Published online Jun 21, 2005. doi: 10.3748/wjg.v11.i23.3636
Revised: June 9, 2004
Accepted: July 22, 2004
Published online: June 21, 2005
AIM: To elucidate the role of endoscopic sphincterotomy (EST) in the treatment of acute pancreatitis.
METHODS: Ninety patients with acute pancreatitis were randomly divided into two groups: EST group and control group. All the patients underwent pancreatitis routine therapy, additionally the EST group was treated with EST and endoscopic naso-bile drainage (ENBD).The time of disappearance of abdominal symptoms and signs, normalization of amylase, hospitalization and absorption of acute fluid was recorded for all patients.
RESULTS: The time of disappearance of abdominal pain, normalization of blood and urine amylase and hospitalization was significantly shorter in EST group than in control group. The ratios of disappearance of fluid in mild acute pancreatitis patients was significantly higher in EST group (51.52%, 84.85%, 90.91%,93.94%) than in the control group (0%, 30.30%, 69.70%, 72.73%, P<0.01 or P<0.05). When the ratios of reduction of fluid in severe acute pancreatitis patients of the EST group were compared (8.33%, 58.33%, 83.33%, 91.67%) with those in the control group (0%, 8.33%, 25% and 41.67%), there were significant differences.
CONCLUSION: The effect of EST+ENBD on acute pancreatitis with fluid is rather good.
- Citation: Chen WX, Li YM, Gao DJ, Xiang Z, Yu CH, Xu GQ, Ji F. Application of endoscopic sphincterotomy in acute pancreatitis with fluid collection: A prospective study. World J Gastroenterol 2005; 11(23): 3636-3639
- URL: https://www.wjgnet.com/1007-9327/full/v11/i23/3636.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i23.3636
Pancreatic fluid is a very frequent finding in acute pancreatitis patients. Bradley[1] believed that peripancreatic fluid often occurs at the early period of acute pancreatitis because of necrosis of pancreas and peripancreatic tissue. Some pancreatic fluid spontaneously disappear and can be drawn with a fine needle guided by ultrasonogram or CT. To observe the effect and security of EST and ENBD for acute pancreatitis with fluid collection, we prospectively analyzed 90 such cases of acute pancreatitis with fluid in our hospital.
Ninety patients were diagnosed with acute pancreatitis under the diagnostic criteria set by surgical pancreatic group of the Surgical Society of Chinese Medical Association. At the same time, they were diagnosed as mild acute pancreatitis with APACHE-II scores <8, Ranson criterions <3, Balthazar CT graded as B or C, and severe acute pancreatitis with the APACHE-II scores ≥8, Ranson criterions ≥3, Balthazar CT graded as D or E. All patients were randomly divided into two groups: EST group and control group. There were 45 cases in EST group, with average age of 52.52±15.96 years, 28 males and 17 females. In control group there were 45 cases too, with average age of 49.12±14.31 years, 30 males and 15 females. No significant differences of gender and age were found between two groups (P>0.05). There were 33 cases of mild acute pancreatitis and 12 cases of severe acute pancreatitis in EST group and in control group respectively. The etiological diagnoses are summarized in Table 1.
| Etiology | EST n (%) | Control n (%) |
| Biliary | 36 (80.00) | 35 (77.78) |
| Diet-induced | 3 (6.67) | 4 (8.89) |
| Alcohol-related | 2 (4.44) | 1 (2.33) |
| Strictures in intraduct of pancreas | 1 (2.22) | 0 (0) |
| Idiopathic | 3 (6.67) | 5 (11.11) |
Pancreatic fluid was detected by computerized tomography (CT). Balthazar CT grades in two groups are summarized in Table 2.
| Grades | EST n (%) | Control n (%) |
| B | 11 (24) | 14 (31) |
| C | 22 (49) | 19 (42) |
| D | 3 (7) | 4 (9) |
| E | 9 (20) | 8 (18) |
All of the two groups received fasting, infusion, prophylactic application of antibiotics and somatostatin. CT was done in all patients 24 h after admission. The size, shape and fluid of pancreas were recorded. And EST group received extra treatment of ERCP, EST[2,3] and ENBD which were done with side-viewing endoscope (Olympus-JF240). After the endoscope was advanced into the descending duodenum, the papilla was located and deep cannulation achieved, and a diagnostic cholangiogram was obtained. Sphincterotomy was done according to guidelines 17 by pull spinchterotomy knife, or by needle-knife. The sphincter muscle was cut at the ampulla with a unipolar blended current. The landmark that helps determine the safe extent of the cut is the intraduodenal portion of the common bile duct. The incision of the sphincterotomy stops when it reaches the transverse fold located to the upper part of papilla. Within the zone from 11:00 a.m. to 1:00 p.m. The cut is performed with short bursts of current. The size of the sphincterotomy generally from 1.5 to 2.5 cm is determined by the therapeutic objectives. If one or more stones are identified in bile, stones are removed by means of baskets, balloon-tipped catheters, or both. ENBD is placed in bile and vacuum suction will be connected for 7 d, then ENBD is removed. After operation, the same drugs should be administrated. Observe abdominal pain and sign, and recheck blood and urine amylase everyday. Endoscopic naso-pancreatic drainage (ENPD) would be undergone in case of noneffective ENBD. Disappearance of fluid in mild acute pancreatitis, and decrease of fluid in severe acute pancreatitis (Balthazar CT grades go down one grade or more) can be detected by CT.
Put all data into SPSS computer system. The qualitative data are done by the χ2 method, the quantity data are expressed as mean±SD, and t test is used. The significance level is set at 0.05 for each analysis.
The ratio of success of diagnostic cholangiograms done by cannulation or pull-spinchterotomes knife is up to 91.11% (41/45). After diagnostic cholangiogram, sphincterotomy is done by pull-spinchterotomes knife. In the rest of the four cases, the papilla is straightly dissected by the needle knife, then sphincterotomy is done according to guidelines17 by means of pull spinchterotomy knife for two patients, and for the other two patients ,the papilla is pre-cut by pull-spinchterotomes knife, then enlarged. EST was achieved in 100% patients in EST group. Among 45 cases under the treatment of EST+ENBD, 1 patient with continued abdominal pain received ENPD in 2 wk and then felt painless.
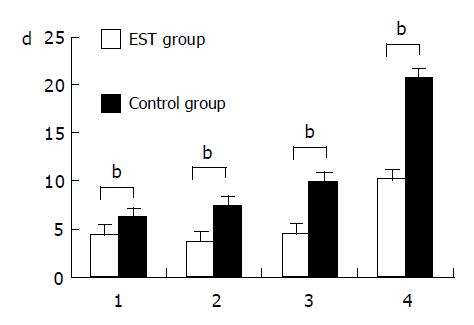
Compared with the control group, the days of disappearance of abdominal pain, the days of normalization of blood and urine amylase and the hospitalization are significantly shorter in the EST group than that in the control group (P<0.001), particularly, the time of normalization of amylase and hospitalization are 0.5-fold shorter in EST group than in control group (Figure 1).
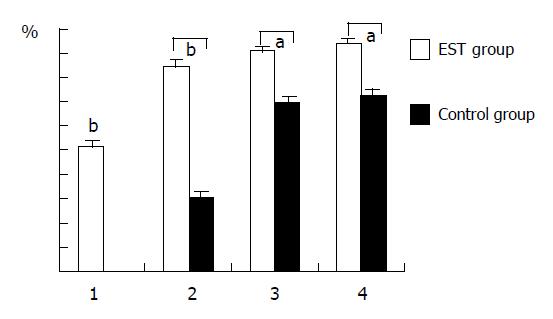
In EST group, the rate of pancreatic fluid disappearance in mild acute pancreatitis is 51.52% for the 1st wk, 84.85% for the 2nd wk, 90.91% for the 3rd wk and 93.94% for the 4th wk checked by B ultrasonography. But the rate of pancreatic fluid disappearance in control group is 0% for the 1st wk, 30.30% for the 2nd wk, 69.70% for the 3rd wk and 72.73% for the 4th wk. EST group is superior to control group (P<0.01 or P<0.05) (Figure 2).
