Published online Jul 21, 2005. doi: 10.3748/wjg.v11.i27.4230
Revised: December 3, 2004
Accepted: December 8, 2004
Published online: July 21, 2005
AIM: Although the radiological features of acute appendicitis have been well documented, the value of plain radiography has not been fully appreciated. The aim of this study was to determine the frequency of the association of acute appendicitis with images of fecal loading in the cecum.
METHODS: Plain abdominal radiographs of 400 patients operated upon for acute appendicitis (n = 100), acute cholecystitis (n = 100), right acute pelvic inflammatory disease (n = 100) and right nephrolithiasis (n = 100) were assessed. The presence of fecal loading was recorded and the sensitivity and specificity of this sign for acute appendicitis were calculated.
RESULTS: The presence of fecal loading in the cecum occurred in 97 patients with acute appendicitis, 13 patients with acute cholecystitis, 12 patients with acute inflammatory pelvic disease and 19 patients with nephrolithiasis. The sensitivity of this sign for appendicitis was 97% and its specificity to this disease was 85.3%. Its positive predictive value for appendicitis was 68.7%; however, its negative predictive value for appendicitis was 98.8%.
CONCLUSION: The present study suggests that the presence of radiological images of fecal loading in the cecum may be a useful sign of acute appendicitis, and the absence of this sign probably excludes this disease. This is the first description of fecal loading as a radiological sign for acute appendicitis.
- Citation: Petroianu A, Alberti LR, Zac RI. Fecal loading in the cecum as a new radiological sign of acute appendicitis. World J Gastroenterol 2005; 11(27): 4230-4232
- URL: https://www.wjgnet.com/1007-9327/full/v11/i27/4230.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i27.4230
Abdominal pain in the right lower quadrant is probably one of the most challenging problems in Medicine[1-4]. In most patients, acute appendicitis is diagnosed on the basis of clinical examination, white blood cell count, abdominal radiographic studies, and abdominal ultrasound[1-5] However, the less than perfect accuracy of these exams leads to a high rate of misdiagnosis leading to a rate of negative appendicectomies of about 15%[1,2,6,7]. In order to avoid the unnecessary removal of the appendix, other investigation methods, such as computed tomography and abdominal scintigraphy have been proposed, without real advantages[2-5].
In the presence of acute abdominal pain, abdominal radiographs are relevant and helpful, but little significance is attached to this exam in appendicitis although associated radiological features have been documented, such as localized adynamic ileum (51 - 81% of cases), increase in soft-tissue density in the right lower quadrant (12 - 33%), appendicoliths (7 - 14%) and deformity of cecum (4 - 5%)[1,5,8-10] The aim of this prospective study was to evaluate an apparently new sign present in the plain abdominal radiography of patients with acute appendicitis, i.e., images of fecal loading in the cecum. This sign was studied comparatively with other patients presenting acute right abdominal pain due to other diseases. This is the first description of fecal loading as a radiological sign for acute appendicitis.
Four hundred consecutive patients with acute right abdominal pain were prospectively studied at the Alfa Institute of Gastroenterology of the Hospital of Clinics and Hospital Julia Kubitshek between 2002 and 2004. No patient was discarded from this investigation.
Plain abdominal radiographies were obtained for all patients before treatment in order to verify the presence of fecal images in the cecum. These patients were divided into the following four groups, with 100 patients each, according to their disease.
Patients of both sexes (62 men and 38 women) ranging in age from 10 to 73 (28.3±12.2) years. All patients were operated for acute appendicitis and the diagnosis was confirmed in all cases by histologic examination of the removed appendix. Fifty of the patients with positive fecal loading in the cecum during the appendicitis period were submitted to a new plain abdominal radiography on the second postoperative day, to verify the presence of this sign after the appendicectomy.
Patients of both sexes (30 men and 70 women) ranging in age from 17 to 75 (mean 49.4 ± 16.3 years). All patients were operated for acute cholecystitis and the diagnosis was confirmed in all cases by histologic examination of the removed gallbladder. Eight of these cases presented acute cholangitis as well.
Women of the age from 20 to 45 (mean 32.3 ± 8.1 years). The complaint of these cases was due to right hydrosalpingitis (69 cases), right Fallopian pregnancy (14 cases), rupture of a right ovarian cyst (12 cases) and torsion of the right ovary (5 cases). The diagnoses were confirmed in all cases by clinical follow-up, pelvic ultrasound, laparoscopy, and surgical procedures.
Patients of both sexes (42 men and 58 women) ranging in age from 10 to 73 (43.5 ± 14.3) years. The diagnosis was confirmed in all these cases by plain abdominal radiography, urography, ultrasound and CT scan.
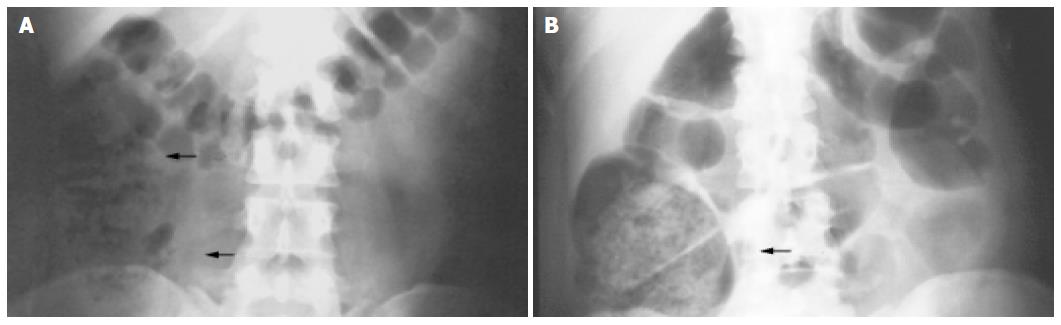
The radiological image studied was cecal intraluminal mass consisting of a mixture of soft tissue and internal gas bubble like feces, suggesting fecal impaction, or residual feces. The amount of fecal material and consequent cecal dilatation were considered.
