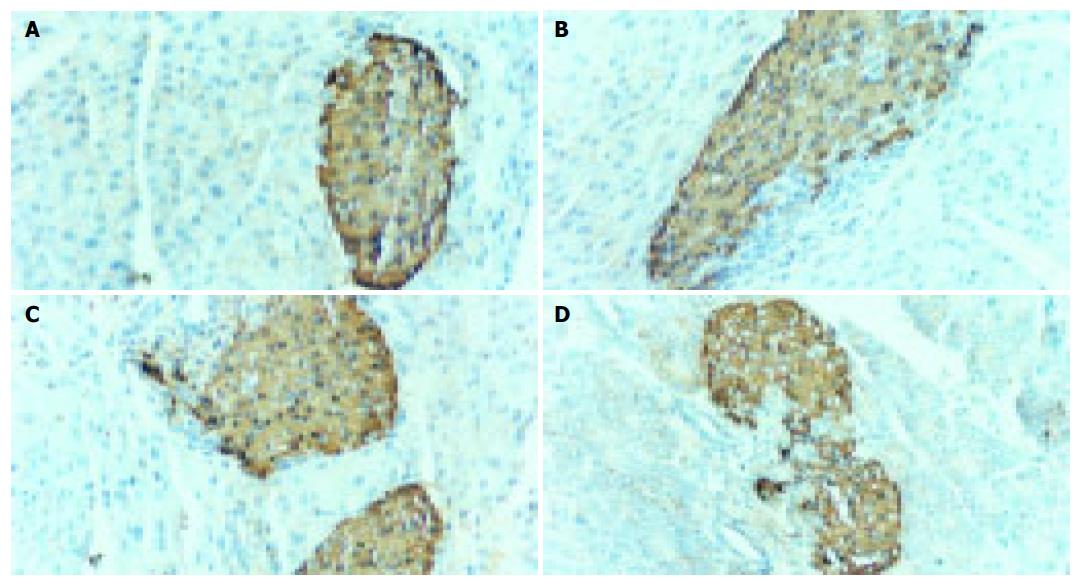
Pancreatic islets were positively stained in all NOD mice. Insulitis could be found at the age of 4 wk (Figures 1A-D)
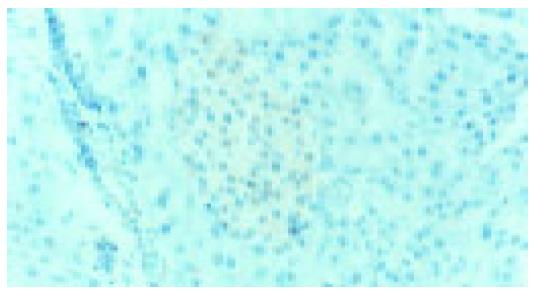
Weakly positive results were found in the pancreatic islets of BALB/c mice, which were stained light brown (Figure 2). No insulitis could be found.
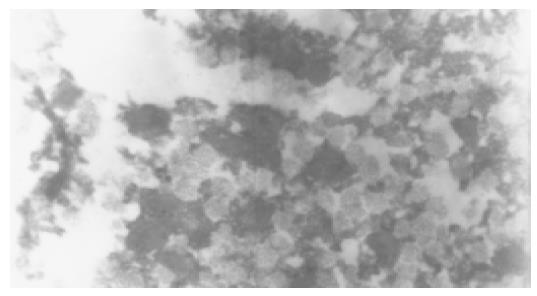
Immunoelectron microscopy demonstrated that IP-10 was produced by pancreatic β cells and stored in cytoplasm of the cells (Figure 3).
Type 1 diabetes is a chronic disease, severely affecting the health of children. Its incidence has been increasing continuously from 1980s. In both human and rodent models of Type 1 diabetes, the disease has a distinct stage characterized by immune cell infiltration in pancreas (insulitis). The major populations of infiltrating cells are macrophages and lymphocytes. Therefore, the infiltration of macrophages and lymphocytes may be a crucial step in the auto-immune response of type 1 diabetes. IP-10 is a member of CXC chemokine subfamily and has chemoattractant effects on monocytes and activated lymphocytes. Thus, we suppose that it may play an important part in the immune cell infiltration of pancreatic islets.
We demonstrated in this study that the expression of IP-10 was positive in the pancreas of both NOD mice and BALB/c mice, which agrees well with the findings of Arimilli et al.[4], suggesting that IP-10 is constitutively produced by the pancreatic islets in mice. But the production of IP-10 is small because weak expression of IP-10 has been shown in BALB/c mice, and IP-10 produced has no chemoattractant effect as no infiltration of immune cells could be found in the control group. It has long been known that chemokines have many functions in addition to chemo-attractant effect. IP-10 is involved in delayed-type allergy and the suppression of angiogenesis. Therefore, IP-10 has other biological functions in normal pancreatic tissues other than chemoattractant effect. Few studies on expressions of IP-10 in pancreas are available. The acute functions of the constitutive expressions of IP-10 in pancreatic tissues need further study. But, the pancreatic islets of diabetic mice produce high level of IP-10 and accompanied insulitis, which supports our hypothesis that abundant IP-10 can be produced in a pathological environment and attract immune cells into pancreatic tissues. Our study also proved that IP-10 could be found in the pancreatic islets of NOD mice at the age of 2 wk when there was no significant insulitis, suggesting that IP-10 is produced at the onset of diabetes. Its concentration may not be high enough to cause insulitis at first. As IP-10 accumulates, more immune cells can be recruited into the pancreatic islets and finally result in insulitis.
Viral infections and inflammatory cytokines including IL-1β and interferon-γ are important factors triggering type 1 diabetes. Double stranded RNA (dsRNA) produced by virus cooperated with IL-1β and Interferon-γ or IL-1β could induce high levels of IP-10 in human and NOD mice pancreatic β cells in vitro[5,6]. Our study also showed that IP-10 existed in the pancreatic β cells. These results indicate that pancreatic β cells can produce IP-10, and that virus and inflammatory cytokines can initiate expression of IP-10 in vivo. Pancreatic β cells are possibly one of the main sources of IP-10. It has been reported that pancreatic islet specific Th1 cells can produce IP-10 and may be another source[7].
We can speculate about the possible mechanism of viral infections causing diabetes based on the present studies. Viruses induce the expression of IP-10 in pancreatic β cells, and IP-10 is secreted into the pancreatic islets. Then, peripheral immune cells migrate into the pancreatic islets along with the IP-10 concentration gradient and result in insulitis.
Since few studies on the role of IP-10 in type 1 diabetes are available, our data are necessary to be confirmed by more studies. There is no study on the expression of IP-10 in the pancreas of patients with type 1 diabetes. Although the serum IP-10 levels in newly diagnosed patients with type 1 diabetes are much higher than those in healthy subjects[8], chemokines tend to form high concentration grade in local secretion point that attract target cells. The serum chemokine level cannot reflect the true conditions of expressions of chemokine in human pancreas.
In conclusion, IP-10 may play an important part in the pathogenesis of type 1 diabetes by attracting immune cells to infiltrate the pancreatic islets.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | Devendra D, Liu E, Eisenbarth GS. Type 1 diabetes: recent developments. BMJ. 2004;328:750-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 186] [Article Influence: 8.9] [Reference Citation Analysis (2)] |
| 2. | Atkinson MA, Eisenbarth GS. Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet. 2001;358:221-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 955] [Cited by in RCA: 924] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 3. | Atkinson MA, Wilson SB. Fatal attraction: chemokines and type 1 diabetes. J Clin Invest. 2002;110:1611-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Arimilli S, Ferlin W, Solvason N, Deshpande S, Howard M, Mocci S. Chemokines in autoimmune diseases. Immunol Rev. 2000;177:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Liu D, Cardozo AK, Darville MI, Eizirik DL. Double-stranded RNA cooperates with interferon-gamma and IL-1 beta to induce both chemokine expression and nuclear factor-kappa B-dependent apoptosis in pancreatic beta-cells: potential mechanisms for viral-induced insulitis and beta-cell death in type 1 diabetes mellitus. Endocrinology. 2002;143:1225-1234. [PubMed] |
| 6. | Cardozo AK, Proost P, Gysemans C, Chen MC, Mathieu C, Eizirik DL. IL-1beta and IFN-gamma induce the expression of diverse chemokines and IL-15 in human and rat pancreatic islet cells, and in islets from pre-diabetic NOD mice. Diabetologia. 2003;46:255-266. [PubMed] |
| 7. | Bradley LM, Asensio VC, Schioetz LK, Harbertson J, Krahl T, Patstone G, Woolf N, Campbell IL, Sarvetnick N. Islet-specific Th1, but not Th2, cells secrete multiple chemokines and promote rapid induction of autoimmune diabetes. J Immunol. 1999;162:2511-2520. [PubMed] |
| 8. | Shimada A, Morimoto J, Kodama K, Suzuki R, Oikawa Y, Funae O, Kasuga A, Saruta T, Narumi S. Elevated serum IP-10 levels observed in type 1 diabetes. Diabetes Care. 2001;24:510-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 123] [Article Influence: 5.1] [Reference Citation Analysis (0)] |