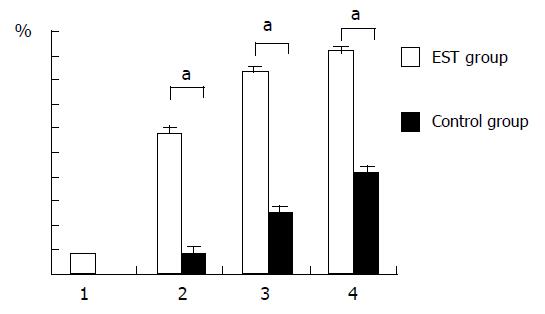
The pancreatic fluid collection remission rate in severe acute pancreatitis is 8.33%, 58.33%, 83.33% and 91.67% respectively for the 1st, 2nd, 3rd, 4th wk after EST. But it is 0%, 8.33%, 25% and 41.67% for the 1st, 2nd, 3rd, 4th wk in control group. The pancreatic fluid collection remission rate after 2 wk is significant difference between two groups (P<0.05) (Figure 3).
Pancreatitis is often caused by gallstone, alcohol, diet, gastroenteritis, wound and so on. The activation of trypsinogen to trypsin within acinar cells is the initial step in the pathogenesis of acute pancreatitis. Trypsin, in turn, converts a variety of proenzymes into active enzymes, pancreatic and peripancreatic tissue will be autodigested. It is a type of chemical inflammation. Acute pancreatitis is characteristic of interstitial edema associated with inflammatory exudation or necrosis. If the pancreatic duct is involved and pancreatic fluid could not drain unobstructed, it could induce pancreatic duct dilatation and severe disruption. Pancreatic fluid exudation will stimulate peritoneum, and then inflammatory exudation accumulate and form pancreatic fluid. Pancreatic fluid accumulate in pancreas or spread to peripancreatic spaces. The shape and size of pancreatic fluid are different in different anatomic locations, and Siegelman[4] called it acute fluid collection (AFC) in 1980. The international pancreas conference accepted AFC in 1992.
AFC can occur in mild or severe acute pancreatitis. The incidence of AFC is lower in mild acute pancreatitis whose Balthazar CT grades is B or C and AFC is limited. Our data show that EST+ENBD treating mild acute pancreatitis associated with AFC can shorten AFC absorbing time significantly. In some cases the AFC disappeared within 1 wk, while in most cases it disappeared within 2 wk. The incidence of AFC is higher in severe acute pancreatitis whose Balthazar CT grades is D or E and the AFC area is more extensive, commonly with abdominal cavity free fluid. Compared with control group, EST+ENBD greatly shortens the AFC absorbing time, and the AFC alleviated 2 wk later. So we can know it is effective that EST treats mild or severe pancreatitis. The possible mechanism is as follows: (1) pancreatic fluid collection may communicate with small pancreatic duct[5,6] . Once sphincterotomy is done, pancreatic and biliary fluid can drain unobstructively, the intraductal pancreatic pressure will lessen and fluid will be absorbed quickly; (2) After sphincterotomy is done, the pathogeny of pancreatitis disappears, pancreatic exudation is reduced and fluid will also be absorbed quickly.
In a majority of pancreatitis cases including non-biliary acute pancreatitis, EST can alleviate the patients’ clinical symptoms, assays and fluid collection. The reason could be: (1) many cases of non-biliary pancreatitis are caused by gallstones or cholesterol crystal too small to be visualized by abdominal ultrasonography or CT[7-9], actually those cases are biliary pancreatitis so the effect of EST is very evident; (2) duodenal papilla edema, oddi sphincter jerking bile and pancreatic fluid draining obstruction exist in any type of pancreatitis, all of which can aggravate pancreatitis and reduce inflammation permeance absorption. But after EST+ENBD, Oddi sphincter jerking disappears, bile and pancreatic fluid drains unobstructedly, ENBD makes drainage more fluent so intraductal pancreatic pressure is lessened, pancreatic fluid and AFC can be absorbed more quickly. In EST group when sphincterotomy is done we can see through endoscope that lots of exiguous solid matter and bile effused. It reveals that pancreatitis is associated with the common channel obstructing. If ERCP shows that the pancreatic duct is obstructed or the effect of EST is not good, it is necessary that endoscopic naso-pancreatic drainage (ENPD) is carried out.