The sensitivity and specificity of this radiological sign, as well as its positive and negative predictive values for acute appendicitis were calculated.
The present study followed the Ethics Principles of Research in Humans, according to World Medical Association Helsinki Declaration, adopted in 1964 and amended in 1996, and was approved by the Ethical Committee of the Department of Surgery of the Medical School of the Federal University of Minas Gerais, Belo Horizonte, Brazil. All exams performed on these patients are routinely employed in the presence of acute abdominal pain in the hospitals where this investigation was carried out.
Table 1 describes the presence of fecal loading in the cecum of the patients of the four groups (Figure 1A). Some of these radiographs showed cecal dilatation by the large amount of fecal mass (Figure 1B).
| Disease | Fecal loading | |||
| Present | Absent | |||
| n | (%) | n | (%) | |
| Acute appendicitis | 97 | 97 | 3 | 3 |
| Acute cholecystitis | 13 | 13 | 87 | 87 |
| Right pelvic inflammatory disease | 12 | 12 | 88 | 88 |
| Right nephrolithiasis | 19 | 19 | 81 | 81 |
The sensitivity of this sign was 97% for acute appendicitis, 13% for acute cholecystitis, 12% for right acute pelvic inflammatory disease and 19% for right nephrolithiasis. The specificity of fecal loading in the cecum for acute appendicitis was 85.3%. The positive predictive value of this sign for acute appendicitis was 68.7%; however, its negative predictive value for appendicitis was 98.8%.
On the second postoperative day, only two of the 50 patients with previous positive radiological sign preserved the fecal loading in the cecum. In the other 48 patients, this sign disappeared from the cecum.
Although a few studies have suggested that plain abdominal radiography is not helpful anymore in patients with acute abdominal pain, its indiscriminate use remains the rule in most emergency units[6,8,9-11]. However, the radiological signs described in the literature are not constant or characteristic of appendicitis. Recent investigations have called into question the value of routine use of plain abdominal radiography in patients with suspected appendicitis[1,3,4,9]. Many physicians consider ultrasound studies as standard in acute abdominal pain, believing the impact of radiograph is not of value.
In this prospective study, the association of acute appendicitis with images of fecal loading in the cecum had a sensitivity of 97% and a specificity of 85.3% when compared with other common causes of acute right abdominal pain. This rate is higher than the frequency of other clinical, laboratory, or radiological signs associated with acute appendicitis.
Another important result of the present study is based on the predictive value. According to these data, the possibility of appendicitis in the presence of fecal loading in the cecum is 68.7%. However, the absence of this sign practically excludes the diagnosis of appendicitis, which may occur in only 1.2% of cases.
We could not understand the pathophysiology to answer why appendicitis could lead to fecal loading in the cecum. However, we believe it is worth supposing that this sign may be related to a local ileum of the cecum with stool, which occurred in the presence of an acute inflammatory condition. This is the first description of fecal loading as a radiological sign for acute appendicitis.
In conclusion, the results of the present work suggest that the presence of images of fecal loading in the cecum on plain abdominal radiographs may be a useful sign associated with acute appendicitis. This association should be emphasized, mainly considering that this sign is rare in the presence of other acute inflammatory abdominal diseases and disappears when the inflamed appendix is removed.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Boleslawski E, Panis Y, Benoist S, Denet C, Mariani P, Valleur P. Plain abdominal radiography as a routine procedure for acute abdominal pain of the right lower quadrant: prospective evaluation. World J Surg. 1999;23:262-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215:337-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 343] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 3. | Sivit CJ. Imaging the child with right lower quadrant pain and suspected appendicitis: current concepts. Pediatr Radiol. 2004;34:447-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Hayes R. Abdominal pain: general imaging strategies. Eur Radiol. 2004;14 Suppl 4:L123-L137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Rao PM, Rhea JT, Rao JA, Conn AK. Plain abdominal radiography in clinically suspected appendicitis: diagnostic yield, resource use, and comparison with CT. Am J Emerg Med. 1999;17:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Thorpe JA. The plain abdominal radiograph in acute appendicitis. Ann R Coll Surg Engl. 1979;61:45-47. [PubMed] |
| 7. | Petroianu A, Oliveira Neto JE. Prevalence of acute appendi-citis in a mixed population. Dig Surg. 1997;14:195-197. [DOI] [Full Text] |
| 8. | Shimkin PM. Radiology of acute appendicitis. AJR Am J Roentgenol. 1978;130:1001-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Shorvon PJ. Imaging of appendicitis: a cautionary note. Br J Radiol. 2002;75:717-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Shelton T, McKinlay R, Schwartz RW. Acute appendicitis: current diagnosis and treatment. Curr Surg. 2003;60:502-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Petroianu A, Oliveira-Neto JE, Alberti LR. [Comparative incidence of acute appendicitis in a mixed population, related to skin color]. Arq Gastroenterol. 2004;41:24-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |