Published online May 14, 2005. doi: 10.3748/wjg.v11.i18.2781
Revised: October 24, 2004
Accepted: December 1, 2004
Published online: May 14, 2005
AIM: The molecular diagnosis of microsatellite instability (MSI) in colorectal cancer (CRC) is based on the analysis of five microsatellite markers. Among them, the two mononu-cleotide microsatellite repeats are considered more infor-mative for this analysis than the three dinucleotide ones. The aim of this study is to establish the most relevant markers for MSI analysis in colorectal cancers from Asian patients.
METHODS: The MSI analysis of 143 CRC cases in a routine molecular diagnostic laboratory was reviewed. Analysis by fluorescence-based PCR of the five recommended micros-atellites was performed, followed by data interpretation according to internationally accepted guidelines. The results were analyzed to address (1) the rate of success in the analysis of histopathological samples not specifically prepared for molecular analysis; (2) the relative importance of individual markers in the diagnosis of high-MSI (H-MSI).
RESULTS: MSI analysis was unsuccessful in 34 cases (24%), but for tissues archived in recent years the unsuccessful rate was 5%. We found the D2S123 marker the most vulnerable to inadequate tissue preservation, failing to amplify in 58 instances. Approximately 30% (32/109) of the cases were H-MSI, while 7/109 (6%) were low-MSI. A detailed analysis of the H-MSI cases revealed that the dinucleotide repeats (and D5S346 in particular) were more relevant than the mononucleotide repeats in assigning the correct MSI status.
CONCLUSION: The analysis of dinucleotide repeats is essential for the establishment of MSI status in Asian CRC patients.
- Citation: Salto-Tellez M, Tan SY, Chiu LL, Koay ESC. Dinucleotide microsatellite repeats are essential for the diagnosis of microsatellite instability in colorectal cancer in Asian patients. World J Gastroenterol 2005; 11(18): 2781-2783
- URL: https://www.wjgnet.com/1007-9327/full/v11/i18/2781.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i18.2781
The diagnosis of microsatellite instability (MSI) in colorectal cancer (CRC) is based on the molecular analysis of five microsatellite markers, including two mononucleotide repeats (Bat-25 and Bat-26) and three dinucleotide repeats (D2S123, D5S346 and D17S250)[1]. However, it has been argued that the analysis of a single mononucleotide repeat such as Bat-26[2] may be sufficient for this purpose. Furthermore, the comparison of the five microsatellites in hereditary non-polyposis colorectal cancer (HNPCC)-proven cases has highlighted the higher informativity[3] of mononucleotide repeats for this analysis.
In a recent report[4], based on a limited number of 27 patients, we suggested that the dinucleotide markers were the most frequently unstable and the most relevant ones for the diagnosis of MSI. To fully confirm or refute this fact, we reviewed all the MSI analyses on CRC cases performed in the Molecular Diagnosis Centre at the National University Hospital of Singapore since the establishment of the test 3 years ago.
A total of 143 cases were analyzed. The mean age of the patients was 46 years. These were cases referred to our laboratory because of clinical features that required the consideration of the HNPCC syndrome, following the Amsterdam criteria.
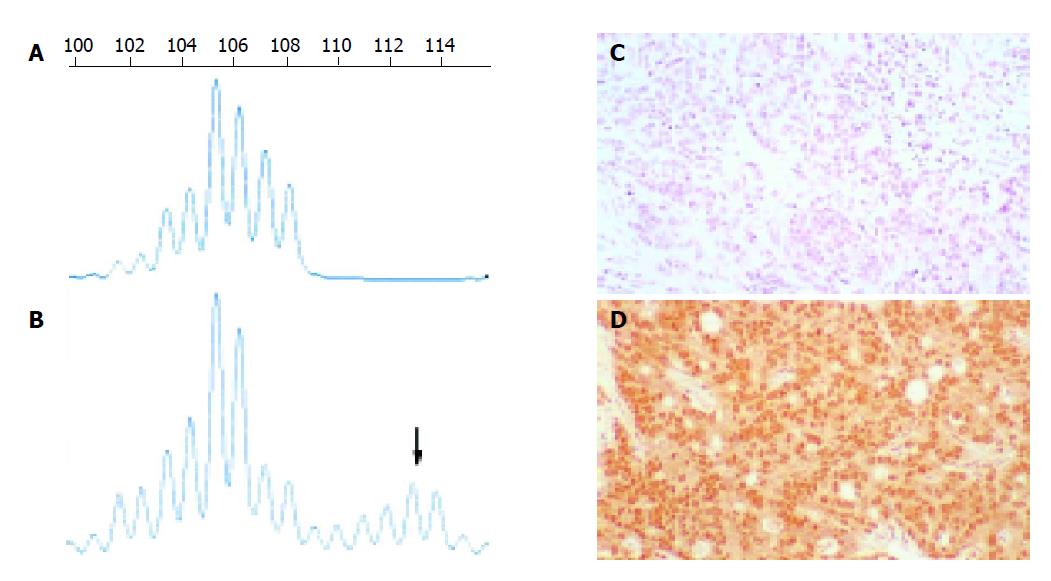
The analysis was done as reported elsewhere[3,4]. Briefly, CRC tissue and normal colonic mucosa were manually microdissected. DNA was extracted with the DNeasyTM Tissue Kit (Qiagen GmbH, Hilden, Germany), according to the manufacturer’s instructions. This was followed by a capillary electrophoresis, fluorescence-based PCR analysis of the five microsatellite repeats mentioned above, namely Bat-25 (4q12-c-kit), Bat-26 (2p16.3-hMSH2), D2S123 (2p16-hMSH2), D5S346 (5q21-APC), and D17S250 (17q11.2-BRCA1). A subset of those cases with positive results was subjected to immunohistochemical staining with hMSH2 and hMLH1 antibodies, as well as sequencing of the hMSH2 and hMLH1 genes[4]. An example of microsatellite analysis and mismatch repair gene immunohistochemistry is shown in Figure 1.
The criterion for high MSI status (H-MSI) is based on instability in at least two microsatellite markers. Instability of a single marker represents low microsatellite instability (L-MSI). Cases with no evidence of instability in any of the markers are considered microsatellite stable (MSS). In view of this, cases with successful PCR amplification in only 2, 3 or 4 markers, and with instability in at least two of those markers, were considered H-MSI; cases with unsuccessful PCR amplification in one or more microsatellites and one or no unstable markers in the successful ones, were regarded as “unsuccessful” analyses, as in these cases we would not be able to exclude L-MSI or H-MSI status.
With these criteria in mind, a total of 109 successful cases were analyzed (76%), while 34 (24%) unsuccessful cases were excluded. This apparently high percentage of unsuccessful cases was directly related to the age of the paraffin blocks: in fact, the bulk of the unsuccessful cases had paraffin blocks of more than 5 years of age (and sometimes up to 19 years old), at a time when fixation and embedding conditions were not so critically controlled to maintain full nucleic acid preservation. In those cases from recent years, from our own laboratories, where an adequate control in fixation was exercised (10% buffered formalin during a tightly controlled fixation period of 12-24 h), the success rate was 95% (61/64 cases).
Approximately 30% (32/109) were H-MSI, while 7/109 (6%) were L-MSI. Lack of PCR amplification was noted with the following frequency: Bat-25-10/143 (7%); Bat-26-28/143 (19%); D2S123-58/143 (40%); D5S246-13/143 (9%); and D17S250-26/143 (18%). As unsuccessful amplification was noted predominantly in those cases with older blocks and poor DNA preservation, this analysis gives an indication of the resistance or vulnerability of specific microsatellites to DNA degradation. It appears clear that D2S123 is the most vulnerable, while Bat-25 and D5S346 are the most resistant. This can only be explained in part by the size of the amplicon; indeed, D2S123 is vulnerable as it has the largest PCR product, but does not explain the fact that Bat-26 and Bat-25, with a narrow base-pair difference of 4 units, have a significant difference in outcome. As suggested elsewhere[5], PCR re-design may be important in narrowing down these differences when looking at paraffin-embedded samples with potential DNA degradation.
To analyze the “diagnostic importance” of each individual marker, we looked at the 13 H-MSI cases in which the diagnosis was made because the minimum number of markers (2) was unstable (Table 1). In these cases, the exclusion of one of those markers would have rendered a different diagnosis altogether. The frequency of instability in these cases for each individual marker is: Bat-25-7 cases; Bat-26-3 cases; D2S123-3 cases; D5S346-8 cases; D17S250-5 cases. Thus, it appears that the dinucleotide repeats are at least as relevant as the mononucleotide repeats for the analysis of H-MSI in these cases; in particular, D5S346 seems to be the most frequently unstable marker. Furthermore, 10/13 cases in this series show no Bat-26 instability.
| S/N | Results | Status | ||||
| Bat-25 | Bat-26 | D2S123 | D5S346 | D17S250 | ||
| 1 | - | - | - | + | - | H-MSI |
| 7 | - | - | - | + | + | H-MSI |
| 31 | - | - | + | - | + | H-MSI |
| 34 | - | - | + | - | + | H-MSI |
| 41 | - | - | - | + | + | H-MSI |
| 56 | + | + | - | - | - | H-MSI |
| 58 | - | - | + | + | - | H-MSI |
| 87 | - | + | - | + | - | H-MSI |
| 95 | + | - | - | - | + | H-MSI |
| 103 | + | - | - | + | - | H-MSI |
| 106 | + | - | - | + | - | H-MSI |
| 110 | + | - | - | + | - | H-MSI |
| 140 | + | + | - | - | - | H-MSI |
This analysis allows some conclusions in the application of MSI analysis in Asian patients. Firstly, they confirm that analysis of Bat-26 alone may not be sufficient to establish the MSI status in CRC[6]. Secondly, it highlights the importance of the inclusion of dinucleotide repeats in the MSI analysis of Asian patients. The relevance of dinucleotide repeats in our patient population is a fact difficult to explain. Comparative studies of microsatellite polymorphisms in different ethnic populations have shown a difference[7] that perhaps may be applicable to Asian patients as well. Also, the relevance of mononucleotide repeats in MSI analysis was generally calculated taking HNPCC-proven patients as the gold standard. With the increasing evidence that the MSI status may be useful in establishing the prognosis of H-MSI, sporadic CRC patients[8,9], the clinical importance of individual MSI markers may have to be redefined.
In conclusion, dinucleotide repeats are essential for the establishment of MSI status in Asian CRC patients. In general, a comparative analysis of the relevance of microsatellites in different ethnic populations, and in both HNPCC and H-MSI sporadic CRC patients, may be of importance when applying this test in the future for both HNPCC diagnosis and CRC prognostication.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58:5248-5257. [PubMed] |
| 2. | de la Chapelle A. Testing tumors for microsatellite instability. Eur J Hum Genet. 1999;7:407-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Berg KD, Glaser CL, Thompson RE, Hamilton SR, Griffin CA, Eshleman JR. Detection of microsatellite instability by fluorescence multiplex polymerase chain reaction. J Mol Diagn. 2000;2:20-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 119] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Salto-Tellez M, Lee SC, Chiu LL, Lee CK, Yong MC, Koay ES. Microsatellite instability in colorectal cancer: considerations for molecular diagnosis and high-throughput screening of archival tissues. Clin Chem. 2004;50:1082-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Umetani N, Sasaki S, Watanabe T, Ishigami H, Ueda E, Nagawa H. Diagnostic primer sets for microsatellite instability optimized for a minimal amount of damaged DNA from colorectal tissue samples. Ann Surg Oncol. 2000;7:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Loukola A, Eklin K, Laiho P, Salovaara R, Kristo P, Järvinen H, Mecklin JP, Launonen V, Aaltonen LA. Microsatellite marker analysis in screening for hereditary nonpolyposis colorectal cancer (HNPCC). Cancer Res. 2001;61:4545-4549. [PubMed] |
| 7. | Pyatt R, Chadwick RB, Johnson CK, Adebamowo C, de la Chapelle A, Prior TW. Polymorphic variation at the BAT-25 and BAT-26 loci in individuals of African origin. Implications for microsatellite instability testing. Am J Pathol. 1999;155:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Hemminki A, Mecklin JP, Järvinen H, Aaltonen LA, Joensuu H. Microsatellite instability is a favorable prognostic indicator in patients with colorectal cancer receiving chemotherapy. Gastroenterology. 2000;119:921-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 253] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 9. | Ribic CM, Sargent DJ, Moore MJ, Thibodeau SN, French AJ, Goldberg RM, Hamilton SR, Laurent-Puig P, Gryfe R, Shepherd LE. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med. 2003;349:247-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1585] [Cited by in RCA: 1634] [Article Influence: 74.3] [Reference Citation Analysis (0)] |