Most authors[10-13]claim that the effect of early endoscopic sphincterotomy in treating patients with severe acute pancreatitis is good in spite of etiology. But in our data, those patients are mostly transferred from grass-rooted hospitals to our hospital, the course of diseases are more than 72 h delayed, but this trial shows that delayed EST+ENBD can relieve pancreatitis quickly and accelerate amylase normalization. The mechanism may be that EST can relieve the pathogeny which may induce continued injury.
Take patients with acute pancreatitis with fluid for example, their duodenal papilla has edema and deviated from normal location so we cannot make sure the direction of cannulation. When gallstones impacted in the ampulla of Vater, the duodenal papilla looks like an elliptoid ball whose hatch is downward; the location of the papilla is difficult to adjust and the deep cannulation or pull-spinchterotomes knife cannot achieve easily, so the papilla is dissected using a straight needle knife, and the operation is more risky. ENBD can prevent recurrence of complications. So ENBD can not only accelerate bile fluid and remnant stones draining unobstructively but also reduce the risk of EST[14].
Science Editor Wang XL Language Editor Elsevier HK
| 1. | Bradley EL. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1929] [Cited by in RCA: 1735] [Article Influence: 54.2] [Reference Citation Analysis (1)] |
| 2. | Safrany L. Duodenoscopic sphincterotomy and gallstone removal. Gastroenterology. 1977;72:338-343. [PubMed] |
| 3. | Leese T, Neoptolemos JP, Carr-Locke DL. Successes, failures, early complications and their management following endoscopic sphincterotomy: results in 394 consecutive patients from a single centre. Br J Surg. 1985;72:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 153] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Siegelman SS, Copeland BE, Saba GP, Cameron JL, Sanders RC, Zerhouni EA. CT of fluid collections associated with pancreatitis. AJR Am J Roentgenol. 1980;134:1121-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 158] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Tsiotos GG, Sarr MG. Management of fluid collections and necrosis in acute pancreatitis. Curr Gastroenterol Rep. 1999;1:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Espinel J, Jorquera F, Fernández-Gundín MJ, Muñoz F, Herrera A, Olcoz JL. Endoscopic transpapillary drainage of an infected pancreatic fluid collection in pancreas divisum. Dig Dis Sci. 2000;45:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Kaw M, Brodmerkel GJ. ERCP, biliary crystal analysis, and sphincter of Oddi manometry in idiopathic recurrent pancreatitis. Gastrointest Endosc. 2002;55:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | van Brummelen SE, Venneman NG, van Erpecum KJ, VanBerge-Henegouwen GP. Acute idiopathic pancreatitis: does it really exist or is it a myth? Scand J Gastroenterol Suppl. 2003;239:117-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Coyle WJ, Pineau BC, Tarnasky PR, Knapple WL, Aabakken L, Hoffman BJ, Cunningham JT, Hawes RH, Cotton PB. Evaluation of unexplained acute and acute recurrent pancreatitis using endoscopic retrograde cholangiopancreatography, sphincter of Oddi manometry and endoscopic ultrasound. Endoscopy. 2002;34:617-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 96] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Scheurer U. Acute pancreatitis--ERCP/endoscopic papillotomy (EPT) yes or no? Swiss Surg. 2000;6:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Hammarström LE, Stridbeck H, Ihse I. Endoscopic drainage in benign pancreatic disease: immediate and medium term outcome. Eur J Surg. 1997;163:577-589. [PubMed] |
| 12. | Neoptolemos JP, London N, Slater ND, Carr-Locke DL, Fossard DP, Moosa AR. A prospective study of ERCP and endoscopic sphincterotomy in the diagnosis and treatment of gallstone acute pancreatitis. A rational and safe approach to management. Arch Surg. 1986;121:697-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 53] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Hsu RK, Draganov P, Leung JW, Tarnasky PR, Yu AS, Hawes RH, Cunningham JT, Cotton PB. Therapeutic ERCP in the management of pancreatitis in children. Gastrointest Endosc. 2000;51:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Sharma BC, Agarwal DK, Baijal SS, Saraswat VA, Choudhuri G, Naik SR. Endoscopic management of acute calculous cholangitis. J Gastroenterol Hepatol. 1997;12:874-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |